Fig. 24.1
Jones classification of tibial hemimelia
Kalamchi and Dawe, in their study of 21 cases in 1985, proposed a modification to the Jones classification and the results of their treatments for each type [48]. Type I deficiencies were defined as a total absence of the tibia. This group had knee flexion contractures, greater than 45° and no active quadriceps function. These patients also had proximal migration of the fibular head and hypoplasia of the distal femur. Type II deficiencies were defined as distal tibial aplasia, with a proximal tibia present. There was active quadriceps function and had knee flexion contractures between 25° and 45°. They had more normal development of the distal femur, with normal metaphyseal width and normal epiphyseal ossification, indicating at least a proximal tibial anlage was present. There was also less proximal migration of the fibula. Type III deficiencies were defined as distal tibia aplasia with diastasis of the tibiofibular syndesmosis. They had normal knee joints and good quadriceps function. Usually the talus was subluxated proximally with a prominent distal fibula.
Paley proposed a classification in 2003 based on the Jones classification [49]. The Paley classification (Fig. 24.2) is modified in this manuscript and described in more detail below. The classification is oriented around the treatment for each type.
Fig. 24.2
Paley classification of tibial hemimelia
The most recent classification scheme was published by Weber in 2007 [50]. Previous classifications had not taken into account the cartilaginous anlage. He also added a few types of tibial hemimelia which were previously unclassifiable by the previous schemes and previously published by case report [51]. Weber’s new classification took into account the entire affected leg, from hip to foot. He proposed seven types of increasing severity, with subgroups based on whether the cartilage anlage was present (a) or not (b). Type 1 was tibial hypoplasia but intact proximally and distally. Type 2 was distal diastasis. Type 3 was distal aplasia. Type 4 was proximal aplasia. Type 5 was bifocal aplasia proximally and distally. Type 6 was complete tibial agenesis with double fibulae. Type 7 was complete agenesis with a single fibula. He then assigned a score to determine the functional ability of the limb, where higher scores indicate less impairment of the limb. The tibia (0–22 points) and presence of an anlage (+10 points) weighed heaviest in importance, and the patella (0–3 points) was given slightly extra weight. The rest of the limb was scored from 0 to 2 points, and included the hip joint, distal femur, fibula, foot, and muscle function over the hip, knee, and ankle joints. Five classes were defined based on the score, indicating the degree of deficiency and difficulty of reconstruction.
The rarity of tibial hemimelia lends itself to other variants, which still may not fit any classification scheme. One reported case which does not fit any current classification is that of the intercalary deficiency, where the central portion of the tibia is missing but the proximal and distal tibia is intact [52]. The authors in this case were able to transfer the fibula into the defect with success.
Box 24.2. Jones Classification
Type I: No visible tibia
Ia: Hypoplastic distal femoral epiphysis
Ib: Normal distal femoral epiphysis ossification (possible cartilaginous proximal tibia)
Type II: Distal tibia deficiency
Type III: Proximal tibia deficiency
Type IV: Shortened tibia with distal tibia-fibula diastasis
History of Treatment
Early Treatments
In 1877, Albert first published about the centralization of the fibula, fusing the femur and fibula [53]. In 1905, Myers [54] proposed a fibula-femoral arthroplasty, which was further developed by Brown in 1965. In the case of a partial absence of the tibia, there are early published reports of attempted synostosis between the tibial remnant and fibula, either side-to-side or end-to-end (Bade [55], Nove-Josserand [56]). Fraser and Robarts in 1914 reported a case with an intercalary defect in which they transplanted the contralateral fibula with reported success [57]. In 1929, Putti [58] was one of the first to give directives on treatment, describing different approaches to eight different cases: fusing the fibula to the talus in extreme equinus to increase the leg length, transfer of the proximal fibula to the intercondylar notch, and side-to-side synostosis of the fibula to the tibia both proximally and distally. Sulamaa and Ryoeppy [41] performed side-to-side opposition and recommended knee disarticulation for type I deformity.
In the current literature, the treatment of choice for tibial hemimelia has historically been biased towards amputation, though it is dependent upon the classification of the deformity. In addition, in some communities, the option of amputation is not accepted culturally, and patient families wish to pursue limb salvage. With complete absence of the tibia (Jones type Ia), most literature points towards amputation [32, 42, 48, 67, 69], while less severe deformities have several case reports of salvage options [59–61]. The presence of a tibia anlage and an active quadriceps mechanism are important factors for reconstruction, as well as prevention of knee flexion deformities [62]. Their absence may be indicated by the absence of a patella, which can be difficult to find in young children. Thus, current imaging options such as MRI and ultrasound are a useful method of determining the presence of the patella or tibia anlage [63].
Brown Procedure (Fibular Centralization)
Brown first published his surgical procedure of fibular transfer and centralization under the femur in 1965 [64]. This procedure was done for patients with complete absence of the tibia (Jones type I). He also recommended a Syme-type amputation of the foot. In 1972, Brown published his 15-year follow-up, in which 40 of 56 patients were available for review [65]. Eighteen required secondary surgery due to a knee flexion deformity. Of the remaining 22, 1 was nonambulatory, and all but 2 were wearing braces while ambulatory. He recommended attachment of the patellar ligament to the fibula, preoperative traction, as well as femoral shortening and soft tissue releases as needed to gain extension. He also recommended surgery before age 1 for maximal ambulatory and fibular articulation potential. Inferior results were noted with an absence of quadriceps function.
Jayakumar and Eilert (1979) [66] reported six cases treated with the Brown procedure. All patients received either a Boyd or Syme amputation. Clinical outcomes were graded on several criteria of knee joint function, requiring (1) at least 10–80° of active range of motion, (2) <5° varus/valgus instability, and (3) no flexion contracture. Only two patients achieved these criteria, and they had 3+ quadriceps power. One patient had ipsilateral congenital femoral deficiency and underwent a femoral-fibula arthrodesis. Three patients had “poor” results from knee flexion contractures and two went on to knee disarticulations. The authors concluded that strong active quadriceps function of at least 3+ was necessary for Brown reconstruction to have superior results to an amputation.
Loder and Herring (1979) [67] reported nine cases of Jones type I deficiencies treated with the Brown procedure. All had preoperative knee flexion contractures. Initially, five of nine had good results with active range of motion and no flexion contractures. However, only one patient maintained active quadriceps power, and all progressively developed knee flexion contractures. Despite secondary procedures, outcomes were also poor due to knee instability and poor range of motion. At final follow-up, five had knee disarticulations and the remaining cases had poor range of knee motion (10–45°).
Epps and Schneider (1989) [68] published on three cases of Brown procedures, and noted that their results deteriorated over time due to progressive flexion contractures, and needed secondary procedures. In 1991, Epps et al. [69] reported on 14 patients (20 knees) who underwent centralization of the fibula for Jones type I tibial hemimelia. All patients developed progressive knee flexion deformities and needed multiple secondary procedures, leading the authors to recommend early disarticulation of the knee and prosthetic fitting as the treatment of choice. However, the results were considered to be failures due to the knee flexion deformities.
Simmons et al. (1996) [70] revisited the Brown procedure, publishing his results on five patients and seven limbs. All cases had Jones type Ia deformities, though one case was found to be a 1b during surgery and thus the rudimentary proximal tibia was utilized for fixation. All patients had knee flexion and varus deformities. They also had equinovarus deformities of the foot and underwent Syme amputations. An anterolateral knee incision was used, and the biceps tendon and distal insertion of the patellar tendon released. Femoral or fibular shortening was performed as needed along with peroneal nerve decompression. The fibula was centralized underneath the femoral condyles and the knee stabilized in extension with a Steinmann pin. The patellar tendon was reattached to the fibula and along leg spica cast was applied. Subsequent procedures included split thickness skin grafting, and heel pad release for the Syme amputation, and one quadricepsplasty for lack of knee flexion. All ambulated with a PTB socket with thigh extension. Average range of knee motion was 57° and only two patients achieved 10–80° of knee flexion. However, all patients were satisfied and none went on to knee disarticulation. They recommended narrowing indications for reconstruction to those patients with grade 3+/5 active quadriceps, younger than 1 year of age, no fibular bowing, and ambulatory potential.
Wada et al. (2006) [71] published nine cases of limb reconstruction in Jones type I and II cases. They performed four tibiofibular synostosis and five Brown procedures, with concurrent foot centralization procedures and subsequent lengthening as needed. The tibia-fibular fusion patients had good results with preserved knee function. Of the Brown procedures, four had poor quadriceps function and one had persistent knee instability. All five had unsatisfactory functional results based on Jayakumar’s criteria [66]; however, they were all household ambulators with only one patient needing an orthosis.
Hosny (2005) [72] published a case series of 6 patients with tibial hemimelia. Amputation was not accepted in his community and they presented at an older age (3.5–13 yo). Jones type I cases were treated with gradual distraction of the fibula with an external fixator, followed by a Brown procedure 1 month later. Type II cases were treated with gradual distraction followed by fixation of the proximal fibula to the proximal tibia. Fibula lengthening was subsequently performed but had limitations due to knee flexion contractures that resulted. Femoral lengthening was then performed at a later stage. Hosny reported all patient’s families were satisfied with the outcome, with all the type II patients ambulating independently with minimal (5°) to no knee flexion contractures and active ROM greater than 90°. The type I patients could walk with a KAFO and walker and had limited ROM (10–35/40°) but could perform ADLs at home without any pain.
Overall, most authors did not report good outcomes with the Brown procedure and recommended knee disarticulation rather than reconstruction as the best option for total absence of the tibia. Many of the poor outcomes were due to progressive knee flexion contractures, knee instability, and poor range of motion, as previously defined by Jayakumar [66]. However, for some patients in whom amputation is not an option, a limb that is weight bearing though less functional may be considered a success. Certainly the presence of a strong quadriceps, patella, and proximal tibia or anlage seems to favor reconstruction, and tibiofibular synostosis has generally met with good results. In addition, the use of an external fixator prior to reconstruction can help overcome soft tissue contractures.
Amputation
Knee disarticulation has been described for treatment and remains a salvage option for failed Brown procedures, as seen in many of the studies above. Kalamachi (1985) [48] treated three children with the Brown procedure, and all went on to subsequent knee disarticulations. The failure was attributed to knee flexion contractures and no active quadriceps function, leading the authors to recommend early disarticulation of the knee without attempt of reconstruction. Alternatively, if the femur was severely hypoplastic, a femorofibular arthrodesis was performed to effectively lengthen the femur, creating a longer lever arm for improved prosthetic fitting.
Similar results and conclusions were drawn by Schoenecker et al. (1989) [32]. Of a series of 57 patients and 71 limbs, 61 limbs eventually had some type of an amputation. Brown procedures were performed on 14 Jones type Ia limbs. Ten required secondary procedures due to knee instability or flexion contractures. Based on their results, they recommended evaluating for a proximal tibia anlage to differentiate Jones types 1a and 1b, and that a type Ia should be treated by knee disarticulation due to their less-than-satisfactory results with the Brown procedure.
Fernandez et al. (1998) [38] have also been a proponent of early amputation. Twenty-two cases of tibial hemimelia were reported, of which 17 patients (and caretakers) accepted surgery. All ten Jones type I cases underwent knee disarticulation. Three Jones type II and III cases had distal amputations. Only the remaining four Jones type IV cases had conservative treatment. The author recommended early amputation so that the patient would treat it as a “congenital amputation,” allowing for better adaptation to their prosthesis and rehabilitation. For many of these patients, their socioeconomic status also required a quicker and more definitive solution.
Spiegel et al. (2003) [31] described some potential complications and sequelae of amputation in patients with tibial hemimelia. They treated nine Jones type I deficiencies with knee disarticulation without any subsequent complications. Five type II deficiencies were initially treated with distal amputation (Chopart or Syme). They developed prosthetic irritation from the proximal fibula from the varus malalignment and prominent fibular head. Three patients subsequently underwent tibiofibular synostosis. One patient had progressive varus deformity and difficulty with prosthetic fitting that improved after hemiepiphysiodesis. Overall, the authors felt unsure about the best course of action for type II deficiencies. Four type III deficiencies were treated with Syme or Chopart amputations and did well.
Tibiofibular Synostosis
In the presence of a tibial anlage (Jones type Ib) or a proximal tibia (Jones type II), most authors have reported good results with tibiofibular synostosis. Kalamachi [48] reported ten patients with Jones type II tibial hemimelia that were treated with tibia and fibula synostosis. Three of these utilized a modified Brown procedure, fusing the fibula with the cartilaginous tibia anlage. They found good stability and adequate range of motion with only mild (20–30°) flexion contractures. Due to leg length discrepancies and foot deformities, half had concurrent Boyd amputations and did well with a prosthesis.
Schoenecker [32] reported 8 of 15 Jones type II limbs successfully treated with tibiofibular synostosis. Twelve were treated with a Syme amputation and were functional below-knee amputees, one had a knee disarticulation, one was nonoperative, and only one patient, who also had a tibiofibular synostosis, retained the foot. They recommended tibiofibular synostosis for Jones Ib and II with concurrent distal Syme or Boyd amputations.
Distal Tibia and Ankle Stabilization
For Jones type II deficiencies, distal tibia aplasia leads to an unstable ankle. These have historically been treated with stabilization of the ankle in the form of arthrodesis and possible amputation. In Kalamachi’s [48] series, three cases had essentially normal knees, but the talus was subluxated proximally with a varus foot and prominent distal fibula. These were treated with calcaneo-fibular fusions and Boyd amputations. Schoenecker [32] treated seven Jones type limbs with Syme or Chopart amputations to function as below-knee amputees. Tibiofibular synostosis was performed in two of these patients.
Jones type IV deficiencies have a shortened tibia with significant distal tibia and fibula diastasis. Tokmakova et al. (2003) [73] felt that the treatment of choice was reconstruction of the ankle mortise, as their patients were independent ambulators with stable ankles and plantigrade feet.
In Schoenecker’s series of ten Jones type IV limbs, one limb had a Syme amputation and nine limbs had ankle joint reconstruction and salvage of the foot. Of these nine, five had a Syme amputation within 3 years due to leg length discrepancy. He recommended ankle reconstruction and leg length equalization, similar to Fernandez [38].
Limb Lengthening
Limb lengthening is also an option and adjunct for the treatment of tibial hemimelias [74]. Hootnick et al. (1977) [75] followed the natural history of tibial hemimelia and found that the leg length discrepancy remained proportional over time. Thus, they were able to calculate a final predicted leg length discrepancy to help a family decide on lengthening versus Syme amputation. They recommended amputation for predicted discrepancies greater than 8.7 cm. However, with newer technology and a better understanding of the biology, staged reconstruction and limb lengthening may allow the trained surgeon to address more severe cases of congenital tibial deficiency, preserving more lower limb function than what has been reported previously.
Desanctis et al. (1990) [76] published three cases of Jones type II deficiencies treated with staged reconstruction. They corrected the foot deformity with serial casting and posteromedial soft tissue release, followed by tibiofibular diaphyseal reconstruction, alignment of axis of the foot and leg, and limb lengthening using the Ilizarov technique. Javid (2000) [77] reported on a lengthening after centralization of the fibula in a Jones IIb deformity. They found that the fibula had delayed new bone formation, and compression-distraction technique with an Ilizarov device had to be utilized to promote osteogenesis. Devitt reported good results with differential lengthening of two cases of Weber type I deficiency [51].
Weber Patelloplasty
The Weber patelloplasty was published in 2002 [78] and described a surgical procedure in which the patella was converted into a tibial plateau. The soft tissues were gradually distracted with an external fixator to avoid the need to shorten the femur or fibula. The patella is then brought down with crossing “visor” flaps from the capsule and chondrodesed to a centralized fibula. A Z-plasty of the quadriceps tendon was used to gain length. A hinged external ring fixator was used to stabilize while allowing knee range of motion and weight bearing. A second procedure was done to achieve chondrodesis between the distal fibula and the talus. To our knowledge, there have been no publications of results of this procedure, though Weber did further describe and refine his procedure in 2006 [79].
Box 24.3. Treatment Options
Outcomes for the Brown procedure (centralization of the fibula) depend on the presence of a quadriceps mechanism and a mobile knee without flexion contractures.
Progressive knee flexion contractures and knee instability are common reasons for failure of the Brown procedure.
The presence of a proximal tibia or its anlage has had good results from synostosis with the fibula.
For some parents, a quicker and more definitive knee disarticulation may be a more attractive option, allowing a child to adapt early to a prosthesis.
Distal tibia deficiencies can be treated with distal fusion or synostosis or Syme-type amputation.
Advances in limb lengthening allows for limb length equalization.
The Weber patelloplasty converts an existing patella into a proximal tibia.
New Horizons and Strategies for Reconstruction in Tibial Hemimelia
The deficiency in tibial hemimelia is a spectrum of pathology, ranging from a congenitally short tibia with relative fibular overgrowth to complete absence of the tibia. It is to be distinguished from fibular hemimelia, where there is a progressive deficiency of the fibula, ranging from a congenitally short tibia with relative fibular hypoplasia to complete absence of the fibula. An important distinction between these two conditions is that the foot and ankle are always in varus with tibial hemimelia and almost always in valgus with fibular hemimelia. The progression of deficiency of the tibia is from distal to proximal, contrary to fibular hemimelia, where the progression of fibular deficiency is from proximal to distal. Tibial hemimelia should be distinguished from proximal deficiency of the knee, which is most commonly associated with TAR (thrombocytopenia absent radius) syndrome. Proximal deficiency of the tibia ranges from simple genu varum to a ball and socket, complete absence, or congenital fusion of the knee joint. Therefore, in order to prevent confusion, tibial hemimelia should be classified as an incremental deficiency from distal to proximal.
Most classifications in orthopedics classify pathology from the less severe to the more severe (e.g., Garden classification of hip fractures [80], Berndt and Harty classification of talar dome osteochondral fractures [81], Herring and Catterall classifications of Perthes [82, 83], and Kalamchi classification for fibular hemimelia [84]). The Paley classifications [85] for congenital femoral deficiency and fibular hemimelia (FH) follow a similar format. Some well-accepted published classifications follow the opposite format, starting with the most severe or deficient cases (e.g., Pappas classification for CFD [86], Kalamchi classification of tibial hemimelia [48], and Jones classification for tibial hemimelia [47]). The Jones classification for tibial hemimelia has been the most widely used, but it is in reverse order of deficiency. Furthermore, the Jones type III is so rare that the senior author has only seen two cases of it in 27 years of practice and more than 300 cases of tibial hemimelia. The complete absence of the proximal tibia in the Jones III makes its treatment similar to the Jones I where the proximal tibial is missing. One consideration was to add this subtype to the Paley type 5 group. I have chosen not to do this since the treatment is the same whether the distal tibia is present or not. The treatment at the knee still depends on the presence or absence of the patella and whether the fibula is autocentralized or not. The treatment of the foot does not change since the foot is in severe equino-varus as if this remanant of distal tibia was not present (Figure 24.3). Finally, the Jones classification also lacks description of several types of tibial deficiency that involve both the proximal and distal physes, such as the Delta tibia type [87] or types that have a normal appearing tibia beside a longer fibula. The Jones classification also does not consider the presence or absence of a patella.
Fig. 24.3
(a) Jones type III tibial hemimelia. This would be classified and treated as a Paley type 5 despite the remnant of distal tibia. (b) Long x-ray of both legs showing the bilateral nature of this rare type. The left leg is a Paley type 3a and cannot be classified using the Jones classification. (c) Magnetic resonance imaging (MRI) confirming that there is no cartilaginous proximal tibia. (d) Another MRI cut confirming absence of the proximal tibia
The Weber Classification [50, 79] changed the order back to increasing severity of deficiency. It also included types with a proximal deficiency (type 3). Similar to the Pappas classification, it splits tibial hemimelia into a large number of types (total of 7). The Weber also subdivides into types that will eventually ossify and change into other types (types 3, 4, 5, 6, 7). The Weber scoring system, combined with the large number of subdivisions, makes this classification challenging for practical use.
Dissatisfied with the existing classifications and prior to Weber’s publication, Paley proposed a new classification in 2003 [49]. Each type and subtype has a different surgical treatment. The progression of deficiency is from least to most, and the classification assumes that tibial hemimelia is a progressive spectrum of deficiency from distal to proximal.
Box 24.4. Paley Classification of Tibial Hemimelia (See Fig. 24.2)
Type 1: Congenital short tibia with relative overgrowth of the fibula, distal tibial plafond intact
Type 2: Congenital deficiency of the tibial plafond with diastasis of the tibia and fibula and relative fibular overgrowth
Type 3: Congenital deficiency of tibia with proximal and distal physis of tibia present; distal tibial physis more dysplastic than proximal; relative fibular overgrowth
Type 4: Absent distal tibia; proximal tibia present; relative fibular overgrowth
Type 5: Complete absence of tibia, fibula present
Paley Classification with Subtypes and Description of Common Features
Type 1: Valgus proximal tibia (genu valgum), overgrowth of fibula proximally, plafond present and normal.
