FIGURE 41-1 A: Coronal FSE PD MRI image demonstrates a capitellar osteochondral defect. B: Sagittal FSE IR MRI image reveals an intra-articular loose body in the anterior compartment of the elbow.
Little epidemiological data are available regarding the true incidence or prevalence of OCD. Prior studies by Lyman et al.20 have clearly demonstrated that approximately a quarter of all youth baseball pitchers will report elbow pain during a baseball season. Presumably, a considerable proportion of these complaints will be due to OCD.21 Until more thorough screening and longitudinal observational studies are performed, the exact frequency with which OCD occurs will remain unknown.
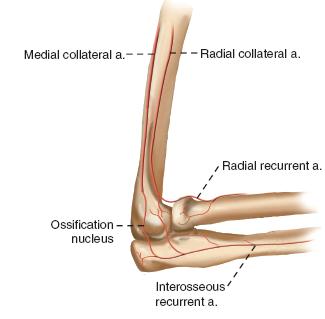
FIGURE 41-2 Schematic diagram of the vascular anatomy to the lateral elbow.
Clinical Evaluation
Over 90% of patients with OCD will present with lateral elbow pain. While often casually attributed to lateral epicondylitis or “Little Leaguer’s elbow,” careful history and examination will elucidate that the location of the pain is in the capitellum, not the lateral epicondyle or extensor-supinator mass (Figure 41-3). Direct palpation over the capitellum, which can only be performed with the elbow hyperflexed, will elicit tenderness. While usually present only during or immediately after provocative activities (e.g., pitching, gymnastics), often patients will develop continuous pain even at rest in advanced situations.
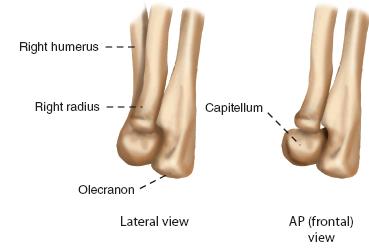
FIGURE 41-3 Schematic diagram demonstrating hyperflexion of the elbow, uncovering the capitellum in the typical region of OCD involvement. Direct palpation in this area with the elbow flexed will elicit tenderness in patients with OCD.
Up to half of patients will demonstrate subtle loss of elbow motion, typically an elbow flexion contracture. This is often the first clinical sign of internal derangement of the elbow. An elbow effusion may or may not be detectable. Similarly, RC crepitus or instability may be elicited in those patients with unstable lesions. Neurovascular examination is usually normal.
In the young thrower or overhead athlete, careful examination of the shoulder will invariably detect an internal rotation deficit (see Chapter 39). Identification of this is critical in the rehabilitation of elbow OCD. As the patient tries to impart more angular velocity during throwing, the presence of an internal rotation deficit will often result in a lower arm-trunk angle (“dropping down”) and greater valgus and lateral compression forces across the elbow, thereby increasing the risk for OCD.
Finally and perhaps most importantly, up to 20% of patients will present with mechanical symptoms of locking, catching, or giving way of the elbow. These symptoms should alert the examiner of the possibility of an intra-articular loose body and advanced stage of OCD.
In patients with medial elbow pain, tenderness with direct palpation of the medial epicondyle should alert the examiner to the possibility of medial epicondyle apophysitis. Tenderness more distally over the proximal flexor-pronator mass and pain with resisted wrist flexion are consistent with flexor-pronator tendinosis. In patients with suspected UCL insufficiency, a number of provocative maneuvers will elicit pain and/or instability, including: (1) valgus stress at 30 degrees of elbow flexion, (2) positive modified milking test, and (3) positive moving valgus stress test.22–24 Finally, all patients with medial elbow pain should be assessed for ulnar nerve instability and ulnar neuritis. Ulnar nerve subluxation may be palpated with elbow flexion and extension. A Tinel’s sign, positive elbow flexion test, diminished sensation in the ulnar two digits, or any evidence of adductor pollicis or intrinsic weakness should raise the question of ulnar neuropathy.
