Fig. 38.1
Clinical photograph showing a child with splenomegaly
A number of infections and diseases can contribute to splenomegaly. These include:
Viral infections, such as infectious mononucleosis
Bacterial infections, such as syphilis or subacute bacterial endocarditis
Parasitic infections, such as malaria
Cirrhosis and other diseases affecting the liver
Various types of hemolytic anemia—a condition characterized by premature destruction of RBCs
Blood cancers, such as leukemia, and lymphomas, such as Hodgkin’s disease
Metabolic disorders, such as Gaucher’s disease and Niemann–Pick disease
Pressure on the veins in the spleen or liver (liver cirrhosis) or thrombosis in these veins (portal vein thrombosis)
Massive Splenomegaly
This describes a spleen that weighs more than 1000 g (Fig. 38.2) .
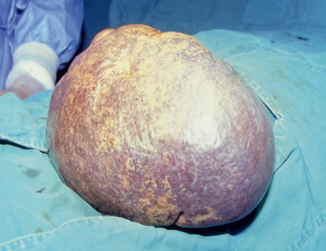
Fig. 38.2
Intraoperative photograph showing massive splenomegaly
Causes: chronic myeloid leukemia, Gaucher’s disease, hairy cell leukemia, marginal zone B cell lymphoma, myelofibrosis, plasmacytoma, and prolymphocytic leukemia.
Splenic Rupture
Splenic rupture is due to blunt trauma, penetrating trauma, or abdominal surgery.
Only rarely ruptures occur spontaneously (associated with infectious mononucleosis, malaria, typhoid fever, leukemia/lymphoma, other tumors, subacute bacterial endocarditis, peliosis lienis, acute splenitis, and pregnancy).
Splenosis
Splenosis is a condition where foci of splenic tissue undergo autotransplantation, most often following trauma or splenectomy .
Displaced tissue fragments can implant on well-vascularized surfaces in the abdominal cavity, or, if the diaphragmatic barrier is broken, the thorax.
The spleen can regenerate through various mechanisms. Autotransplantation of splenic tissue after traumatic disruption of the splenic capsule is well recognized. Splenic tissue can lodge anywhere in the peritoneal cavity following traumatic disruption and regenerates under favorable conditions.
The incidence of splenic regeneration correlates with the severity of splenic injury. Patients requiring a splenectomy for trauma tend to be those with the greatest splenic damage and dissipation of splenic tissue, which favors autotransplantation.
They are supplied by newly formed arteries that penetrate the capsule .
Accessory Spleen
An accessory spleen (supernumerary spleen, splenule, or splenunculus) is a small nodule of splenic tissue found apart from the main spleen .
Accessory spleens are found in approximately 10 % of the population and in 20–30 % of autopsies.
Accessory spleens are typically around 1 cm in diameter but may reach up to 4 cm.
They form either by the result of developmental anomalies or trauma .
Accessory spleens resemble normal spleen macroscopically and microscopically.
They may be found anywhere:
Along the splenic vessels
In the gastrosplenic ligament
In the splenorenal ligament
In the walls of the stomach or intestines
In the pancreatic tail
In the greater omentum, the mesentery or the gonads and their path of descent (Fig. 38.3)
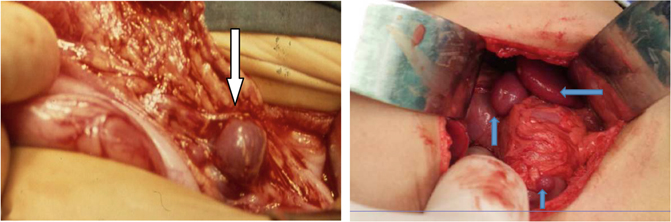
Fig. 38.3
Intraoperative photograph showing a spleniculi and intraoperative photograph showing multiple accessory spleens
An accessory spleen derives its blood supply from branches of the splenic artery.
The presence of spleniculi is important to document or find in patients at the time of splenectomy for hematologic diseases specially patients with idiopathic thrombocytopenic purpura (ITP).
These accessory spleens can enlarge following splenectomy and be the source of recurrent symptoms in those operated on for hematological disorders (Fig. 38.4) .

Fig. 38.4
a CT scan of the abdomen showing an enlarged spleniculi in a patient with congenital asplenia. This spleniculi enlarged and became ischemic causing abdominal pain. b and c, A clinical photograph showing an enlarged spleniculi that was removed. Note that macroscopically it resembles a normal spleen
Asplenia (Congenital Absence of Spleen)
Congenital absence of the spleen is very rare .
It is associated with other malformations including:
Cardiac malformations (80 %, usually involving atrioventricular endocardial cushion and ventricular outflow tract)
Situs inversus
Anomalies of blood vessels, lung, and abdominal viscera
Hepatolienal Fusion
This is a very rare condition in which there is fusion of liver and spleen .
Polysplenia
Polysplenia is the presence of multiple spleens. This is commonly associated with extrahepatic biliary atresia (Fig. 38.5) .
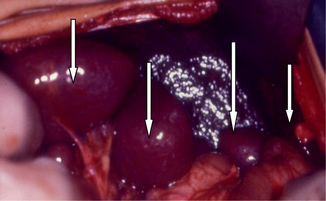
Fig. 38.5
Intraoperative photograph in a patient with biliary atresia and polysplenia
Splenogonadal Fusion
Splenogonadal fusion is a rare congenital anomaly in which ectopic splenic tissue unites with a gonad and can result in one or more accessory spleens along a path from the abdomen into the pelvis or scrotum .
Splenogonadal fusion is divided into two types: continuous or discontinuous.
Continuous: The spleen is connected to ectopic splenic mass by cord of splenic and/or fibrous tissue that is connected to the gonad.
Discontinuous: There is no connection between the spleen and ectopic splenic mass which unites with a gonad.
Ninety percent occurs in males and usually on the left sided.
Twenty percent of continuous types are associated with other congenital defects, including:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


