Perimenopause includes the time beginning with the first features of the approaching menopause, such as vasomotor symptoms and menstrual irregularity, and ends 12 months after the last menstrual period.
Post-menopause should be defined as dating from the final menstrual period. However, it cannot be determined until after 12 months of spontaneous amenorrhoea.
Premature menopause is arbitrarily defined as menopause occurring before the age of 40 and affects 1% of women. In most women no cause is found. Some will have a surgical menopause following bilateral oöphorectomy perhaps performed during hysterectomy. Other causes include infections, autoimmune disorders, chemotherapy, ovarian dysgenesis and metabolic diseases. Hormone replacement therapy (HRT) is indicated at least until the age of 50. Oocyte donation is required for fertility treatment.
Post-menopausal Bleeding
Definition
Vaginal bleeding occurring at least 12 months after the last menstrual period.
Causes
Post-menopausal bleeding is an important clinical problem. The main onus is to exclude carcinoma of the endometrium or cervix and premalignant endometrial hyperplasia with cytological atypia, which account for about 20% of cases. Withdrawal bleeds occur with sequential HRT and, so long as they are regular, do not warrant investigation. Bleeding may also occur from a poorly oestrogenized vaginal wall: ‘atrophic vaginitis’, but this should be a diagnosis of exclusion. A purulent blood-stained vaginal discharge in a post-menopausal woman should be investigated to rule out endometrial cancer or, uncommonly, a diverticular abscess draining via the uterus or vagina.
Causes of Post-menopausal Bleeding (PMB)
Endometrial carcinoma
Endometrial hyperplasia ± atypia and polyps
Cervical carcinoma
Atrophic vaginitis
Cervicitis
Ovarian carcinoma
Cervical polyps
Management
All women should undergo a bimanual and speculum examination and a cervical smear taken if one has not been taken according to the national screening programme. Transvaginal sonography (TVS) has become a routine procedure for initial assessment. It measures endometrial thickness and also gives information on other pelvic pathology, such as fibroids and ovarian cysts. TVS is less invasive than endometrial biopsy or hysteroscopy but does not give a histological diagnosis. A thickened endometrium or a cavity filled with fluid indicates an increased risk of malignancy or other pathology (hyperplasia or polyps).
If the endometrial thickness is 4 mm or less on TVS and there was only a single episode of PMB then endometrial biopsy ± hysteroscopy is not required. If the endometrium is thicker or there have been multiple bleeds an endometrial biopsy ± hysteroscopy should be performed. If undertaken as an outpatient procedure, endometrium can be obtained using a Pipelle suction device. Outpatient hysteroscopy, under paracervical local anaesthetic block, can also be performed. If an endometrial polyp is found on scan, if the woman is anxious about having a procedure under local, or if vaginal access is expected to be difficult (for instance due to an atrophic vagina) then hysteroscopy and endometrial biopsy is performed under general anaesthetic as a day case procedure. Once malignancy is excluded, atrophic vaginitis can be treated with topical oestrogen.
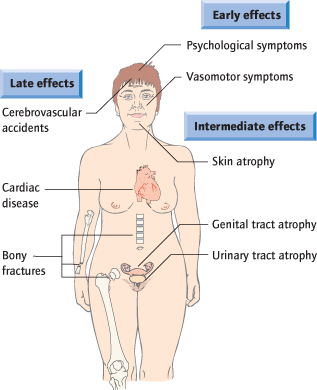
Symptoms and Consequences of the Menopause (Fig. 13.2)
Cardiovascular Disease
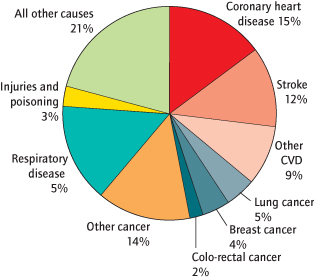
CVD (coronary heart disease and stroke) is the number one cause of death globally. In the UK, CVD accounts for about one-third of all deaths in women (Fig. 13.3): the same proportion as for men.
