Substance use during pregnancy is at least as common as many of the medical conditions screened for and managed during pregnancy. While harmful and costly, it is often ignored or managed poorly. Screening, brief intervention, and referral to treatment is an evidence-based approach to manage substance use. In September 2012, the US Centers for Disease Control and Prevention convened an Expert Meeting on Perinatal Illicit Drug Abuse to help address key issues around drug use in pregnancy in the United States. This article reflects the formal conclusions of the expert panel that discussed the use of screening, brief intervention, and referral to treatment during pregnancy. Screening for substance use during pregnancy should be universal. It allows stratification of women into zones of risk given their pattern of use. Low-risk women should receive brief advice, those classified as moderate risk should receive a brief intervention, whereas those who are high risk need referral to specialty care. A brief intervention is a patient-centered form of counseling using the principles of motivational interviewing. Screening, brief intervention, and referral to treatment has the potential to reduce the burden of substance use in pregnancy and should be integrated into prenatal care.
Related editorial, page 537 .
Introduction
Substance use is common in women of childbearing age. Prior to pregnancy, approximately 55% of women drink alcoholic beverages, 23% smoke cigarettes, and 10% use either illicit drugs or prescription drugs without a prescription. Although most women are able to quit or cut back harmful substances during pregnancy, many are unwilling or unable to stop. National survey data indicate that during pregnancy, 10% of women drink alcohol (4% binge, ie, had ≥5 alcoholic drinks on the same occasion on at least 1 day in the past 30 days), 15% smoke cigarettes, and 5% use an illicit substance. This makes substance use as or more common than many conditions routinely screened for and assessed during prenatal care (PNC), such as cystic fibrosis, gestational diabetes, anemia, postpartum depression, or preeclampsia. Moreover, substance use during pregnancy is both costly and harmful. Substance use during pregnancy is associated with poor pregnancy outcomes, including preterm birth, low birthweight, birth defects, developmental delays, and miscarriage. Long-term effects on the mother and infant include medical, legal, familial, and social problems, some of which are lifelong and costly.
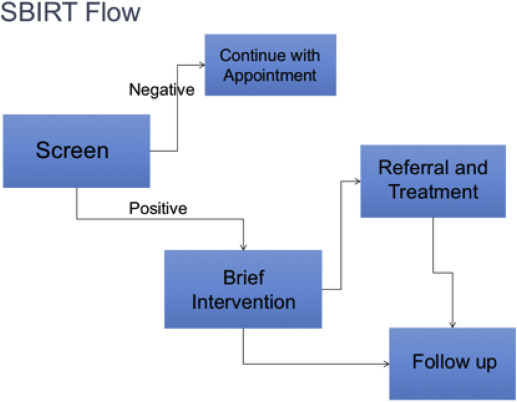
The perinatal provider, therefore, has an important medical and ethical role in screening for substance use, counseling women on the importance of avoiding harmful substances, supporting their behavioral change, and referring women with addiction to specialized treatment when needed. This process, known as screening, brief intervention (BI), and referral to treatment (SBIRT), represents a public health approach to the delivery of early intervention and treatment services for persons with substance use disorders (SUD) ( Table 1 ). Its use in emergency, general primary care, and obstetric settings for alcohol and tobacco has been recommended by the US Preventive Services Task Force as well as by professional societies such as the American Congress of Obstetricians and Gynecologists (ACOG).
