Trauma, Burns, and Bites
Robert P. Foglia
Between age 1 month and 18 years, one half of all deaths in children are the result of a traumatic injury. Trauma accounts for more deaths in children in this age range than all forms of cancer, heart disease, and infections combined. The objectives of this chapter will be to review the differences between adults and children in regard to mechanism of injury and physiologic response; discuss pathophysiology and the initial management of the trauma victim; and outline common injuries involving various organ systems.1-16
CHILDHOOD TRAUMA
The often invoked axiom that children, and especially infants and young children, are not small adults applies also to understanding and treating traumatic injuries. The differences involve anatomical and physical characteristics, physiological and psychological responses, and even the very mechanisms by which trauma occurs. Adult practitioners often need to be reminded that, for instance, children have greater surface ratio of area to mass than do adolescents or adults. This results in greater dissipation of heat and water, which may compound the effects of other traumatic injuries. The child’s skeleton exhibits greater elasticity than the adult’s and is therefore more likely to allow compression and visceral injury without fractures. A vast majority of childhood injuries are passive and result from blunt trauma and thus tend to involve multiple organs. Yet, children tend to experience better outcomes compared to the adult with the same mechanism of injury because of factors such as the occurrence of fewer bone fractures and the lack of comorbid disorders. Yet, it is important to remember that, while a recovery of function and quality of life after blunt injury is common, physical function tends to remain lower than age-matched norms at 6 months postinjury, and often the childhood trauma victim and his or her family bears the consequence of that injury for a lifetime.
TRAUMA SCORES
A common language that describes injuries and their consequences is very useful in the frenzied circumstances that are the norm in the trauma management process. The Glasgow Coma Scale (GCS, see Chapter 104) and Injury Severity Scale (ISS) have been mainstays in the assessment and subsequent review of outcomes in pediatric trauma patients. The New Injury Severity Score (NISS) has been shown to have an improved predictive value in adult trauma victims compared to the ISS, but this superiority has not been corroborated in children. Likewise, trauma scores specifically designed for children have not been found to be superior to trauma scores in general.
TRAUMA MANAGEMENT
The evaluation and management of the injured child is best performed using a standard protocol. The Advanced Trauma Life Support (ATLS) protocol is widely used and establishes three sequential events: the primary survey, the secondary survey, and a definitive care phase.
 PRIMARY SURVEY
PRIMARY SURVEY
The primary survey is performed in the first several minutes. Seminal to this phase is the rapid assessment of vital functions followed by the appropriate resuscitation measures.
The presumption that every patient may have suffered a cervical spine injury has become integral to initial trauma management. Cervical stabilization is thus one of the first steps of the stabilization and is continued until cervical injury can be adequately excluded. Immobilization of the cervical spine is usually carried out by prehospital personnel and can be achieved with appropriately sized Philadelphia or Aspen collars or by using sandbags on either side of the head and applying tape over the sandbag and the forehead of the patient. A foam cervical collar will not adequately stabilize the neck. A care-giver can stabilize the cervical spine by holding both mastoids and mandibles in a manner that prevents flexion-extension and lateral movements. If the child is awake and cooperative, the absence of pain or other findings upon careful full range mobilization of the neck is usually sufficient to exclude injury. However, physical examination alone cannot exclude a spinal injury in: (1) patients who are uncooperative or unresponsive; (2) the young child unable to give a meaningful or reliable response to questions; or (3) the patient with a significant distracting painful injury elsewhere. Pain with neck movement, tenderness to palpation of the cervical vertebrae, a detectable cervical spine deformity, or a neurologic abnormality referable to the neck are all good reasons to continue immobilization and protection of the cervical spine and to obtain specialized imaging studies and neurosurgical consultation if available.
 ASSESSMENT OF VITAL FUNCTIONS
ASSESSMENT OF VITAL FUNCTIONS
In children inadequate oxygenation and ventilation are the more common causes of arrest after trauma. For this reason, primary attention must be directed toward assessing airway patency and the efficiency of breathing effort. In every case, the mouth should be opened and the pharynx examined for foreign material or loose teeth. Secretions should be cleared and, if the child is unconscious, a jaw thrust maneuver or insertion of an oral airway may be used to prevent upper airway obstruction. Supplemental oxygen should be instituted. The presence of persistent respiratory distress or insufficient respiratory effort is usually an indication for tracheal intubation, which should be performed by the most experienced individual. If it is difficult to establish a patent airway, a needle cricothyroidotomy can provide rapid stabilization. A tracheostomy attempted outside of the operating room, particularly in a small child, can be a very difficult procedure, and is not the treatment of choice in this situation. Bag and mask ventilation can often provide adequate ventilation even in the most difficult circumstances and is preferable to unskilled tracheal intubation, particularly if laryngeal or tracheal injuries are suspected.6
If the patient has a suspected injury and no stridor but apparent upper airway obstruction, after several unsuccessful attempts of endotracheal intubation, a cricothyroidotomy is the next step. In the circumstance where there is a suspected laryngeal crush injury and stridor, consideration should be given to proceeding directly to a cricothyroidotomy without attempted endotracheal intubation because of the risk of creating a false passage in placing the airway via an endotracheal route.
After airway patency is assured, attention should move to other aspects of the breathing function (see Chapter 102). Palpation and auscultation are used to determine whether the trachea is in the midline. If it is, breath sounds can be heard well bilaterally. A tracheal shift or a decrease of breath sounds on one side of the chest may indicate a pneumothorax or hemothorax (the tracheal will deviate to the side opposite to the shift). If the patient is stable, a chest radiograph should be obtained to establish the origin of the findings.
If there is a tension pneumothorax, urgent treatment is indicated. This can be carried out by simply placing a needle into the pleural space through the second intercostal space at the midclavicular line. This allows relief of the tension and provides an opportunity to place a chest tube for continued evacuation of air. Chest tube placement or tube thoracostomy is the appropriate treatment for a traumatic accumulation of gas or liquid in the pleural space. In a small infant, a 12 to 14 French chest tube is appropriate. In an older child, an 18 to 24 French chest tube is preferable. A larger bore chest tube is more appropriate if a hemothorax is suspected. 
A child with several contiguous rib fractures may have a flail chest, a condition characterized by a paradoxic inward movement of a portion of the chest during inspiration. This reduces both the functional residual capacity and the tidal volume, almost always requiring positive pressure ventilation. A sucking chest wound involves a penetrating injury that allows air to enter the chest during inspiration. The resulting pneumothorax can be prevented from becoming larger by placing a flap valve dressing over the injury until a chest tube can be inserted and the chest wall can be subsequently repaired.
An often overlooked reason for respiratory dysfunction after trauma is equipment failure. Worsening respiratory function can not infrequently be traced to kinking, disconnection or obstruction of an endotracheal tube, or insufficient suction on a chest tube. The importance of surveying the life support equipment frequently and thoroughly cannot be overemphasized, especially when a child experiences an unexplained worsening.
The next step in the primary survey is assessing the adequacy of tissue perfusion (see Chapter 103). A number of physical signs can reflect inadequate perfusion including tachycardia, pallor, cool extremities, confusion, combativeness, or a decreased blood pressure. After hemorrhage, blood pressure is usually maintained until the child loses 20% of his or her blood volume; thus, hypotension is a late manifestation of a significant injury. Checking the capillary refilling time provides a quick assessment of perfusion, provided that the patient is not cold.
Completion of the primary survey requires an assessment of neurologic function. It is particularly important to establish at this point whether the child has any lateralizing neurological signs that suggest an intracranial space-occupying lesion or spinal cord injury.
 INTRAVENOUS ACCESS
INTRAVENOUS ACCESS
Adequate venous access is essential for the treatment of traumatic injuries. It has become the norm that any child with a significant traumatic injury should have two intravenous lines. If there is an injury involving the abdomen then at least one of the intravenous lines should be in an upper extremity or neck. Attempts should first be made to place intravenous lines percutaneously, although this may be challenging in the young child, particularly if hypovolemic. In such conditions, successful placement of a small bore intravenous line may gain precious time for the initial resuscitation. A larger gauge catheter can be inserted then under less pressing circumstances. If peripheral intravenous access cannot be achieved within several minutes, alternative methods of access should be attempted (see Chapter 107), including intraosseous access and, if skilled personnel are available, insertion of a central venous catheter either percutaneously or by surgical venotomy.
After vascular access is established, fluid resuscitation can be initiated accompanied by frequent reassessment of hemodynamic function (heart rate, blood pressure, state of alertness, capillary refill). A urinary catheter should be placed in a major trauma patient.
 SECONDARY SURVEY
SECONDARY SURVEY
The secondary survey includes a history and a complete head to toe examination of the child with a focus on specific organ systems. The mnemonic AMPLE stands for obtaining a history in regard to Allergies, Medications, Past illnesses, Last meal, Events, and Environment involved with the injury. In the secondary survey the evaluation, testing, and interventions should be individualized for each patient. Every part of the body should be palpated, the chest and abdomen should be auscultated and the patient “log rolled” to examine the back and to perform a rectal examination.
Head and Neck
The assessment and management of acute neurological injuries are discussed in Chapters 104 and 111. Inspection and palpation of the head focuses on the detection of eye and ear injuries, and craniofacial fractures. Crepitus usually indicates a communication between the sinuses and the subcutaneous tissue through a facial bone fracture. Tenderness over the maxilla, and mandible, and malocclusion also indicate facial bone fractures. Rhinorrhea or otorrhea suggest a spinal fluid leak through a base of the skull fracture.
Examination of the neck and cervical spine includes palpation to identify tenderness, mobilization to assess range of motion, a motor and sensory examination, evaluation of reflexes, and appropriate imaging studies. Difficulty in carrying out this examination is most commonly the result of an altered level of consciousness and/or lack of ability to cooperate because of the patient’s age, or the distracting effects of other injuries. Signs of airway obstruction, hoarseness, stridor, crepitus, or significant soft tissue swelling are alerts for a possible airway injury.
In patients who have undergone stabilization of the neck with a collar, examination of the cervical spine requires the removal of the collar. This may not be appropriate in patients who are unconscious or uncooperative. After inspecting for injury, the cervical spine is palpated. If there is pain on palpation or if there is a deformity or swelling, the cervical collar is re-applied and an imaging study should be performed. If no abnormality on examination is noted and no pain elicited, the patient is asked to rotate the head and neck to each side, move it laterally, and then flex and extend it. If movement is limited or pain occurs, the collar is re-applied and imaging studies are indicated. If again no pain or abnormality is noted, the patient’s cervical spine has been “cleared” and no diagnostic imaging is needed. The decision process is more difficult, if for any reason, usually loss of consciousness or lack of cooperation, the cervical spine cannot be “cleared” in this manner. Computerized tomography (CT) examination provides a practical method to assess for neck injuries in children. A combined head and neck CT scan will, in the right circumstances, decrease the number of studies that a child will eventually undergo. It is important to recognize, however, that a normal neck CT scan does not eliminate the need to perform a functional examination of the neck once it is possible to obtain patient cooperation.
Chest
More than 80% of thoracic injuries in children are caused by blunt trauma. The incidence decreases to slightly less than 60% in adolescents. In the patient with blunt chest injuries, the most common cause of death is a head injury; in patients with penetrating chest injury, the death is most often caused by the chest injury itself.
The majority of thoracic injuries can be handled well with supplemental oxygen, tube thoracostomy, and analgesia. Approximately 5% to 10% of all blunt chest injuries may require a thoracotomy. Immediate life-threatening conditions include complete airway obstruction, tension pneumothorax, massive hemothorax, cardiac tamponade, and penetrating cardiac injury. Also potentially life-threatening conditions include pulmonary contusion, myocardial contusion, aortic disruption, diaphragmatic rupture, tracheobronchial disruption, and esophageal perforation. Indications for emergency thoracotomy include a penetrating wound to the heart or aorta, continued significant intrathoracic bleeding from other source (≥ 3–4 mL/kg/hour), an imaging study indicating an injury to the aorta or other large vessel, a pneumothorax with an open chest wall injury, a large continuing air leak indicative of a bronchial injury, cardiac tamponade, impalpable pulses with closed chest compression, diaphragmatic rupture, and esophageal perforation.
Abdomen
The secondary survey of the abdomen includes inspection, palpation, percussion, auscultation, and the use of imaging studies as needed. Abdominal blunt trauma carries an increased risk of injuring multiple organs. The presence of a “seat belt” sign, a linear abdominal wall ecchymosis, is indicative of a rapid deceleration mechanism of injury. This deceleration can often cause significant intra-abdominal injuries. The combination of a seat belt injury and significant tenderness on palpation should cause a high degree of suspicion for injuries of the abdominal viscera.
