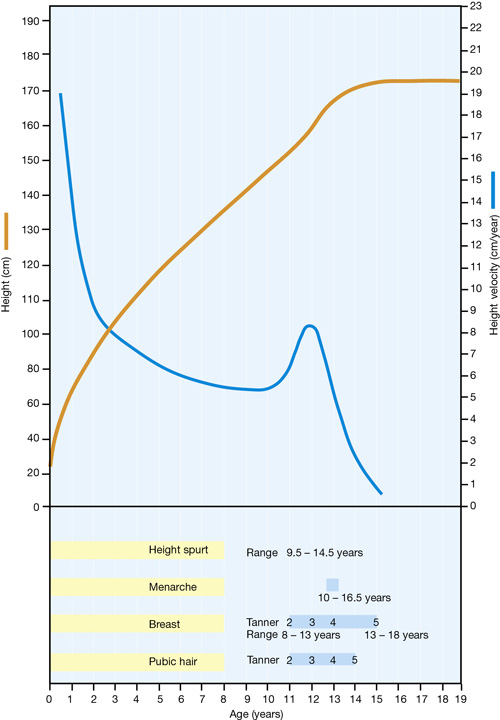
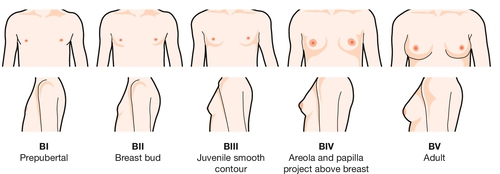
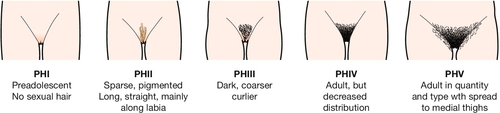
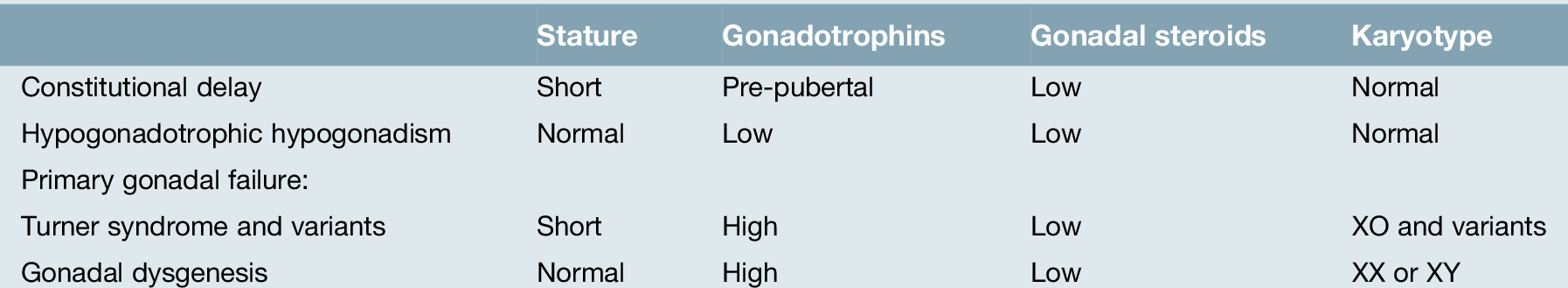
5 Puberty should transform a girl into a fertile woman, and its social importance is so great that any deviation from normality may be the cause of considerable embarrassment and anxiety. This chapter describes normal puberty and outlines the management of both delayed puberty and precocious puberty. There is also a short discussion about sexual abuse. Puberty encompasses: Puberty begins with the reactivation of the hypothalamo–pituitary–ovarian axis, which has lain dormant from the 3rd or 4th month of postnatal life. During childhood, the hypothalamus and pituitary are highly sensitive to suppression by low levels of gonadal steroids. With the onset of puberty, this extreme sensitivity is lost. The first recognized endocrine event is the appearance of sleep-related, pulsatile release of gonadotrophins. As puberty progresses, these extend throughout the 24 h of the day. These gonadotrophins lead to production of ovarian oestrogen, which initiates the physical changes of puberty. Changes in the ovaries are evident at an early stage. In normal girls, before any physical signs of puberty are apparent, ultrasonography demonstrates a progressive increase in the size of ovarian follicles, such that after the age of The external signs of puberty usually (but not always) occur in a specific order (Fig. 5.1). The onset of the adolescent growth spurt is an early feature of puberty in girls and this acceleration in growth is dependent on growth hormone as well as gonadal steroids. Almost at the same time, the subareolar breast bud appears (thelarche). Breast development, which is primarily under the control of ovarian oestrogens, is described in five stages (Fig. 5.2). The appearance of the breast bud is followed shortly afterwards by pubic and axillary hair (pubarche), mainly under the influence of ovarian and adrenal androgens (Fig. 5.3). Menarche is a late feature in the course of puberty. Since the turn of the 20th century, the average age for the onset of puberty has become progressively younger. In 1900, the average age of the menarche was approximately 15.5 years, while currently, it is 12.8 years. This has been attributed to improvement in socioeconomic conditions, nutrition and general health. This trend appears to have slowed or ceased in Western Europe and the USA during the past 30 years, as might be expected once nutrition and child care had reached an optimum level. It had previously been proposed that the menarche was closely related to the attainment of a critical body weight, which in the USA and Europe was approximately 48 kg. Further analysis suggested that the significant component of body weight was body fat, which during the adolescent growth spurt increases to about 22% of body weight. This converts a lean body weight-to-fat ratio of 5:1 at the initiation of the growth spurt to one of 3:1 at the menarche. Factors which delay the attainment of a critical body weight may delay the menarche. These include: Some 95% of normal girls attain stage 2 breast development (the appearance of the subareolar breast bud) by the age of 13.2 years; 50% will complete all stages of puberty in 2–3 