| Component | Goal | Approach |
|---|---|---|
| Screening | Assess substance use and its severity | Patient-/computer-administered instrument or direct provider questions ( Table 4 ) |
| Brief intervention | Increase intrinsic motivation to affect behavioral change (ie, reduce or abstain from use) | 1–5 Patient-centered counseling sessions lasting <15 min using principles of motivational interviewing ( Table 2 ) |
| Referral to treatment | Provide those identified as needing more treatment access to specialty care | Warm handoff to specialized treatment (eg, provider-to-provider telephone call), which requires practitioner familiarity with community resources and systems of care |
Unfortunately, a number of barriers has limited the public health impact of SBIRT, particularly during pregnancy. First, although universal screening for substance use is recommended during pregnancy, many women are not screened or not screened with evidence-based screening tools. Providers are often overwhelmed by the number of disease states for which they are expected to screen and/or feel inadequately trained to screen for substance use. Clinicians may also question the clinical utility of screening and the likelihood that women will reduce substance use or attain abstinence; conversely, they may be under the impression that they do not have patients who use substances in their practices or may not want to “play police” due to mandatory reporting requirements in some states. In addition, providers may be at a loss of what to do if they encounter a patient with a SUD or unsure how to help the patient if unaware of community resources for treatment. Finally, inadequate reimbursement for evaluation and management services is a disincentive to provide preventative care even in the case of pregnant women.
Second, failure to disclose substance use (or incomplete disclosure) is also common, and further complicates efforts to identify at-risk women. Pregnant women also have reasons to withhold information about their use of substances in pregnancy. Some states have mandatory reporting requirements with the possibility of incarceration in a minority of states. This may not only create a disincentive for disclosure, but possibly for treatment-seeking itself. Women may also be concerned about prejudicial treatment and stigma from their physicians who should be their advocates, while pregnant youth may fear disclosure to family members and the possible consequences of such disclosure.
Third, SBIRT research and practice has traditionally focused on the more commonly used substances such as alcohol and tobacco, with relatively less focus on illicit drugs. This gap has become particularly apparent and troubling as rates of prescription drug misuse in pregnancy have risen steadily in recent years, leading to almost 3-fold increases in the incidence of neonatal abstinence syndrome from 2000 through 2009. This increase has prompted calls for urgent action to help limit prescription opioid use and misuse during pregnancy.
In response to these calls, the US Centers for Disease Control and Prevention (CDC) convened an Expert Meeting on Perinatal Illicit Drug Abuse in Atlanta, GA, in September 2012. The expert panel participants were chosen based on their experience and past work specifically related to the use of the SBIRT approach in pregnant women. About 40 clinicians, scientists, and public health professionals representing academia (Johns Hopkins University, Harvard Medical School, Yale University, University of North Carolina, University of Maryland, University of Hawaii, and Wayne State University), professional organizations (ACOG and American Academy of Pediatrics [AAP]), states (Massachusetts, Washington, Georgia, and Indiana) and federal agencies (CDC, National Institutes of Health [NIH], Substance Abuse and Mental Health Services Administration [SAMHSA], Human Resources and Services Administration, and the Food and Drug Administration) were present at the meeting. This article represents the formal conclusions from that meeting, presented below within each of the 3 major elements of SBIRT for drug use in the perinatal period.
Screening
Screening for substance use should be universal, as SUDs occur in every socioeconomic class, and racial and ethnic group. Moreover, screening based on risk factors such as late entry to PNC or prior poor birth outcome potentially leads to missed cases and can exacerbate stigma and stereotyping. Universal screening is recommended by many professional organizations, including ACOG, AAP, American Medical Association (AMA), and CDC. Screening should be done at the first prenatal visit, and repeated at least every trimester for individuals who screen positive for past use ( Table 2 ). In addition, screening for tobacco use, at-risk drinking, illicit drug use, and prescription drug misuse should occur on an annual basis as a part of routine well-woman care. Women should be asked at medical exams if they are planning to get pregnant in the next year, so that adequate contraception and preconception care can be provided. Conclusions regarding screening are summarized in Table 3 .
| Raise subject |
|
| Provide feedback |
|
| Enhance motivation |
|
| Negotiate plan |
|
|
Most of the studies looking at screening have focused on using instruments, such as TWEAK, T-ACE, 4P’s, or AUDIT-C ( Table 4 ). These instruments have the advantage of being validated and most are fairly sensitive. Also, preliminary screening can be done by anyone in the practice, with follow-up by the provider. Barriers to implementing instrument-based screening include patient discomfort and lack of literacy, staff resistance due to time pressures, and organizational issues such as lack of administrative support. Integration into practice flow can be eased by incorporation into electronic medical record systems or by using a computer-based approached, which may diffuse the discomfort women feel in disclosing a behavior about which they are embarrassed, but this has not been compared to clinician-administered screening in pregnant women. All positive screens require follow-up by the provider.
| Instrument | Substance | Validated in pregnancy | Subjects identified |
|---|---|---|---|
| CAGE | Alcohol | No | At-risk drinking |
| Cut down | |||
| Annoyed | |||
| Guilt | |||
| Eye opener | |||
| T-ACE | Alcohol | Yes | At-risk drinking |
| Takes | |||
| Annoyed | |||
| Cut down | |||
| Eye opener | |||
| TWEAK | Alcohol | Yes | At-risk drinking |
| Tolerance | |||
| Worry | |||
| Eye opener | |||
| Amnesia | |||
| Cut down | |||
| 4Ps a | Any substance | Yes | Any affirmative answer is considered positive screen |
| Past | |||
| Present | |||
| Parents | |||
| Partner | |||
| Substance Use Profile-Pregnancy | Alcohol Illicit drugs | Yes | Any drinking or illicit drugs |
a Modifications of 4Ps screener are available; eg, 5Ps (adding smoking) and 4Ps Plus, which is copyrighted and requires yearly fee to use.
To counteract some of the institutional barriers to instrument-based screening, some experts encourage simply asking 3 open-ended questions regarding use of tobacco, alcohol, and other drugs (NIDA Quick Screen) : “In the past year how many times have you drunk >4 alcoholic drinks per day? Used tobacco? Taken illegal drugs or prescription drugs for nonmedical reasons?” Among the expert panel, the consensus was that these questions are likely sensitive with fairly good specificity. Women are also more likely to report lifetime use or use before pregnancy than they are to disclose use during pregnancy because of the risks and stigma involved.
Regardless of which method is used and how the screening is delivered, it is essential that conversations around substance use be nonjudgmental. Prefacing screening with statements such as “I ask all my patients about substance use” can help normalize the enquiry and increase patient comfort with disclosure. The process of screening is only the first step in a conversation with the patient that may lead to treatment referral or provision of other treatment resources.
Urine drug testing is a common practice for many obstetricians and family practice physicians. It does have the advantage of detecting use in cases where the woman does not disclose her use and may help in diagnosing neonatal abstinence syndrome. Toxicology testing is a useful adjunct for individuals in SUD treatment and has utility at the time of delivery in case of complications of pregnancy, where knowing the substance used informs management decisions. Toxicology testing of pregnant women also has a number of limitations and negative consequences and should therefore never be done without the woman’s knowledge or consent. For example, it greatly increases the risk of legal or child welfare involvement, particularly in states with mandated reporting requirements that include mention of drug use during pregnancy. This places physicians in a difficult ethical position, and raises the likelihood that women will fail to disclose potential health risks or avoid recommended medical care. Further, the reporting of drug use during pregnancy to child welfare–made more likely or even mandated as a result of positive toxicology–is strongly biased against racial and ethnic minorities, even following concerted efforts to prevent such bias. A positive toxicology test also shows evidence of use, but does not provide any information about the nature or extent of that use; similarly, a negative test does not rule out substance use, which is often sporadic. Additionally, the consequences of false-positive results can be devastating to the woman and her family.