Type 2: Tibial plafond missing. Medial and lateral malleolus present; distal fibula (lateral malleolus) normally aligned to lateral talus, internally rotated with foot around the tibia. Talus is positioned between the tibia and fibula due to absence of tibial plafond. Relative fibular overgrowth present. Foot follows the fibula. The diastasis can extend as a cleft between the tibia and fibula.
Type 3a: Well-formed distal tibial physis and separate from proximal growth plate of tibia. Plafond present but dysplastic. Major relative overgrowth of fibula.
Type 3b: Delta Tibia: proximal and distal growth plates connected through bracket epiphysis. Malorientation of ankle and knee joints ends of tibia. Major relative overgrowth of fibula.
Type 4a: Delayed ossification of part, or all, of the tibia. Ankle joint present, but distal tibial physis absent. Major relative overgrowth of fibula.
Type 4b: Diaphyseal deficiency of tibia. Complete absence of distal tibia at level of diaphysis; proximal tibia has atrophic, pointed bone end often covered by separate skin pouch. Major relative overgrowth of fibula.
Type 4c: Epiphysis of proximal tibia present but absent proximal physis. Knee joint present. Delayed ossification of epiphysis. Significant relative overgrowth of fibula.
Type 5a: Complete absence of tibia: a remnant of distal tibia may be present in rare cases; patella present; flexion contracture of knee.
Type 5b: Complete absence of tibia; no patella present; flexion contracture of knee; fibula may be (i) auto-centralized or (ii) dislocated.
Limb Reconstruction Surgery
Since Brown introduced centralization of the fibula, many attempts to reconstruct the knee in the most severe types (Jones I, Paley 5) have been made. These have been met with poor results, as previously discussed. Similarly, poor results of reconstruction for Jones types II and IV and Paley types 2, 3, and 4 have led most surgeons to conclude that through-knee amputation for Jones type I, through- or below-knee amputation for Jones type II, and Syme’s amputation for Jones type IV are the best treatment for each type of tibial hemimelia. In light of the advances in modern prosthetics, this is definitely a good option and should be considered as the most tried and proven method of treatment. However, advances in the treatment of all types of tibial hemimelia offer new options with excellent functional results as an alternative to amputation. The rest of this manuscript will focus on the reconstructive options for tibial hemimelia according to Paley type and subtype.
Paley Type 1 (Fig. 24.4)
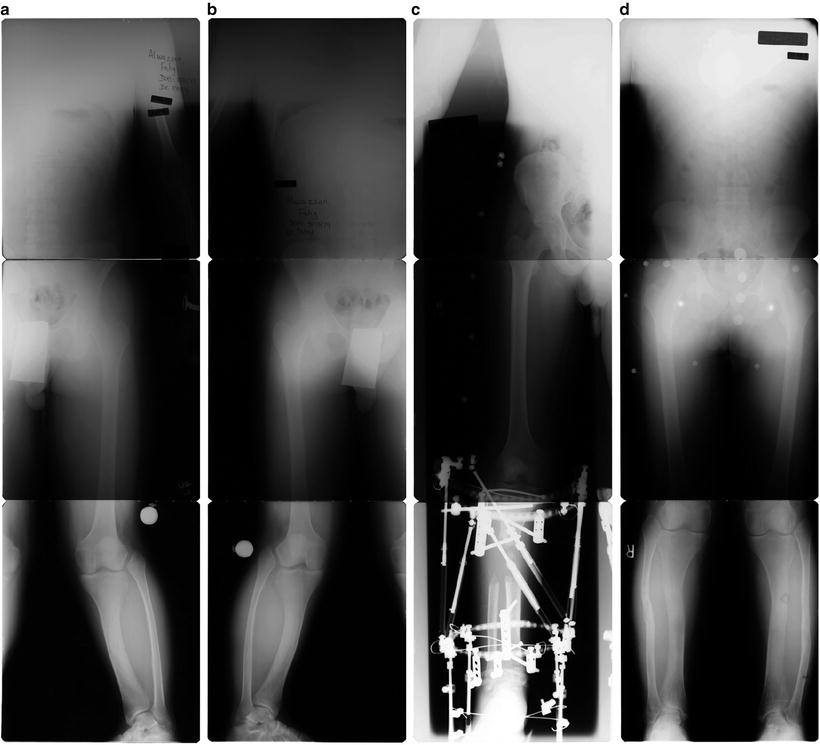
Fig. 24.4
(a, b) Right and left AP radiograph of Paley type 1 TH side showing valgus tibial deformity and overgrowth of fibula. (c) Lengthening and valgus correction of tibia and fibula with TSF. The fibula is not transported distally. (d) Final standing radiograph showing good alignment bilaterally. Proportions of femur to tibia restored closer to normal
These patients tend to have bilateral involvement. The condition is often familial (autosomal dominant). The tibias are short and the knees are in valgus. The valgus is usually from the proximal tibia, but can also be from the distal femur. If treated when the physes are open, the valgus can be corrected using temporary hemiepiphysiodesis. In adulthood, the valgus can only be treated by osteotomy. The biggest complaint of these patients is mesomelic disproportion and short stature. Therefore, the treatment is usually bilateral and includes tibial lengthening for stature in addition to correction of the valgus angulation. In regard to the overgrown proximal end of the fibula, which often articulates with the side of the femur, I prefer to leave it alone and not pull it distally. This avoids the problem of a knee flexion contracture that can result from transporting the fibula distally. If the proximal fibula is producing a noticeable bump that is bothersome to the patient, then the tibia can be lengthened without cutting the fibula, transporting the fibula distally.
Paley Type 2 (Fig. 24.5, 24.6)
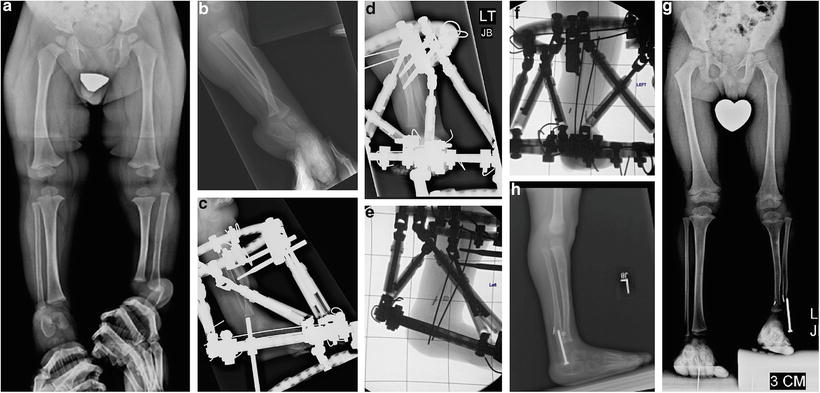
Fig. 24.5
(a) AP and (b) lateral radiographs of Paley type 2 TH. The distal fibula is more anterior than the tibia on the lateral. The distal fibula goes with the talus and is more hypertrophied than the distal tibia. (c, d) TSF device applied to foot and tibia for distraction of contracture of foot and to move the talus under the distal tibia. (e, f) After the talus is under the tibia, the ankle joint is opened and a biologic arthroplasty of the ankle joint is performed. A suture washer system is used to compress the diastasis. An intramedullary wire is placed to hold the foot in place under the tibia and the external fixator is left in place for 3 more months. (g, h) Epiphysiodesis of the distal fibula is performed to prevent distal overgrowth of the fibula. The final result is a plantigrade stable foot with some motion of the ankle
The diastasis of the tibia with the fibula starting with the absence of the tibial plafond (Fig 24.4) may extend up the tibia. The tibia may have a varus bow to its diaphysis and in rare cases there can be a skin cleft between the two bones (Fig. 24.5). The foot always remains with the fibula. The foot is in equinovarus and internally rotated relative to the knee. The talus is proximally migrated relative to the distal tibia. The talus is at the correct level relative to the distal fibula. Since the ankle joint is to be reconstructed, the Achilles tendon is not cut but a gastrosoleus recession may be performed. The foot is repositioned by gradual distraction of the foot from the tibia using a circular ring external fixator. To prevent epiphysiolysis of the proximal and distal fibula, a 1.5-mm wire is drilled retrograde into the fibula and up the fibular diaphysis to exit through the proximal fibular epiphysis. The wire is brought through the skin proximally and then bent backwards on itself to form a hook. A small proximal incision is made and the wire is pulled back into the fibular head to lock into the proximal epiphysis. Distally, the wire is also bent 180°, then shortened and buried under the skin. This creates a temporary epiphysiodesis of the proximal and distal fibula.