years, while 97% will do so in 5 years. The bone age, which is an index of physiological maturation, correlates closely with the menarche. It can be measured by an X-ray of the hand. A total of 80% of girls begin to menstruate at a bone age of 13–14 years. After the menarche, menstrual cycles tend to be irregular, as ovulation is initially infrequent. Most girls take several months or even as long as 2–3 years to establish a regular cycle. Delayed puberty in girls may be defined as the absence of physical manifestations of puberty by the age of 13 years. Primary amenorrhoea is defined as no menstruation by the age of 14 years, accompanied by failure to develop secondary sexual characteristics. It is also defined as no menstruation by the age of 16 years in the presence of normal sexual development, and this is discussed further in Chapter 6. In some instances, a girl may enter puberty but the normal progression is not maintained. This is described as ‘arrested puberty’. These features of delayed puberty fall into three main categories (Table 5.1).
Paediatric gynaecology
Introduction
Normal puberty
![]() an adolescent growth spurt
an adolescent growth spurt
![]() the acquisition of secondary sexual characteristics
the acquisition of secondary sexual characteristics
![]() the onset of menstruation (menarche)
the onset of menstruation (menarche)
![]() the establishment of ovulatory function.
the establishment of ovulatory function.
Endocrine changes
 years a multicystic appearance of the ovaries (defined as more than six follicles > 4 mm in diameter, in each ovary) can often be demonstrated.
years a multicystic appearance of the ovaries (defined as more than six follicles > 4 mm in diameter, in each ovary) can often be demonstrated.
Signs of puberty
Age of menarche
Influence of body weight
![]() malnutrition
malnutrition
![]() slow growth before and after birth
slow growth before and after birth
![]() twins, who have a later menarche than singletons of the same population
twins, who have a later menarche than singletons of the same population
![]() athletic training, as it results in an increased proportion of lean body mass at the expense of adipose tissue; for each year of premenarcheal training, the menarche is delayed by 5 months
athletic training, as it results in an increased proportion of lean body mass at the expense of adipose tissue; for each year of premenarcheal training, the menarche is delayed by 5 months
![]() eating disorders; anorexia nervosa in particular can cause both primary and secondary amenorrhoea and a halt in pubertal progress.
eating disorders; anorexia nervosa in particular can cause both primary and secondary amenorrhoea and a halt in pubertal progress.
![]() environmental factors may also play a role; urban communities tend to have an earlier menarche than rural communities, as do girls from social class I when compared with girls from social classes II and III.
environmental factors may also play a role; urban communities tend to have an earlier menarche than rural communities, as do girls from social class I when compared with girls from social classes II and III.
Progression through puberty
Delayed puberty
Definition
Causes of delayed puberty
Constitutional delay
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree