The Pharynx and Upper Airway
Marshall E. Smith
ORAL CAVITY AND OROPHARYNX
 EMBRYOLOGY
EMBRYOLOGY
The oral cavity begins as a depression that invades into the developing embryo. It invaginates until the ectoderm of the stomodeum contacts the endoderm of the primitive foregut, creating the buccopharyngeal membrane. This membrane degenerates at 4 weeks of gestation, providing continuity between the ectodermally derived oral cavity and the endodermally derived oropharynx. The five branchial arches are mesodermal condensations on the lateral cervical area of the embryo and are separated by branchial clefts externally and branchial pouches internally. The cleft is ectodermally lined, whereas the pouch is endodermally lined. The first arch develops into the mandible, the portions of the ossicles, and the muscles associated with these structures. The second arch contributes to portions of the ossicles, the styloid process, the portions of the hyoid bone, the facial muscles, the posterior belly of the digastric muscle, and the buccinator muscles. The third arch differentiates into portions of the hyoid bone and pharyngeal muscles. The fourth arch develops into the anterior/superior portions of the larynx. Finally, the fifth arch contributes to the posterior, larynx, cricoid, and intrinsic muscles of the larynx and the inferior pharyngeal constrictor muscle.
The pharyngeal pouches produce a variety of structures. The first pouch becomes the middle-ear cavity. The first branchial cleft creates the external ear canal. The tonsils are formed from contributions from both the first and second pouches invading into the surrounding mesoderm. Between the third and fifth months of gestation, lymphatic tissue then invades these primitive structures. The third pouch gives rise to the thymus gland and the inferior parathyroid glands. The fourth pouch develops into the thyroid gland and the superior parathyroids.
The hard palate is divided into a primary and secondary palate. The primary palate contains the anterior alveolus and the four upper incisors and is derived from the medial nasal swelling. The secondary palate (the area posterior to the incisive canals) is formed by the medial growth of the lateral palatine processes of the maxilla. The primary palate is completely developed by the seventh week of gestation, and the secondary palate completes its fusion between weeks 10 and 12 of gestation. Clefts of the soft palate are generally associated with clefts of the secondary hard palate. Complete clefts involve the primary, secondary, and soft palate structures.
The anterior two thirds of the tongue are derived from ectoderm, whereas the posterior one third is derived from endoderm of the primitive foregut. Swellings begin to condense during the fourth week of gestation and are complete by the seventh week. The fungiform and filiform papillae develop by the 11th week, and the circumvallate papillae develop between weeks 8 and 20. The floor of the mouth is a first arch derivative. The salivary glands are of ectodermal origin and are derived from the first pouch, developing between weeks 5 and 8.
 ANATOMY
ANATOMY
Oral Cavity The oral cavity is surrounded anteriorly by the lips. The lips are supplied with a rich sensory innervation and fine-motor control to provide a complex sphincter mechanism. The lips function to prevent the loss of saliva and food materials from the oral cavity and are instrumental in producing labiodental and plosive speech sounds. Loss of sensation interferes with the protective function of the labial sphincter, often causing sialorrhea and mild feeding problems. The dental arches support the teeth and gingival mucosa, which cover the alveolar ridges. The lingual frenulum divides the floor of the mouth in the midline. The geniohyoid, mylohyoid, genioglossus, and hyoglossus muscles support the floor of the mouth.
The Tongue The tongue is an important structure for communication and mastication. Fine-motor abilities of the tongue permit proper articulation for speech and provide the necessary manipulation of food materials. The tongue is divided into an anterior two thirds (which lie within the oral cavity) and a posterior one third (which lies within the oropharynx). The division between these two areas is demarcated by the large circumvallate papillae that form a V, with the apex posteriorly at the foramen cecum. The foramen cecum is an embryologic derivative of the thyroid gland. If the thyroid gland fails to descend, a lingual thyroid may be visible on the dorsum of the tongue in this area. The tongue’s mucosal covering is composed of a mixture of papillae. In addition to the circumvallate papillae, smaller fungiform papillae are located on the lateral aspects and on the tip of the tongue. The filiform papillae are the most abundant and cover the dorsum of the tongue. Taste buds are abundant on the circumvallate and fungiform papillae. The filiform papillae contain no taste buds.
The tongue’s musculature is composed of intrinsic and extrinsic muscle groups. The extrinsic muscles include the genioglossus, the hyoglossus, and the styloglossus. These muscles assist in positioning the tongue forward, backward, upward, and downward. The intrinsic muscles of the tongue—the transverse, vertical, and longitudinal muscles—are responsible for changing the tongue’s shape and are integral to both speech and swallowing. Sensation is supplied to the anterior two thirds of the tongue via the lingual nerve, which is a branch of the mandibular division of the trigeminal nerve. The posterior one third of the tongue is innervated by the glossopharyngeal nerve. Special taste afferents from the anterior tongue course through the lingual nerve to the chorda tympani nerve within the middle ear. The hypoglossal nerve controls the tongue’s motor function. Injury to this nerve will result in a tongue that deviates to the injured side on protrusion.
Palate, Velopharyngeal Sphincter, and Pharynx The palate comprises the roof of the mouth. The bony hard palate is in continuity with the soft palate posteriorly. The hard palate consists of three fused bones. The soft palate consists of muscles that originate from the posterior edge of the hard palate and the skull base. Sensory innervation to the palate is supplied by branches of the maxillary division of the trigeminal nerve, whereas motor innervation is supplied through the pharyngeal plexus of the vagus nerve. Only the tensor veli palatini muscle receives innervation from the motor division of the trigeminal nerve. The six muscles of the soft palate (levator veli palatini, tensor veli palatini, musculus uvulae, palatoglossus, palatopharyngeus, and superior pharyngeal constrictor) act to create a dynamic sling. The coordinated movement of these muscles closes the velopharyngeal sphincter, which separates the nasopharynx from the oropharynx during swallowing and speech.
In addition to assisting palate elevation, the tensor veli palatini is the primary muscle responsible for opening the eustachian tube. Abnormalities in the orientation of this muscle or its insertion in the eustachian tube cartilage, such as seen in cleft palate, greatly predispose individuals to chronic ear disease. The pharynx is a mucosal-lined tube that extends from the skull base to the esophageal inlet. It is divided into three parts—the nasopharynx, the oropharynx, and the hypopharynx. The nasopharynx is located superiorly and extends from the posterior choanae of the nasal cavity anteriorly to the level of the free edge of the soft palate inferiorly. It contains the eustachian tube and the adenoid. The oropharynx extends from the free margin of the soft palate to the vallecula. The vallecula is the space created by the junction of the tongue base with the epiglottis. The faucial tonsils lie within the oral cavity. Anteriorly, the oropharynx extends to the anterior tonsillar pillars. The hypopharynx extends from the vallecula to the esophageal inlet. The larynx and pyriform sinuses are contained within the hypopharynx.
The pharyngeal constrictors are paired muscles lining the pharynx. They insert into the medial raphe on the midline of the posterior pharyngeal wall. The superior, middle, and inferior pharyngeal constrictors are responsible for the forces generated to clear materials from the pharynx during the act of swallowing. The innervation of all the pharyngeal muscles is from the pharyngeal plexus of the vagus nerve, except the stylopharyngeus muscle, which is innervated by the glossopharyngeal nerve. Sensory innervation to the pharynx is via the glossopharyngeal nerve and pharyngeal plexus inferiorly and the maxillary division of the trigeminal nerve superiorly.
Salivary Glands The parotid duct (Stensen duct) enters the oral cavity through the buccal mucosa, which is adjacent to the second maxillary molar at the level of the gingival mucosa. The sublingual glands and the duct from the submandibular gland (Wharton duct) enter the floor of the mouth on either side of the lingual frenulum. The paired parotid glands produce the majority of the serous secretions in the mouth. The submandibular and sublingual glands predominately produce mucoid secretions in response to gustatory stimuli. Secretions in the mouth that are formed during times other than eating are expressed by minor salivary glands scattered throughout the mucosa lining the oral cavity and the pharynx.
