Thin Corpus Callosum
Susan I. Blaser, MD, FRCPC
DIFFERENTIAL DIAGNOSIS
Common
Normal Variant
Immature Brain
Encephalomalacia
Multiple Sclerosis
White Matter Injury of Prematurity
Callosal Dysgenesis
Callosectomy/Callosotomy
Obstructive Hydrocephalus
Less Common
Hypomyelination
Injury (Any Cause)
Rare but Important
Susac Syndrome
Holoprosencephaly
Inherited Metabolic Disorders
Hereditary Spastic Paraplegia with Thin
Corpus Callosum (HSP-TCC)
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Diffuse corpus callosum (CC) thinning can be normal
Newborn (immature brain)
Abnormally thin CC can be inherited or acquired
Broad spectrum of congenital malformations, inherited metabolic disorders can all result in thin CC
Check history for trauma, surgery, ischemia-infarction
Thin CC, normal signal hyperintensity
Normal variant, immature brain
Secondary to hemispheric white matter (WM) volume loss
Dysgenesis
Thin CC, abnormal signal intensity
Hypomyelination or demyelinating disease (chronic MS, Susac syndrome)
Injury (trauma, ischemia, radiation, toxic-metabolic insult)
Obstructive hydrocephalus
Helpful Clues for Common Diagnoses
Normal Variant
Focal thinning of corpus callosum at “isthmus” (junction between posterior body, splenium) is normal
Sagittal section slightly off-midline can make corpus callosum appear mildly thinned
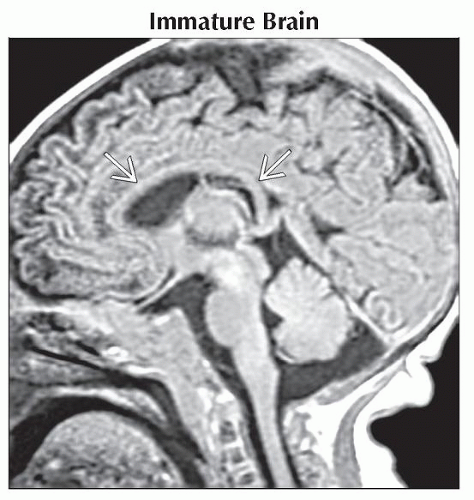
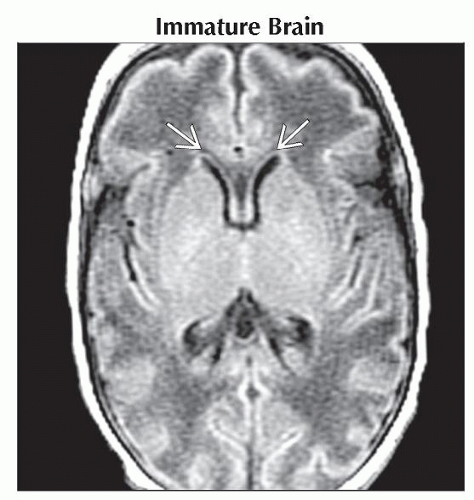
Immature Brain
Hemispheric WM in newborn unmyelinated, corpus callosum thin and hypointense on T1WI
As myelination progresses, corpus callosum thickens, becomes hyperintense on T1WI
Corpus callosum splenium at 4 months
Corpus callosum genu at 6 months
By 8 months, corpus callosum essentially like an adult’s
Encephalomalacia
Holohemispheric WM volume loss, regardless of etiology, causes diffuse corpus callosum thinning
Focal WM loss can cause focal corpus callosum thinning
Multiple Sclerosis
Look for T2/FLAIR hyperintense lesions along callososeptal interface
Ependymal “dot-dash” sign along callosoventricular border occurs early
Longstanding MS with decreased hemispheric WM volume results in thinned corpus callosum
White Matter Injury of Prematurity
Corpus callosum thinning secondary to periventricular white matter infarction
Posterior corpus callosum disproportionately affected
Callosal Dysgenesis
Hypoplasia or absence of part or all of corpus callosum
Rostrum, splenium most likely deficient
Remnants vary in size, shape, and configuration
Most common abnormality associated with other malformations
Chiari 2 malformation
Heterotopias
Interhemispheric lipoma
Cephaloceles
Callosectomy/Callosotomy
History important!
Surgical disruption
Look for surgical changes of craniotomy, ventriculostomy
Obstructive Hydrocephalus
Causes 2 kinds of corpus callosum abnormalities: Stretching and intrinsic signal abnormality
As lateral ventricles enlarge, corpus callosum is stretched, appears thinned
Look for associated signal abnormality in corpus callosum (sagittal T2WI/FLAIR best)
Post-shunt decompression may show corpus callosum thinning, signal abnormality
Can appear bizarre, causing horizontal hyperintense “streaks” in corpus callosum on axial imaging
Can extend into periventricular WM
Theories: Impingement of corpus callosum against falx cerebri with resulting ischemia or axonal stretch
Helpful Clues for Less Common Diagnoses
Hypomyelination
Undermyelination, delayed myelin maturation
Diminished/absent WM myelination for age
Can be primary or secondary to other pathology
Injury (Any Cause)
Trauma (e.g., axonal injury, radiation-induced leukoencephalopathy)
Ischemia
Helpful Clues for Rare Diagnoses
Susac Syndrome
M < F
Classic triad
Encephalopathy (headache, confusion, memory loss)
Vision problems (retinal artery occlusions)
Hearing loss
Always involves corpus callosum
Central > callososeptal interface lesions
Middle callosal “holes” (subacute/chronic)
Holoprosencephaly
Many variants; often affect corpus callosum
Inherited Metabolic Disorders
Focal or diffuse atrophy
Focal: X-linked adrenoleukodystrophy
Diffuse: Many
Hereditary Spastic Paraplegia with Thin Corpus Callosum (HSP-TCC)
HSP-TCC is 1 of many hereditary spastic paraplegias
Autosomal recessive with SPG11 gene mutations on chromosome 15q13-15
Progressive neurodegenerative disorder
Clinical
Slow ↑ spastic paraparesis
Adolescent-onset cognitive decline
Pseudobulbar dysfunction
Imaging
Thin corpus callosum (especially genu, body) with progressive atrophy
Cerebral, cerebellar atrophy often associated
Image Gallery
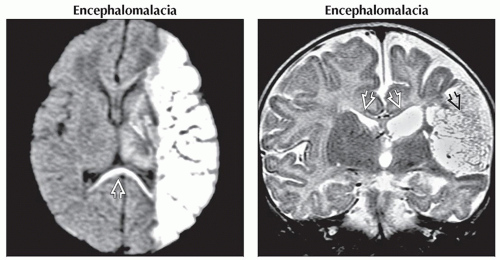 (Left) Axial DWI MR in a newborn shows extensive diffusion restriction of the left hemisphere following perinatal stroke. Acute axonal degeneration of the corpus callosum
 is present. (Right) Coronal T2WI MR at follow-up shows a large area of cystic encephalomalacia is present. (Right) Coronal T2WI MR at follow-up shows a large area of cystic encephalomalacia  and a very thin corpus callosum and a very thin corpus callosum  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|