Plain radiographs should be obtained during the initial evaluation, including anteroposterior (AP) and lateral views. Contralateral elbow radiographs may be helpful for comparison, particularly in the more skeletally immature. Takahara et al.25 have also highlighted the utility of the 45-degree flexion AP view, which may better bring an OCD lesion into profile given its characteristic posterior location within the capitellum (Figure 41-4). In cases of suspected UCL insufficiency, a gravity stress radiograph can be obtained. This view is performed with the patient supine, shoulder abducted 90 degrees, and forearm maximally supinated (thumb pointed to the ground). An AP view of the elbow is then taken with the beam directed parallel to the floor. Medial joint space opening of ≥3 mm is indicative of valgus instability.
Increasingly, MRI is becoming the standard imaging modality of choice, given its ability to localize and stage the OCD lesion, as well as identify associated pathology, including intra-articular loose bodies.26 T2-weighted coronal and sagittal reconstructions are particularly helpful in identifying adjacent signal abnormalities or fluid undercutting of the lesion, radiographic features suggestive of fragment instability. Also, MRI may be helpful in identifying flexor-pronator tendinosis, medial epicondyle apophysitis, and UCL tears.
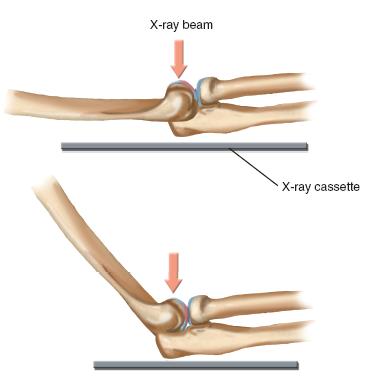
FIGURE 41-4 Schematic diagram depicting use of the 45-degree flexion AP view of the elbow to allow radiographic visualization of OCD lesions.
Currently, a host of classification systems exist for elbow OCD. Most are based on either radiographic or arthroscopic findings and divide lesions according to overlying cartilage integrity and fragment stability. Baumgarten et al.27 proposed an arthroscopic classification based upon that used to assess talar dome lesions. Grade 1 lesions had smooth but ballotable articular cartilage. Grade 2 lesions had cartilage fibrillations or fissures. In grade 3 lesions, there was exposed bone by stable osteochondral fragments. Grade 4 lesions were loose but undisplaced. Grade 5 lesions were displaced with intra-articular loose bodies.
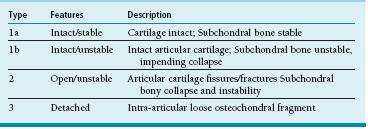
Difelice et al.28 proposed a similar classification system, also based upon cartilage integrity and fragment stability (Table 41.1). Type 1a lesions have intact articular cartilage and fragment stability. Type 1b lesions have intact articular cartilage but unstable subchondral bone with impending collapse. Type 2 lesions demonstrate cartilage fracture with collapse or displacement of sub-chondral bone (e.g., unstable but in situ). Type 3 lesions denote intra-articular loose bodies. This classification system is similar to that of the International Cartilage Research Society classification of osteochondritis dissecans. Grade 1 lesions denote softened but intact cartilage surfaces. Grade 2 lesions have cartilage fissuring but are stable upon probing. Grade 3 lesions demonstrate complete discontinuity of cartilage but remain localized (“dead in situ”). Grade 4 lesions describe displaced lesions. All these classification systems are helpful not only to describe radiographic or arthroscopic appearance but also in guiding treatment. As with many upper limb conditions, however, clinical symptoms often do not correlate with radiographic findings.1
Surgical Indications
Surgical treatment is indicated in cases of symptomatic elbow OCD with fragment instability or intra-articular loose bodies. Furthermore, surgical treatment is also relatively indicated in cases of stable OCD lesions with persistent functionally limiting pain despite “adequate” rest and rehabilitation.
SURGICAL PROCEDURES
The downside isn’t really injury, fear of injury, or the process of fighting injury. The downside, the very worst thing in the world, is surgery.
—Greg Rusedski
 Nonoperative Treatment of Elbow OCD
Nonoperative Treatment of Elbow OCD
Nonoperative treatment is recommended for the intact, stable elbow OCD lesion, particularly in the young, skeletally immature athlete. Complete rest of the affected elbow is initiated for 6 weeks, followed by physical therapy to work on posterior capsular stretching of glenohumeral internal rotation deficit, strengthening of the rotator cuff and periscapular muscles, strengthening of the flexor-pronator mass, and special attention to throwing mechanics. Core strengthening is a major part of their rehabilitation, as most of those young athletes need to transition from using their arm to using their core (knees to chest) musculature to increase throwing velocity. While advocated by some, we do not typically utilize hinged or varus elbow braces, given that the upper limb is a non-weight-bearing joint. This is reserved for the hyperactive child who just will not or cannot slow down. Typically, throwing is resumed once the patient demonstrates no pain, even with direct palpation over the capitellum, and full elbow motion symmetric to the opposite side. An interval throwing program is initiated, with emphasis on the “soreness rules,” which limit progression or advancement through pain. Patients and families are counseled that it may be many months until vigorous throwing (or gymnastics, etc.) can be resumed.29 This is not always an easy “sell,” but the risk of long-term arthritis needs to be kept in mind.30
 Medial Epicondyle Avulsion Fracture
Medial Epicondyle Avulsion Fracture
While further details regarding medial epicondylar fractures in children are provided in Chapter 29, a brief discussion is warranted here. In addition to the valgus compression forces on the lateral elbow resulting in elbow OCD, tensile forces on the medial elbow may result in avulsion fractures of the medial epicondyle in young throwers, gymnasts, wrestlers, cheerleaders, and other overhead athletes. With small avulsion fractures, the athlete will often indicate a particular moment (e.g., “sixth inning, clean-up batter at the plate for the other team, tying run on third, and I threw my best fastball and felt immediate pain”) that resulted in the injury. These fractures will heal with nonoperative management. Complete displacement of the entire medial epicondyle comes with macrotrauma (doing a floor routine in gymnastics with a fall). The displaced fractures may result in symptomatic valgus instability and altered flexor-pronator function in these high-demand athletes. For this reason, surgical reduction and fixation are recommended for displaced medial epicondyle fractures in young overhead or upper limb–weight-bearing athletes.
Table 41.1 Classification of elbow OCD lesions
While surgery may be performed in the prone position with the shoulder internally rotated to impart a varus-producing force on the elbow, our preference is to perform these procedures in the supine position with the limb supported by an operating hand table if the patient has enough external rotation at the shoulder to allow easy access to the posteromedial elbow. Positioning this way makes fluoroscopy a bit easier than prone or “sloppy lateral” positioning. We check for the shoulder passive range of motion under anesthesia before a final positioning decision is made. A nonsterile tourniquet is utilized. A longitudinal incision based upon the medial epicondyle and medial column of the distal humerus is made. Skin flaps are carefully raised, understanding that the course of the medial antebrachial cutaneous nerve (MABCN) is quite variable. The MABCN often runs with the more easily identifiable basilic vein and should be protected to avoid symptomatic numbness or neuroma formation. Deep dissection will allow for identification of the ulnar nerve. While it is unnecessary to dissect the ulnar nerve circumferentially, it is critical to localize and gently retract the nerve during bony fixation, particularly as a high percentage of young patients will exhibit asymptomatic ulnar nerve subluxation.31
Once the ulnar nerve is retracted and protected, direction is turned to the fracture. The medial epicondyle fragment is identified along with the attached origin of the flexor-pronator muscles. A 2-0 suture (Ethibond, Ethicon, Inc., Somerville, NJ) may be placed through the superior periosteum overlying the displaced fracture fragment to be used for traction during the case. The bony donor site is similarly identified and fracture hematoma and fibrous tissue are debrided. Under direct visualization, the fracture is reduced. This typically requires flexing the elbow and imparting varus stress while the forearm is pronated to relax the deforming forces. A threaded guide pin from the 3.5- or 4.5-mm cannulated screw set (Synthes, West Chester, PA) is placed into the medial epicondyle, across the fracture site, and up the medial column of the distal humerus; care is taken to place this guide pin in the center of the fracture fragment to avoid fragmentation of the typically small displaced epicondyle (Figure 41-5). A slick way to do this is drill the center of the medial epicondyle in the displaced position; with the drill bit just protruding from the fragment, anatomically reduce the fracture fragment; and then drill up the humerus obliquely avoiding the olecranon fossa. A second guide pin can be placed for temporary rotational control. Either a partially threaded cancellous screw or a fully threaded cortical screw can be used successfully. If a cancellous screw is used, and the fragment is big enough, then the central guide pin is overdrilled, and a partially threaded cannulated screw with a washer is placed, providing compression across the fracture site. Screw length is typically between 35 and 50 mm, and purchase of the far cortex is not necessary for adequate compression and fixation. If the fragment is smaller and there is concern about fragmentation with fixation, then a cortical screw and washer can be used. Cortical purchase is advised, but the screw needs to be removed sooner to prevent complications. Intraoperative fluoroscopy will confirm reduction, implant placement, and elbow stability. Suture repair of the flexor-pronator origin and periosteum increases stability and rotational control. The wound is closed in layers, and a long arm-bivalved cast is applied. Patients are transitioned into a hinged elbow brace by the second postoperative week to begin gentle range-of-motion exercises.

FIGURE 41-5 Postoperative anteroposterior (A) and lateral (B) radiographs following open reduction and internal fixation of a displaced medial epicondyle fracture.
A couple of technical pearls bear mention. First, anatomic fracture reduction can be challenging when performing the surgery in the supine position. The valgusextension position needed for visualization often impedes anatomic reduction. In addition to elbow flexion, forearm pronation, and varus stress, a dental pick or fracture reduction clamp may be helpful. (In our operating room, we have used a sterilized dinner fork with the central tines removed to facilitate fracture reduction and placement of the central guide pin). Alternatively, the drill hole in the epicondylar fragment and the medial column may be predrilled prior to reduction. Once the cannulated screw is placed into the fracture fragment, the screw tip may be inserted into the drilled medial column, using the screw itself to facilitate reduction. Second, it is important to remember that the medial epicondyle is a posterior structure. For this reason, the screw trajectory should be slightly posterior to anterior, and the lateral fluoroscopic image should demonstrate the posterior position of the screw head once fixation is complete. Failure to do so will result in nonanatomic fixation and suboptimal results.
 Arthroscopy and Drilling
Arthroscopy and Drilling
In patients with unstable OCD lesions with intra-articular loose bodies, arthroscopic loose body removal and drilling may be considered.1,32,33 Under general anesthesia in the supine position, the affected limb is suspended using either a commercially available limb positioning device or finger trap overhead traction (see Sidebar). After the elbow is insufflated with 10 to 15 mL of sterile saline solution via the direct lateral soft spot, a short 2.7-mm arthroscope is introduced into the joint via a proximal anteromedial portal. Arthroscopic survey is performed, and typically the loose body is immediately visualized in the anterior compartment (Figure 41-6A, B). Via an outside-in technique after first localizing with an 18-gauge spinal needle, an anterolateral portal is created just superior to the RC articulation (Figure 41-6C). An arthroscopic grabber is introduced and the loose body removed (Figure 41-6D, E). Following this, with varying degrees of elbow extension, the OCD lesion may be “unroofed” from the overlying radial head and probed. In cases in which inadequate visualization is achieved from a proximal anteromedial viewing portal, a direct lateral portal is created for viewing of the lesion.
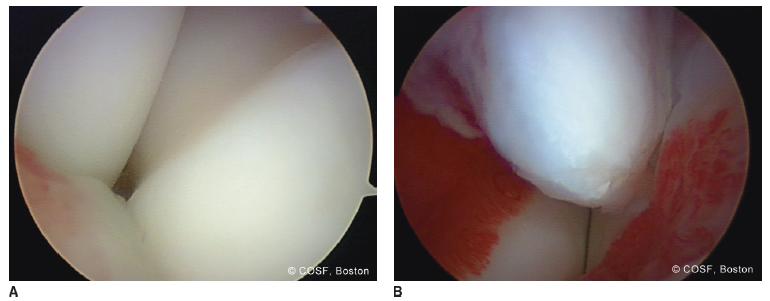
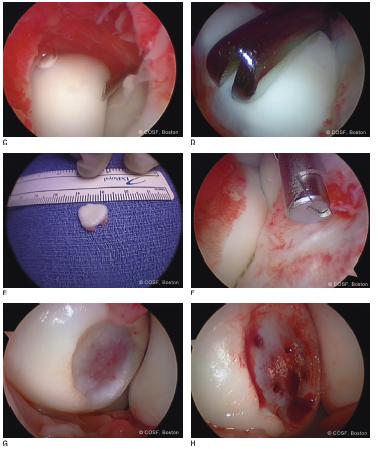
FIGURE 41-6 Arthroscopic treatment of an unstable OCD lesion. A: The lateral aspect of the elbow joint is visualized from the proximal anteromedial viewing portal in a right elbow. The trochlea is seen in foreground, the capitellum to the right, and the radial head to the left. B: A large intra-articular loose body is seen in the anterior compartment of the elbow. C: A spinal needle is used to localize an anterolateral working portal in an outside-in fashion. Note the surrounding synovitis of the anterior compartment. D: An arthroscopic grabber is used to remove the loose body. E: The loose body photographed after removal. F: Limited joint debridement is performed. G: The OCD lesion is easily visualized via an anconeus-splitting small arthrotomy. H: Following drilling/microfracture of the donor site, appropriate bleeding is seen.
Arthroscopy Setup, Portals, and Techniques
Arthroscopy is an invaluable tool for the pediatric hand and upper limb surgeon. While conceptualized almost 100 years ago, only with increased understanding of anatomy and surgical techniques has elbow arthroscopy become safe, reliable, and accepted in modern-day orthopaedics.64–66 Traditional indications for elbow arthroscopy included removal of intra-articular loose bodies, osteophyte debridement, and synovectomy. Over time, indications have expanded to include debridement of lateral epicondylitis, contracture release, drainage of infections, and treatment of OCD lesions. Further investigation has evaluated the role of arthroscopy in arthroscopic-assisted fracture reduction, nerve decompression, as well as instability surgery.
In general, elbow arthroscopy may be done in the supine, lateral, or prone positions. For most pediatric indications, in which the pathology lies in the anterior compartment, supine positioning confers a number of advantages (Figure 41-7). Anesthesia is more readily administered and monitored. Portal placement and instrumentation of the anterior compartment are easier in the supine patient. Furthermore, supine positioning allows for easy conversion to arthrotomy and open surgical reconstructions, particularly if a graft is to be harvested from the iliac crest or lower extremities. Prone positioning may be advantageous in the less frequent situations in which all work is to be done in the posterior compartment (e.g., posterior ulnohumeral impingement or valgus-extension overload in the throwing athlete).
While many have been proposed, a few workhorse portals are utilized in elbow OCD and other pediatric elbow conditions (Figure 41-8). The proximal anteromedial portal of Poehling serves as the primary viewing portal and is the first to be created.64 This portal is created 2 to 3 cm proximal to the medial epicondyle and just anterior to the palpable medial intermuscular septum. After skin incision, careful blunt dissection and spreading are performed in the subcutaneous tissues, with tactile confirmation that dissection proceeds anterior to the inter-muscular septum to avoid iatrogenic injury to the ulnar nerve. A small joint arthroscope is then inserted, directed toward the radial head, and skived along the anterior surface of the distal humerus. This portal allows excellent and immediate visualization of the RC joint and OCD lesions.

FIGURE 41-7 Supine positioning for elbow arthroscopy. A: The limb may be supported via finger trap suspension over an operating hand table. B: Alternatively, arthroscopy may be performed without the hand table present, which allows for closer proximity and easier maneuvering about the elbow. An arm board or hand table may be placed later if an open procedure is to be performed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