Finally, the use of toxicological testing for illicit drugs encourages a focus on substances such as cocaine, opiates, and marijuana that is not justified by their prevalence or the risk that they pose. Other substances such as tobacco and alcohol pose as much or more risk and are far more prevalent ; similarly, other risk factors such as inadequate PNC, depression, or violence exposure present significant unique risks that should be acknowledged–and that are not amenable to toxicology testing. If drug testing is used, a discussion of all substances and medications taken is mandatory as it will allow the clinician to order the correct test(s). Many substances including synthetic opioids such as oxycodone, fentanyl, buprenorphine, and some benzodiazepines are not routinely captured by standard urine tests, and, if suspected, must be ordered separately. In addition, regular urine drug screens do not pick up alcohol use, and tests for alcohol metabolites, such as ethyl glucuronide and ethyl sulfate, are not routine, nor well studied in pregnant women. For these reasons, the expert panel did not endorse using urine drug testing as a primary means to screen women for drug use during pregnancy.
Clinicians who do use urine drug testing should ensure that all positive drug tests are followed by confirmatory testing by mass spectrometry. The health care provider should be aware of the potential for false-positive and false-negative results of urine toxicology for drug use, the typical urine drug metabolite detection times, and the legal and social consequences of a positive test result. It is incumbent on the health care provider, as part of the procedure in obtaining consent before testing, to provide information about the nature and purpose of the test to the patient and how the results will guide management.
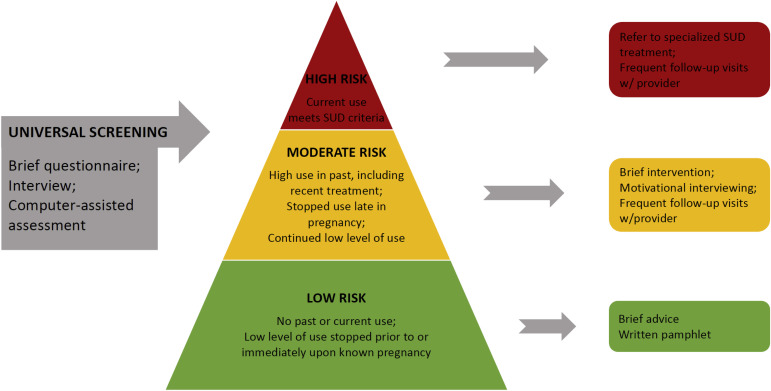
The overarching purpose of screening for substance use is to stratify women into zones of risk given their pattern of use. Based on the consensus of the group and available literature on drug use in pregnancy, we developed the risk pyramid shown in Figure 1 . The majority of women will fall into the low-risk zone (ie, no past use of tobacco, alcohol, or other drugs, or low levels of substance use that stopped prior to or immediately following knowledge of pregnancy) and will need only brief advice/reinforcement. Moderate-risk women are those who have used high quantities of (any) substances in the past (including those who have been recently treated for SUDs), those who stopped during pregnancy, and those with sporadic, low-level use during pregnancy. Per the consensus of the group, these are the women who benefit most from BI. Only about 4-5% of women will fall into the high-risk zone of continued use of illicit drugs during pregnancy. Women in the high-risk zone meet criteria for SUD. While these women can benefit from BI, most need referral to specialized addiction treatment. Figure 2 illustrates the flow of SBIRT in clinical practice.
Screening
Screening for substance use should be universal, as SUDs occur in every socioeconomic class, and racial and ethnic group. Moreover, screening based on risk factors such as late entry to PNC or prior poor birth outcome potentially leads to missed cases and can exacerbate stigma and stereotyping. Universal screening is recommended by many professional organizations, including ACOG, AAP, American Medical Association (AMA), and CDC. Screening should be done at the first prenatal visit, and repeated at least every trimester for individuals who screen positive for past use ( Table 2 ). In addition, screening for tobacco use, at-risk drinking, illicit drug use, and prescription drug misuse should occur on an annual basis as a part of routine well-woman care. Women should be asked at medical exams if they are planning to get pregnant in the next year, so that adequate contraception and preconception care can be provided. Conclusions regarding screening are summarized in Table 3 .
| Raise subject |
|
| Provide feedback |
|
| Enhance motivation |
|
| Negotiate plan |
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