Tonsils and Adenoids The tonsils lie within the oropharynx. The palatine or faucial tonsils are paired collections of lymphoid tissue. The tonsils are bounded anteriorly by the palatoglossus muscle (anterior tonsillar pillar) and the palatopharyngeus muscle (posterior tonsillar pillar). The superior pharyngeal constrictor muscle is deep to the tonsil. The pharyngeal tonsil—or adenoid—resides in the nasopharynx. The lingual tonsil resides in the base of the tongue. Superficial bands of lymphoid tissue connect these four masses of tonsil tissue. Waldeyer’s ring refers to this encircling mass of lymphoid (tonsillar) tissue. Its function is to process antigens and present them to the germinal centers of the lymphoid follicles. This modulates both Band T-cell populations within the tonsil in early childhood. As people age, the tonsil and adenoid tissue atrophies.
 EVALUATION OF THE ORAL CAVITY AND PHARYNX
EVALUATION OF THE ORAL CAVITY AND PHARYNX
Physical Examination
The oral examination begins anteriorly with a systematic evaluation of structures from anterior to posterior and from left to right. The floor of the mouth is examined by having the patient elevate the tongue. In small children, the tongue will often need to be elevated mechanically. The tonsils should be evaluated for signs of inflammatory changes and for debris collecting within the crypts of the tonsil. Tonsillar size should be graded on a scale of 1 to 4 (Fig. 371-1). The oropharyngeal inlet should also be evaluated for adequacy. The tonsils may be of relatively small size but when combined with a small oropharyngeal inlet, may be obstructing. The posterior pharyngeal wall should be checked for symmetry. Granular tissue may often be seen on the posterior pharyngeal wall and may represent small areas of lymphoid tissue.
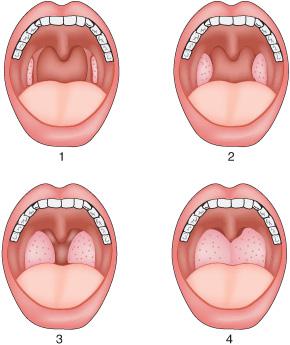
Figure 371-1. Grading of tonsillar size. (1) Tonsils are contained within the tonsillar fossa; (2) tonsils extend to the medial extend of the tonsillar pillars; (3) tonsils extend beyond the tonsillar pillars; (4) tonsils touch in the midline.
The soft palate should be evaluated both at rest and in motion. The uvula deserves close attention. A bifid uvula may be a sign of a submucosal cleft of the palate. On phonation, the soft palate should elevate and its motion should be symmetric. Intraoral palpation may also be warranted (a gloved index finger). The floor of the mouth can be palpated to check for signs of a mass or stone development within salivary ducts. The hard palate can be palpated, paying attention to the feel of its posterior aspect. A posterior projection should be apparent, signifying normal anatomy. Notching of the posterior aspect of the hard palate is found in submucous cleft palate. The buccal area can also be palpated, feeling for stones and expressing saliva from the parotid glands. The tongue can be palpated to feel for abnormalities within the substance of the tongue.
Flexible fiberoptic endoscopy of the pharynx and upper airway is an extremely useful procedure. It can be easily and safely performed in an otolaryngologist’s office in children of all ages without sedation, using only a topical anesthetic. The endoscopy checks the following: the nasopharynx for nasopharyngeal obstruction due to adenoid hypertrophy or other mass lesion and adequacy of velopharyngeal closure; the soft palate for the presence of a submucosal cleft; the tongue base, palatine, and lingual tonsils for size and inflammatory changes; and the hypopharynx and larynx for signs of obstruction from cysts, masses, or inflammation.
Radiological evaluation may be done when endoscopic examination is not available or to supplement its findings. It can begin with a lateral neck x-ray, which provides good visualization of the nasopharynx and assesses the overall size of the adenoid pad. Retropharyngeal and inflammatory processes on the posterior pharyngeal wall may also be identified. Computed tomography with contrast is now the generally accepted method for evaluating suspected inflammatory or neoplastic lesions of the pharynx. This may be supplemented by magnetic resonance imaging to provide fine detail of specific abnormalities in the oral cavity and oropharynx and the relationship to surrounding structures.
APPROACH TO THE CHILD WITH EXCESSIVE SIALORRHEA
Excessive sialorrhea, or drooling, is an uncommon problem in children who do not have developmental delay. Although some children will demonstrate significant sialorrhea early in life, this almost always self-corrects as the child reaches the fourth year of life. However, for the occasional child in whom this does not resolve or in children who have neurodevelopmental delays, a thorough workup should be done. This is best accomplished by a multidisciplinary team that includes an otolaryngologist; a dentist; and a pediatric specialist who has particular interest in childhood development, special needs children, rehabilitation, and neurological development. The otolaryngologist and dental team should perform a complete head and neck exam to ensure there are no anatomic causes for the excessive sialorrhea or other associated abnormalities in the oral cavity and pharynx, such as sensory defects or swallowing dysfunction. In children without previously diagnosed developmental delays, a full workup to rule out any undiagnosed condition should be considered. In children without a defined anatomical, motor, sensory, or neurological difficulty, assistance from a feeding team or swallowing therapist is likely all that will be required to assist with resolving the problem.
In children with neurodevelopmental delays, more aggressive therapy may also be required. This includes pharmacological therapy such as anticholinergic medications and procedural intervention, including botulinum toxin injection, which generally provides transient reduction in salivary production but is relatively noninvasive; salivary duct ligation; and salivary gland excision. The latter two procedures are more permanent but are more invasive. Utilizing these measures, sometimes in conjunction with each other, generally provides relief from excessive sialorrhea even in children with minimal ability to swallow their own secretions.
CONGENITAL MALFORMATIONS
 CLEFT LIP AND PALATE
CLEFT LIP AND PALATE
Orofacial clefting is the second most common birth defect, occurring in 1 out of every 750 live births. A cleft lip results from incomplete fusion of embryonic structures surrounding the primitive oral cavity. The clefts may be unilateral or bilateral. They are often associated with clefts of the palate. Clefts of the palate vary greatly in their extent; they may involve only the soft palate or may extend into the hard palate. The cleft may extend through the hard palate and the alveolar ridge and may be in continuity with a cleft of the lip. A combination of cleft lip and palate leads to significant cosmetic deformities of the nose. The structural support of the nose is absent, leading to abnormal lower lateral cartilage development and abnormal nasal septum development. Dental abnormalities are also common. For further discussion of managing cleft palate, see Chapter 177.
A submucous cleft palate may not be recognized until the child is several years of age. The muscular development of the soft palate is similar to that seen in a child with a cleft palate. The levator muscles do not attach in the midline of the soft palate but insert in the posterior edge of the hard palate. Mucosa completely covers the underlying defect so that there is no obvious defect of the soft palate. However, palpation of the posterior edge of the hard palate will frequently demonstrate a notch. Close inspection of the uvula will often reveal a bifid uvular structure. A blue line (zona pellucida) may be seen in the midline of the soft palate because of the lack of musculature in that area. Velopharyngeal insufficiency with hypernasal speech and an increased incidence of otitis media often result from this deformity, which can be surgically repaired if symptoms are significant.
 OTHER CONGENITAL ABNORMALITIES
OTHER CONGENITAL ABNORMALITIES
Variations of the dentition and oropharyngeal mucosal lining are discussed in Chapter 378.
Lingual Ankyloglossia
This abnormality is a common disorder and is also known as tongue-tie; with this condition, the lingual frenulum limits the movement of the anterior tongue tip. On protrusion of the tongue, there is frequently a heart-shaped deformity that is created as a very short lingual frenulum tethers the midline of the tongue. The tongue often has difficulty protruding beyond the alveolar ridge. Infants may have trouble attaching to the breast during breast-feeding or to the nipple of a bottle. In some cases, frenuloplasty can aid in tongue protrusion and can facilitate feeding. Speech difficulties secondary to ankyloglossia are uncommon. In the English language, the tongue needs only to touch the upper teeth. There are some social activities that may lead a patient to get a frenuloplasty, such as the inability to lick an ice-cream cone. If the individual is unable to protrude the tongue, this activity can be awkward.