Fig. 13.3 Deaths by cause, women, UK
(redrawn from the British Heart Foundation).
CVD, cardiovascular disease.
Vasomotor Symptoms
Hot flushes and night sweats are the most common symptoms of the menopause and affect about 70% of Western women. Night sweats can cause sleep disturbance leading to tiredness and irritability. They may begin before periods stop and usually are present for less than 5 years. However, some women will continue to flush in their 60s and 70s.
Urogenital Problems
Oestrogen deficiency can cause vaginal atrophy and urinary problems. Vaginal atrophy can also affect women taking systemic HRT. It can be extremely uncomfortable and can result in dyspareunia, cessation of sexual activity, itching, burning and dryness. Urinary symptoms include frequency, urgency, nocturia, incontinence and recurrent infection. Women may suffer in silence and not seek medical help.
Sexual Problems
Sexual problems affect about half of all women and become more common with age. Interest in sex declines in both sexes with increasing age and this change is more pronounced in women. The term female sexual dysfunction (FSD) is now used and an international classification system employed. Sexual problems are classified into various types: loss of sexual desire, loss of sexual arousal, problems with orgasm and sexual pain, e.g. dyspareunia.
Osteoporosis
Osteoporosis is ‘a skeletal disorder characterized by compromised bone strength predisposing to an increased risk of fracture’. It is a major problem with 1 in 3 women over 50 years (and 1 in 12 men) having one or more osteoporotic fractures. Bone strength reflects the integration of two main features: bone density and bone quality. Bone density is expressed as grams of mineral per area or volume and, in any given individual, is determined by peak bone mass and amount of bone loss. Bone quality refers to architecture, turnover, damage accumulation (e.g. microfractures) and mineralization.
The World Health Organization (WHO) definitions of osteoporosis, classified according to bone mineral density (BMD), are shown below. The T score is that number of standard deviations (SD) by which a particular bone differs from the young normal mean.
Definitions of Osteoporosis According to the World Health Organization (WHO)
| Description | Definition |
| Normal: | BMD value between −1 SD and +1 SD of the young adult mean (T score −1 to +1) |
| Osteopenia: | BMD between −1 and −2.5 SD from the young adult mean (T score −1 to −2.5) |
| Osteoporosis: | BMD ≥ −2.5 SD from the young adult mean (T score −2.5 or lower) |
Osteoporotic Fractures
Fractures are the clinical consequences of osteoporosis. The most common sites are the wrist or Colles’ fracture, the hip and the spine. Fractures have a major impact on quality of life, result in a significant economic burden and, in the case of hip fractures, are associated with considerable mortality (30% in the year after a hip fracture).
Risk Factors for the Development of Osteoporosis
Most important in clinical practice are parental history of fracture (particularly hip fracture), early menopause, chronic use of corticosteroids (oral and possibly inhaled), prolonged immobilization and prior fracture.
Risk Factors for Osteoporosis
| Genetic: | Family history of fracture (particularly a first-degree relative with hip fracture) |
| Constitutional: | Low body mass index |
| Early menopause (<45 years of age) | |
| Environmental: | Cigarette smoking |
| Alcohol abuse | |
| Low calcium intake | |
| Sedentary life style | |
| Drugs: | Corticosteroids, >5 mg/day prednisolone or equivalent |
| Diseases: | Rheumatoid arthritis |
| Neuromuscular disease | |
| Chronic liver disease | |
| Malabsorption syndromes | |
| Hyperparathyroidism | |
| Hyperthyroidism | |
| Hypogonadism |
Investigations of the Menopause
Follicle-Stimulating Hormone (FSH)
FSH levels give an estimate of the degree of ovarian reserve remaining (Fig. 13.4). Increased levels suggest fewer oocytes remaining in the ovaries. Levels are helpful with suspected premature ovarian failure
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree