Thick Cortex
Susan I. Blaser, MD, FRCPC
DIFFERENTIAL DIAGNOSIS
Common
Encephalitis
Herpes Encephalitis
Less Common
Hypomyelination (Pseudo Thick Cortex)
Tuberous Sclerosis Complex
Taylor Cortical Dysplasia
Pachygyria-Polymicrogyria
Hemimegalencephaly
Lissencephaly Type 1
Rare but Important
Neoplasms Associated with Cortical
Dysplasia
DNET
Ganglioglioma
Dysplastic Cerebellar Gangliocytoma
Glioblastoma Multiforme
Gliomatosis Cerebri
Meningioangiomatosis
Congenital Muscular Dystrophy
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
EXCLUDES transient (e.g., MELAS, cortical edema from stroke/seizure, etc.)
Is cortex thick on both T1 and T2W sequences?
Does cortex follow gray matter signal intensity (malformations)? or is it hyperintense (infection, neoplasm)?
Is thickened cortex very focal (think neoplasm)? or more generalized (malformation)?
Helpful Clues for Common Diagnoses
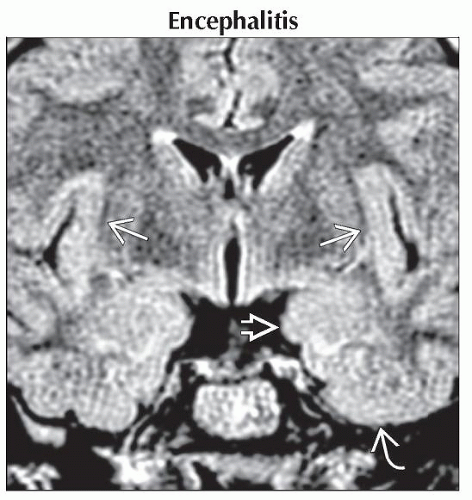
Encephalitis
Commonly identified agents: Enterovirus, HSV1, Mycoplasma pneumonia, Epstein-Barr, HHV-6, influenza
Etiology not found in ≈ 50%
Hyperintense on T2WI, FLAIR
Thickened, hyperintense temporal lobe/insular cortex
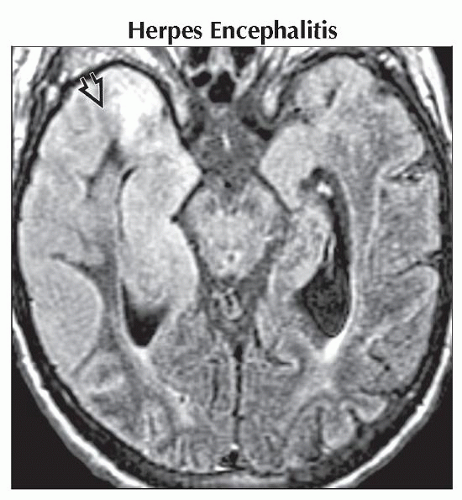
Herpes Encephalitis
Often bilateral, asymmetric
Look for cingulate gyrus, subfrontal cortex involvement
Restricts strongly on DWI
Enhancement, hemorrhage follow
Helpful Clues for Less Common Diagnoses
Hypomyelination (Pseudo Thick Cortex)
Diminished/absent white matter (WM) myelination for age
Lacks peripheral “arborization” of white matter
Can be primary or secondary
Primary hypomyelination (e.g., Pelizaeus-Merzbacher )
Secondary (prematurity, malnutrition)
Imaging
“Pseudo” thick cortex appearance
Poor gray-white differentiation on T1WI in children > 1 year
Poor gray-white differentiation on T2WI in children > 2 years
Small brain with thin corpus callosum
Tuberous Sclerosis Complex
Flattened, thickened gyri with “blurred”
GM/WM border
Can be calcified, involve entire mantle
Look for subcortical WM hyperintensities, subependymal nodules
Taylor Cortical Dysplasia
Also known as focal cortical dysplasia (FCD) type 2A/B
“Balloon cell” dysplasia
Malformation of cortical development
Refractory focal epilepsy
Thickened cortex with T1 hyperintensity, T2 hypointensity in infancy
Rare Ca++
Lesion conspicuity decreases with WM maturation
Pachygyria-Polymicrogyria
Polymicrogyria → excessively small, prominent convolutions (“gyri on gyri”)
Pachygyria (sometimes called incomplete lissencephaly) → thickened, dysplastic cortex
Both cause appearance of “thick cortex” on imaging
Density/signal intensity of affected cortex same as normal gray matter
Hemimegalencephaly
Hamartomatous overgrowth of part/all of a hemisphere
Enlarged hemisphere with thickened, often dysplastic cortex
Ipsilateral ventricle often enlarged, abnormally shaped
White matter often overgrows, is hypermyelinated
Lissencephaly Type 1
Most severe type (complete agyria) is Miller-Dieker syndrome
Thick, multilayered cortex
“Hour glass” configuration with shallow sylvian fissures in severe cases
Helpful Clues for Rare Diagnoses
DNET
Young patient, longstanding seizures
Well-demarcated “bubbly” intracortical mass
Often associated with adjacent cortical dysplasia
Ganglioglioma
Child/young adult, seizures
Superficial hemispheres, temporal lobe
Cyst with nodule, ± Ca++, enhancement typical
Solid ganglioglioma can resemble Taylor cortical dysplasia (TCD does not enhance)
Dysplastic Cerebellar Gangliocytoma
Thickening, overgrowth of cerebellar folia
Gyriform “layered” or “striated” pattern
Can cause significant mass effect
Cowden-Lhermitte-Duclos (COLD) syndrome is considered new phakomatosis
Multiple hamartoma-neoplasia syndrome
Long-term cancer screening (breast, thyroid)
Glioblastoma Multiforme
White matter > > gray matter
Tumor infiltration of cortex, subpial extension may occur late
Hemorrhage, enhancement common
Primary GBM (older patient) 95% necrotic with thick irregular enhancing rim
Secondary GBM (younger patient) shows enhancing focus within lower grade tumor
Gliomatosis Cerebri
Tumor infiltrates but preserves underlying brain architecture
2 or more lobes affected
T2 hyperintense infiltrating mass enlarges cortex, basal ganglia
MRS shows elevated myoinositol (mI)
Most are WHO grade II or III diffusely infiltrating astrocytoma
Meningioangiomatosis
Cortical mass with variable Ca++
Linear &/or gyriform enhancement
Perivascular proliferation of vessels in meninges, cortex
May infiltrate along perivascular spaces, cause mass effect
Congenital Muscular Dystrophy
Cobblestone lissencephaly (overmigration)
Z-shaped brainstem
Hypoplastic rotated cerebellum (similar to Dandy-Walker continuum)
Image Gallery
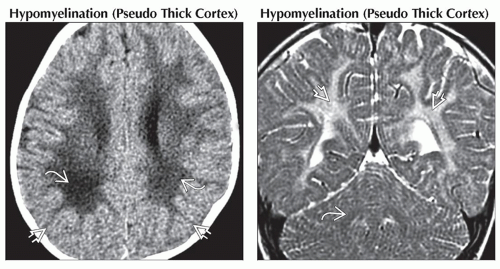 (Left) Axial NECT in a 4 month old with hypomyelination
 shows decreased volume and white matter density. The thin arbors of white matter give a false impression that the cortex, especially in the occipital poles, is thickened shows decreased volume and white matter density. The thin arbors of white matter give a false impression that the cortex, especially in the occipital poles, is thickened  . (Right) Coronal T2WI MR in an 18 month old with Pelizaeus-Merzbacher disease (PMD) shows white matter hypomyelination in the occipital lobes . (Right) Coronal T2WI MR in an 18 month old with Pelizaeus-Merzbacher disease (PMD) shows white matter hypomyelination in the occipital lobes  and cerebellum and cerebellum  , giving the appearance of prominent thick cortex. , giving the appearance of prominent thick cortex.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|