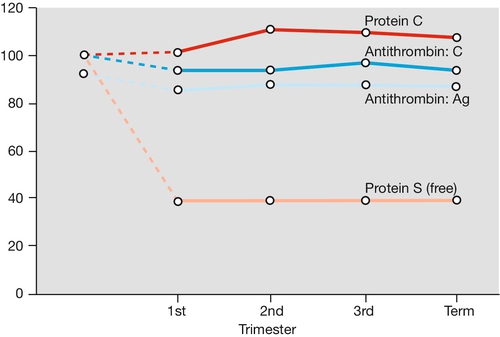
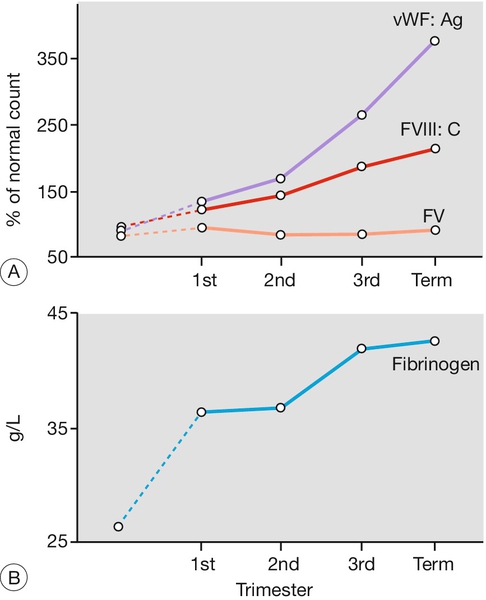
28 Pregnancy brings huge physiological changes and, from a developmental point of view, it is assumed that these changes are in the fetal interest. The changes are proactive; in other words, they are not proportional to the size of the fetus, such that by the end of the first trimester, many systems are functioning at levels close to those at term. The systems are reviewed in order below. Oxygen consumption is increased by around 15–20%. The requirement for this is partly maternal – to satisfy the increase in cardiac output, renal function and other metabolic requirements, including respiratory function, breast and uterine development. Around 40% of the increased oxygen requirement is for the fetoplacental unit. To supply this increased oxygen requirement, the mother hyperventilates, increasing minute ventilation by about 40% above the normal 7 L/min. This increase in ventilation is far greater than the increase in oxygen consumption, effectively providing a safety net. The increase is predominantly achieved by increasing tidal volume rather than respiratory rate – in other words, the mother breathes more deeply. This is more efficient than increasing the respiratory rate, as there is less dead-space movement (i.e. that air which is outwith the alveoli and hence not involved in gas exchange). Maternal serum CO2 falls, favouring CO2 transfer from the fetus to the mother. These changes are thought to be mediated by progesterone, as a smaller but similar effect is noted in patients taking progestogen-containing contraceptives. Breathlessness is a common symptom in pregnancy. This dyspnoea is perceptual rather than a reflection of inadequate gas exchange, and is often worse at rest. In late pregnancy, the gravid uterus may restrict diaphragmatic movement, exacerbating any feelings of breathlessness. Nevertheless, it is important to consider pathological causes of breathlessness, particularly pulmonary thromboembolic disease. In pregnancy, there is an increase in cardiac output and a decrease in peripheral vascular resistance. Cardiac output rises by about 40%, from around 3.5 L/min to 6 L/min, from increases in both stroke volume and cardiac rate. As with the respiratory system, these changes are disproportionately greater than required. The fall in peripheral vascular resistance mediated by vasodilatation is not quite compensated for by the increased cardiac output, so the overall effect is a slight fall in blood pressure in the second trimester, sometimes by as much as 5 mmHg systolic and 10 mmHg diastolic. The blood pressure may rise slightly again in the third trimester and it may be difficult to separate this from the pathological state of pre-eclampsia. The hyperdynamic circulation of pregnancy can often reveal functional flow murmurs, which are usually of little clinical significance. This high blood flow maximizes PO2 on the maternal side of the placenta and maximizes oxygen transfer to the fetal circulation. The plasma volume expansion and increased cardiac output may also help heat loss by increasing blood flow through the skin, thus compensating for the increased metabolic rate of pregnancy. Peripheral vasodilatation causes a feeling of warmth and a tolerance to cold, and may be a factor in the palmar erythema and spider naevi of pregnancy. The cardiac output may rise by a further 2 L/min in established labour; this results from an increase in heart rate and stroke volume. Following delivery the uterus contracts, reducing cardiac output to 15–25% above normal, which over the next 6 weeks gradually returns to the pre-pregnancy state. Late in pregnancy, the mass of the uterus is liable to press on, and partially occlude, the inferior vena cava. This reduced venous return leads to a reduced cardiac