Lingual Thyroid
Failure of the thyroid tissue to descend into the neck from its site of origin in the tongue base results in a raised, violaceous mass at the base of the tongue. In general, this thyroid tissue does not function normally. The size of the mass tends to increase over time. Frequently, signs of airway obstruction will lead the patient to a physician for evaluation. Thyroid hormone replacement will generally reduce the size of the abnormal thyroid remnant. Patients often need long-term thyroid hormone replacement therapy. This is a very rare condition and occurs more commonly in girls.
Thyroglossal Duct Cysts
In rare instances, when the thyroid gland descends into the neck from the tongue, a tract can remain that develops into a midline cystic mass in the neck. Further discussion of presentation and treatment is discussed in Chapter 372.
INFLAMMATORY DISORDERS OF THE TONSILS AND PHARYNX
 TONSILLITIS AND PHARYNGITIS
TONSILLITIS AND PHARYNGITIS
Pharyngitis presents with symptoms of sore throat, pain on swallowing, mild fever, and malaise. The pharynx and tonsils are usually erythematous on examination, and an exudate may be present over enlarged tonsils. Many, slightly enlarged cervical lymph nodes (shotty adenopathy) are often present. Common bacterial pathogens causing tonsillitis and pharyngitis are β-hemolytic Streptococcus, Streptococcus pneumoniae, Hemophilus influenzae, Peptostreptococcus, and Diphtheroids. The symptoms of bacterial pharyngitis are identical to infections caused by viruses. There are no reliable clinical findings that permit the differentiation of viral from bacterial pharyngitis. Throat cultures are necessary to direct treatment (see Chapter 285). Infectious mononucleosis must always be considered in cases of exudative tonsillitis with marked lymph node involvement in the posterior cervical chain. The diagnosis of mononucleosis is made by serology. The tonsils can enlarge enough to obstruct the airway.
Most episodes of pharyngitis and/or tonsillitis resolve without complications. In cases of recurrent acute tonsillitis, or chronic tonsillitis trials of antistaphylococcal antibiotic or rifampin may be helpful in eradicating Staphylococcus aureus or β-hemolytic Streptococcus carriage. When there are multiple episodes of acute tonsillitis, or in chronic tonsillitis unresponsive to medical therapy, adenotonsillectomy may be indicated.
 PERITONSILLAR ABSCESS
PERITONSILLAR ABSCESS
Infections of the tonsils invade the substance of the tonsillar tissue. Spread of the infection to the surrounding tissue results in a peritonsillar cellulitis that may require intravenous antibiotics to resolve the infection. At times, the cellulitis progresses and a coalescence of the infection leads to development of a peritonsillar abscess. The abscess collection and surrounding soft tissue edema cause medial displacement of the tonsil and asymmetry of the posterior soft palate, with the uvula deviating away from the site of infection and with a downward bulge of the soft palate. Trismus and ipsilateral otalgia may be associated with a peritonsillar abscess. A characteristic muffled (hot potato) voice is heard. Treatment of a peritonsillar abscess generally requires drainage of the abscess. This may be accomplished by needle aspiration, by incision and drainage, or by tonsillectomy. A delayed tonsillectomy is generally recommended in patients with a peritonsillar cellulitis/abscess if there is a preceding history of recurring throat or tonsil infections. Mononucleosis can be associated with coincident peritonsillar abscess.
 RETROPHARYNGEAL ABCESS
RETROPHARYNGEAL ABCESS
Lymph nodes in the retropharynx and parapharyngeal space enlarge in response to infection. At times, the node becomes overwhelmed with the infection and becomes necrotic. Cellulitis may progress to abscess. Surgical drainage of the abscess in the retropharyngeal or parapharyngeal space is generally required. Cellulitis will typically respond to high doses of intravenous antibiotics. Peritonsillar abscess, parapharyngeal space abscess, and retropharyngeal abscess all have the potential to cause life-threatening complications if diagnosis and treatment are delayed. A mass effect can cause airway obstruction. Infection may also spread along natural tissue planes upward to the skull base (causing meningitis) or inferiorly into the mediastinum. In cases in which surgical drainage is required, intubation must be performed carefully because the act of intubation can rupture the abscess cavity, soiling an unprotected airway with purulent material.
ADENOTONSILLAR HYPERTROPHY WITH AIRWAY OBSTRUCTION
Adenotonsillar hypertrophy can cause obstruction of the upper airway. Children often present with chronic snoring, interruption of airflow during inspiration, restless sleep behavior, and daytime somnolence. The work of breathing increases as airway obstruction increases. Respiratory rate irregularity also increases as the work of breathing increases. This pattern of sleep disturbance can vary during the night with sleep stages and is often worse during rapid eye movement (REM) sleep. The evaluation and causes of sleep disordered breathing are also discussed in Chapter 509. Snoring is the hallmark of upper airway obstruction and may be caused by enlarged adenoid tissue or tonsils or both. When a questionable history of nighttime breathing patterns is obtained, it is often useful to have the parents record sound alone or videotape the child while sleeping to more adequately allow the physician to evaluate reports of noisy breathing, apneic episodes, and irregular breathing patterns.
Obesity is not always a common feature of children with obstructive apnea. Many children present with poor weight gain because of poor eating habits. Sleep apnea in children is associated with daytime behavioral habits that range from agitation to somnolence. In severely affected children, pulmonary hypertension and cor pulmonale may develop, but these are uncommon. If large tonsils are evident on physical examination, adenotonsillectomy is usually curative. If the tonsils are small on examination, a lateral neck radiograph may demonstrate adenoid hypertrophy or the adenoids can be visualized by nasopharyngoscopy.
Tonsillectomy and Adenoidectomy
The indications for tonsillectomy and adenoidectomy and for adenoidectomy alone are listed in Table 371-1. Rare disorders that appear to improve following tonsillectomy include an immunoglobulin A nephropathy that is associated with recurrent tonsillitis1, and periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis syndrome (PFAPA). Surgery is best performed when the acute inflammatory response has subsided, generally 6 weeks after the last infection. In some circumstances, however, a tonsillectomy is necessary during an acute infection if there are life-threatening complications such as airway compromise or development of a peritonsillar abscess. Tonsil-lectomy usually consists of a subcapsular dissection and total removal of the tonsils. When tonsillectomy is performed for sleep-disordered breathing, a partial or intracapsular tonsillectomy is an option for treatment of tonsillar hypertrophy that may be as effective and appears to reduce postoperative pain and decrease recovery time. The most common complication of tonsillectomy is bleeding, occurring in about 3% of children. It most often occurs within 24 hours of surgery but late bleeding occurs up to 10 days following surgery. Other early complications include pain, dehydration and weight loss due to poor oral intake, and occasional difficulty breathing due to swelling around the surgical sites.
Table 371-1. Indications for Tonsillectomy and Adenoidectomy and for Adenoidectomy Alone
Indications for Tonsillectomy and Adenoidectomy |
Infectious Disease |
Recurrent, acute tonsillitis, with more than 6–7 episodes in 1 year, 5 episodes per year for 2 years, or 3 episodes per year for 3 years |
Recurrent, acute tonsillitis, with recurrent febrile seizures, or cardiac valvular disease |
Chronic tonsillitis, unresponsive to medical therapy or local measures |
Peritonsillar abscess with history of tonsillar infections |
Obstructive Disease |
Heroic snoring with chronic mouth breathing |
Obstructive sleep apnea or sleep disturbances |
Adenotonsillar hypertrophy with dysphagia or speech abnormalities |
Adenotonsillar hypertrophy with craniofacial growth or occlusive abnormalities |
Mononucleosis with obstructive tonsillar hypertrophy, unresponsive to steroids |
Other |
Asymmetric growth or tonsillar lesion suspicious for neoplasm (without adenoidectomy) |
Indications for Adenoidectomy Alone |
Infectious Disease |
Adenoid hypertrophy with eustachian tube dysfunction and persistent ear infection or middle ear effusion |
Adenoid hypertrophy associated with chronic sinusitis, unresponsive to medical therapy |
Obstructive adenoid hypertrophy |
Heroic snoring with chronic mouth breathing |
Obstructive sleep apnea or sleep disturbances |
Craniofacial growth or occlusive abnormalities |
Other |
Adenoid mass or lesion or asymmetric enlargement |