The abdominal plain film may show evidence of inferior rib fractures, vertebral anomalies, a pelvic fracture, and an abnormal bowel gas pattern. A nasogastric tube should be placed to decompress the stomach if distended. If there is any evidence of a mid-face fracture, the tube should be placed via an orogastric route to avoid the possibility of the tube being misplaced into the cranial cavity. Urethral injury is common in males and should be suspected if there is blood in the urethral meatus or a high riding prostate on rectal examination. If there is a significant suspicion to a urethral injury, a retrograde urethrogram should be performed before inserting a Foley catheter.
The presence of a pelvic fracture should raise suspicions of a concomitant retroperitoneal or urethral injury. Contemporary evaluation of the abdomen often includes an abdominal and pelvic computerized tomography scan. With the new generation of helical scanners, a full abdominal examination can be carried out in minutes. Radiological assessment should only be performed, however, once the patient is sufficiently stable. Peritoneal lavage is now used in very limited circumstances, because the presence of free blood in the abdominal cavity is no longer considered an automatic indication for surgery.
The spleen and the liver are two of the abdominal organs most commonly injured. The conservative management of childhood splenic and liver injuries is common practice today. A retrospective study of 440 patients from 17 pediatric trauma centers who had isolated splenic injuries showed that only 4% required surgery.12 Large multi-institutional studies have shown that children with isolated splenic or hepatic injuries (Grades I–III) injuries typically do not require admission to the intensive care unit (ICU), infrequently require blood transfusion, and, in their majority, can be managed nonoperatively. Indications for surgery include a persistently low hemoglobin unresponsive to blood transfusion, or hemodynamic instability unresponsive to fluid resuscitation.
Injuries to the pancreas are often the result of a blunt injury, such as those caused by the handlebar of a bicycle, a rapid deceleration injury in a motor vehicle accident, a fall, or intentional child abuse. Because of the location of the pancreas, there are often coexisting injuries to the stomach, duodenum, kidneys, or spine. The diagnosis is made on the basis of laboratory studies (elevation in amylase and lipase) and imaging studies (a CT scan demonstrating pancreatic edema, hematoma, or disruption). A penetrating injury of the abdomen with a pancreatic injury requires laparotomy. A blunt injury with stable vital signs and no peritonitis can usually be managed nonoperatively. The decision to operate is usually prompted by the persistence of fever, pain, ileus, and hyperamylasemia. Treatment otherwise consists of bowel rest, intravenous nutrition, and administration of octreotide to decrease pancreatic exocrine secretions. A pancreatic pseudocyst is a known complication of pancreatic trauma, often associated with an elevation in lipase and amylase. The pseudocyst is initially managed nonoperatively. Many of these will decrease spontaneously in size and resolve. If the pseudocyst if still present for over six weeks, consideration should be given to internal drainage, a cystgastrostomy, or drainage into the bowel depending upon the location of the pseudocyst (see Chapter 417).
Intestinal injuries can occur throughout the large or small bowel. The ligament of Treitz and the ileocecal valve are the two most vulnerable points because shear forces tend to tear the bowel at its tethering points to the abdominal wall. The duodenum, on the other hand, is often injured when compressed between the abdominal wall and the spine. A duodenal hematoma can be diagnosed by an upper GI contrast study or an abdominal CT scan. Management is nonoperative, and in approximately 85% of cases the hematoma will resolve spontaneously.
The presence of microscopic hematuria may not require admission if the CT scan of the abdomen shows no abnormalities. An algorithm for management is shown in eFigure 116.1  . If there is microscopic hematuria and a normal CT scan outpatient follow-up is reasonable. An abnormal CT scan or macroscopic hematuria provides indication for hospital admission. If the CT scan shows a major blood extravasation, or nonvisualization of renal flow, arteriography is indicated. If the vasculature is normal, bed rest and observation is reasonable. However, if there is disrupted vasculature, operative intervention is required. Bladder rupture also requires operative intervention.
. If there is microscopic hematuria and a normal CT scan outpatient follow-up is reasonable. An abnormal CT scan or macroscopic hematuria provides indication for hospital admission. If the CT scan shows a major blood extravasation, or nonvisualization of renal flow, arteriography is indicated. If the vasculature is normal, bed rest and observation is reasonable. However, if there is disrupted vasculature, operative intervention is required. Bladder rupture also requires operative intervention.
Child Abuse
This subject is covered more extensively in Section 4. However, in the evaluation of the trauma patient, the suspicion of child abuse should be kept in mind. This is particularly true if any or several of the following are noted: (1) a discrepancy between the history and the degree of injury; (2) a prolonged interval from injury to treatment; (3) a history of repeated similar injuries; (4) an inappropriate parental response; or (5) a changing history given by the caretaker.
 DEFINITIVE CARE
DEFINITIVE CARE
In this phase of care, decisions are made regarding transfer from the Emergency Department to the next site of care. This begins with a reassessment of the patient, review of the need for medications (antibiotics, analgesics, immunizations), further imaging studies, monitoring, and consultation. A comprehensive outline of the status of the patient and the injuries identified is given to the accepting unit in the hospital.
BURNS
Burn injuries are the third most common cause of death due to trauma in children in the United States, accounting for 2500 deaths and over 10,000 cases of severe, permanent disability annually. Many of these injuries are preventable. The majority of pediatric-burn hospital admissions are in children under age 2 years. Burns are often caused by hot liquids in younger children, particularly those under three years of age, and by fire in older children and adults. The initial resuscitation has a fundamental role, particularly in the case of large surface-area burns. The outcome for the burned patient is related to the magnitude of the injury, and is influenced substantially by the quality of the care provided. Patients with significant burn injuries are best cared for in a burn center. Survival rates in pediatric burn victims with 40% to 60% body surface area (BSA) burns have been reported to be as high as 100% and with 60% to 100% BSA burn survival of 86%.17-27
Burns can be categorized as the result of thermal, electrical, chemical, or radiation mechanism. The majority of burns in children have a thermal mechanism. Developmental differences in body surface area to body mass ratio and thickness of the skin account for most differences in the response to a burn injury between infants, children and adults. The child has a larger body surface area (BSA) to body mass ratio in comparison to an adult. A 1 year old weighing 10 kg has one seventh the body mass of an adult and one third the adult’s body surface area. Accordingly, the child has a larger evaporative fluid loss and greater difficulty maintaining temperature regulation. The child’s skin is less thick than the adult’s, and thus can burn more deeply after the same duration of contact with a comparable heat source.
The severity of tissue damage after a burn is related to several factors: (1) temperature of the heat source responsible for the burn; (2) duration of exposure; (3) area of the body burned; and (4) age of the patient. Grease, casseroles, and other hot liquids that tend to stick to the skin, have a longer exposure time, and have the potential to cause a deeper burn than a hot liquid of the same temperature that remains in contact with the skin for a shorter length of time. Burns to the palms of the hand and soles of the feet tend to be less deep than similar burns to other parts of the body because of the relative thickness of the epidermis in those areas. Likewise, while a shoulder burn may require a skin graft because of the depth of burn, a facial burn after a similar exposure may heal spontaneously, because the rich blood supply of the face limits the injury by dissipating heat more rapidly from that area.
DETERMINING BURN SURFACE AND DEPTH
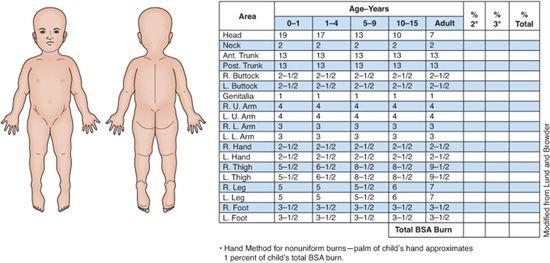
The accurate determination of the burned surface area is an integral part of burn-wound management. In adults, the rule of nines is a simple and accurate way of estimating this surface. Each upper extremity, and each of the anterior or posterior surfaces of the chest, abdomen, and lower extremities represent 9% of the total body surface. Unfortunately, the same rule is not applicable to children. The head and neck of a child less than age 1 year accounts for 21% of the body surface area. The modified Lund-Browder body surface area chart (Fig. 116-1) can be used to estimate the percent of the body surface area involved in a burn. Except in “stocking-glove” type burns that extend from the tip of an extremity to the trunk, it is often necessary to approximate the magnitude of involvement of a body part. Especially in the case of irregular burns, it is also useful to know that the palm of a child represents approximately 1% of the body surface area.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