output and may lead to hypotension, so-called ‘supine hypotension’. The clinical importance of this is such that women in later pregnancy and in labour should not lie flat and, ideally a wedge or other device should be employed to allow the woman to lie at a slight tilt. Supine hypotension often results in a sensation of nausea but even in the absence of this, may be associated with fetal heart rate abnormalities. All women undergoing caesarean section, elective or emergency, should be placed on an operating table capable of a 15º lateral tilt. On average, the total red cell mass increases steadily throughout the pregnancy by 25%, from around 1300–1700 mL. The circulating plasma volume, however, increases by 40%, from around 2600–3700 mL. Because the plasma volume increases proportionately, more than red cell mass, there is a dilutional drop in the haemoglobin concentration and in the haematocrit, such that a haemoglobin level of 105 g/L would be normal in a healthy pregnancy. Plasma colloid osmotic pressure falls in pregnancy; as a result, fluid shifts into the extravascular compartment, causing oedema. Around 80% of pregnant women have some degree of dependent oedema. The typical changes in the full blood count in pregnancy are shown in Table 28.1. Iron requirements are increased (Table 28.2) to meet the requirements of the larger red cell mass, developing fetus and the placenta, and the serum ferritin level therefore falls. The fetus gains iron from maternal serum by active transport across the placenta, mostly in weeks 36–40. In the absence of iron deficiency, routine supplementation is not recommended. Nevertheless, iron deficiency is not rare particularly if iron stores are low before pregnancy. A high index of suspicion is required to aid diagnosis, particularly in at-risk populations and among resource deficient populations. The World Health Organization (WHO) has suggested iron supplementation at haemoglobin levels below 105 g/L. Table 28.1 Blood changes in pregnancy ESR, erythrocyte sedimentation rate; MCH, mean corpuscular haemoglobin: MCHC, mean corpuscular haemoglobin concentration; MCV, mean corpuscular volume. Table 28.2 The requirements of elemental iron during pregnancy The daily folate requirement rises from 50 μg to 400–600 μg, and folate deficiency may occur. It is usually possible to meet this increased requirement through a normal diet, although intake in those with a poor diet is likely to be inadequate. Daily folic acid supplementation from before conception reduces the risk of neural tube defects. Pregnancy is a hypercoagulable state, with an increase in procoagulants (particularly fibrinogen, but also platelets, factor VIII, von Willebrand factor) and a reduction in naturally occurring anticoagulants (e.g. protein S and antithrombin). Fibrinolysis is also increased, so there is an increased net turnover of coagulation factors (Figs 28.1 and 28.2). Fibrinolytic activity returns to normal within 1 h of placental delivery, suggestive that inhibition of fibrinolysis is mediated by the placental unit. FV, factor V.
The physiology of pregnancy
Introduction
Respiratory system
Cardiovascular system
Blood, plasma and extracellular fluid volume
Blood constituents and anaemia
Non-pregnant
Pregnant
Haemoglobin (g/L)
120–140
100–120
Red cell count (× 1012/L)
4.2
3.7
Haematocrit (venous)
40%
34%
MCV (fl)
75–99
80–103
MCH (pg)
27–31
No change
MCHC (g/dL)
32–36
No change
White cell count (× 109/L)
4–11
9–15
Platelets (× 109/L)
140–440
100–440
ESR (mm/h)
< 10
30–100
Fetus and placenta
500 mg
Red cell increment
500 mg
Postpartum blood loss and 6 months’ lactation
360 mg
Total
1360 mg
Saving from amenorrhoea approximately
360 mg
Net increased demand approximately
1 g
Folate metabolism
Haemostasis in pregnancy
Obgyn Key
Fastest Obstetric, Gynecology and Pediatric Insight Engine