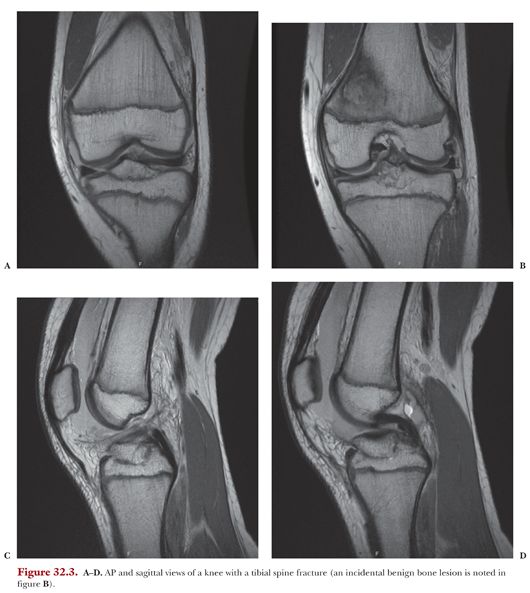
Some may choose to get additional diagnostic studies such as a computed tomography (CT) scan, which has been shown to have some use in better defining fracture characteristics as well as degree of comminution.15 CT studies, however, are not part of the routine workup of tibial spine fractures at our institution. A high rate of concomitant injury with tibial spine fractures has been reported in the literature.16,17 As such, magnetic resonance imaging (MRI) for further radiographic assessment of tibial spine injuries is recommended. MRI is useful in preoperative planning for assessing the structural integrity of the knee and ruling out interstitial injury of the ACL. Furthermore, MRI defines the fracture fragment compared to soft tissue structures (Fig. 32.3). This information is informative regarding potential obstacles to fracture reduction. One prior study reported on the MRI findings associated with tibial spine fractures.16 Associated injuries include intrasubstance ACL and posterior cruciate ligament injuries, medial collateral ligament tears, posterior lateral corner injury, and meniscal tears—specifically meniscal entrapment within the spine fracture segment.
Tibial spine avulsion fractures are most commonly classified based on an algorithm devised by Meyers and McKeevers.18 The classification scheme relies on the degree of displacement of the avulsed fragment from the fracture base. In this fracture scheme, tibial spine fractures are classified from types I to III, with type I being the least displaced and type III the most.
Type I fractures are characteristically nondisplaced fractures of the tibial spine. In type II fractures, the anterior portion of the fracture is displaced superiorly while the posterior portion remains hinged. Type III fractures are completely displaced from the fracture base and are divided into two subcategories: IIIA and IIIB. Type IIIA fractures have complete separation from the fracture base, whereas type IIIB fractures are not only completely displaced but are also rotated cephalad. Zaricznyj19 later added a type IV category which includes displaced fractures with comminution of the fragment.
Although not yet formally described, the authors propose that there is a fifth subset of tibial spine fractures that could be classified as type 0. In type 0, the fractures would not be seen on standard radiographs but could be detectable on MRI.
Tibial spine fracture management is typically based on the type of underlying fracture. These fractures show significant variation in fracture characteristics and associated injury. The common goal, however, is to restore the integrity and function of the ACL as well as to restore the contour of the tibial plateau.
Management of tibial spine fractures is typically operative versus nonoperative. Type I fractures by nature of nondisplacement can be managed nonoperatively with knee immobilization. Adequate immobilization can be obtained with either a brace or a cast. Type I fractures failing nonoperative management typically have late displacement, which can occur despite adequate immobilization. For this reason, patients with type I fractures being managed nonoperatively should be closely monitored for this complication during the first 6 weeks after injury.20 Early motion after evidence of fracture union is important to prevent knee stiffness.
Treatment of type II fractures is more controversial, and historically good results have been reported from both the operative and nonoperative management of type II fractures.21 Similar to type I fractures, mild forms of type II fractures can be managed nonoperatively with cast or knee immobilization if there is near-anatomic reduction. Residual displacement from a malreduced tibial spine fragment leads to lack of full extension and impingement of the displaced tibial eminence in the notch. Soft tissue entrapment within the fracture is the most common etiology for an irreducible fracture. We indicate most type II fractures for arthroscopic fixation to improve reduction, take care of any meniscal entrapment, and promote early ROM.
Advances in arthroscopic techniques have expanded the surgical management of tibial spine fractures. Prior to the widespread use of knee arthroscopy, arthrotomy and open reduction internal fixation of the fracture fragment were the standards of care for types III, IV, and irreducible type II. In the modern era, surgical intervention is the standard of care for types III and IV fractures. Arthroscopy now provides the benefit of decreased morbidity, and as such, the trend is to offer arthroscopic fixation even for type II fractures. Furthermore, arthroscopy allows the surgeon to rule in/out injury to the intra-articular structures under direct visualization.
There are two primary modalities for the surgical management of tibial spine fractures: suture versus screw fixation. In this chapter, we focus on the surgical technique for screw fixation. We use a suture fixation approach for fractures consisting of a small bone fragment or with significant comminution. Both the suture and screw fixation are technically challenging.22 Suture fixation will be further discussed in Chapter 33.
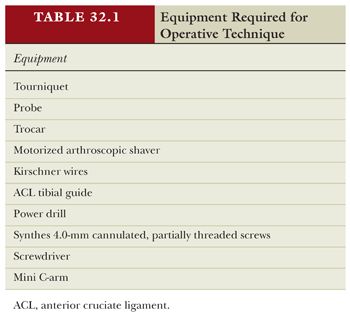
We describe here the authors’ preferred surgical technique for the management of larger sized tibial spine fractures. We present a method for arthroscopic internal fixation using screw fixation (see Table 32.1 for equipment).
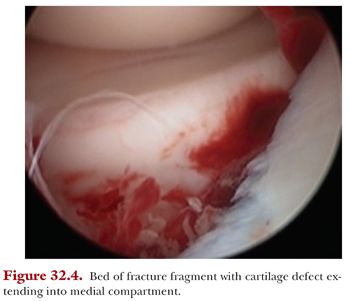
The patient is prepped and draped in the usual sterile fashion in the supine position. A standard anterolateral arthroscopic portal is first established. The arthroscope is introduced via the anterolateral portal and then an anteromedial portal is established under direct visualization from the anterolateral portal. A diagnostic knee arthroscopy is initially performed including the patellofemoral joint and both the medial and the lateral compartments. The presence of a chondral defect is assessed (Fig. 32.4) and the structural continuity of the ACL is determined. The ACL is inspected as is the tibial spine itself. The medial, lateral, and anterior borders of the fragment are evaluated, with particular attention to potential blocks of reduction and extension into the weight-bearing surface of the tibial plateau. Next, the menisci are inspected for involvement of the anterior meniscus in the fracture fragment (Fig. 32.5). Meniscal entrapment, although suspected on MRI, is definitively diagnosed during the diagnostic arthroscopy. One prior study by Kocher et al.8 identified an entrapment of the anterior horn of the medial meniscus, intermeniscal ligament, or anterior horn of the lateral meniscus in 26% of type II fractures and 65% of type III fractures. In cases where there is interdigitation of the meniscus between the plateau and the fracture fragment, a probe can be used to carefully elevate the meniscus from below the tibial spine fragment. With the knee flexed, the tibial spine avulsion fragment is anatomically reduced back into its bed on the tibia. We usually use an ACL tibial guide to manipulate the fracture fragment (an angled microfracture pick or K-wire can also be used). The ACL insertion on the tibia can be used as an anatomic guide for reduction, and reduction should be confirmed by direct visualization under arthroscopy.