One ring is applied to the proximal tibia with one wire and two half pins. The second ring is applied to the foot with three wires. The equinovarus deformity is corrected by gradual distraction of the foot away from the knee, repositioning the talus under the distal tibial epiphysis. Since the fibula is overgrown relative to the tibia, it does not need to be fixed to the distal ring. Its association with the talus and calcaneus causes it to follow the foot distally. This moves the fibula from its relatively overgrown proximal position down to the normal station.
Once the foot is located under the distal tibial epiphysis, a planned second stage surgery can be carried out. Under general anesthesia, the distal ring and wires are removed. The pin sites are covered by Betadine soaked gauzes and the leg is prepped and draped free. A transverse incision is made on the medial side at the level of the tip of the medial malleolus. The tibiotalar joint is opened, and the distal tibia and proximal talus are exposed. The tibialis posterior tendon is often found dislocated between the tibia and fibula, where the plafond should have been. It is moved out of this location and retracted postero-medial to the tibia. The distal end of the tibial cartilage is carved with a knife to the concavity of the tibial plafond, matching the convexity of the dome of the talus, creating a biologic arthroplasty. A wire, perpendicular to the sole of the foot, is passed through the dome of the talus, through the epiphysis of the distal tibia, and continues proximally into the tibial diaphysis. If the tibia has a varus diaphyseal bow to it, a percutaneous osteotomy should be made at the apex of this bow with an acute angular correction, straightening the tibia. The wire is advanced up the tibia to stabilize this osteotomy.
The tibiofibular diastasis is treated next. This is fixed by using a syndesmotic suture system such as the Arthrex-Tightrope™ or the Biomet-Ziptite™. The syndesmotic suture with its two washers is used to reduce and compress across the diastasis. The incision is then closed, and the foot ring is reapplied with three new wires. This helps ensure that the foot remains in a plantigrade position.
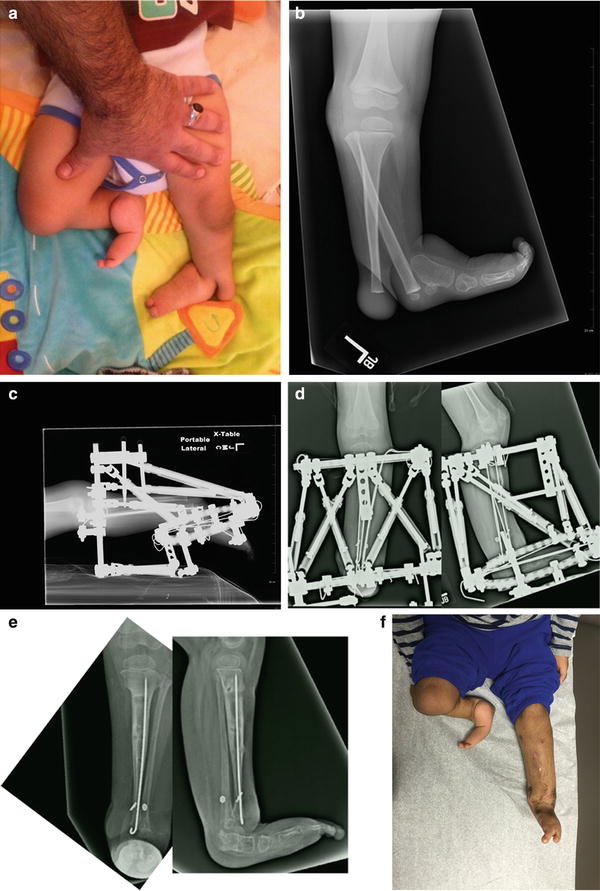
Fig. 24.6




(a) Paley type 2 variant: Clinical photo showing there is a cleft associated with the distal tibio-fibular diastasis. Notice that the foot goes with the fibula. There is also tibial hemimelia on the other side Paley type 5. (b) Radiograph showing the diastasis and cleft. (c) Radiograph of the TSF external fixator applied to the foot and tibia at onset of correction. Notice the 90° equinus contracture requiring the rings to be at 90° to each other. (d) AP and lateral radiographs after the correction is completed. The talus was centralized under the distal tibia. The syndesmotic repair was done using the Ziptite suture-washer implant. The two washers can be seen on the x-ray. The cleft was surgically closed. (e) Final AP and lateral radiographs showing the foot is plantigrade and the talus is centered under the tibia. The fibula is lateral to the talus. The cleft and diastasis are closed. (f) Final clinical photo from the front showing that the cleft is closed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


