Chapter 1
The History of Obstetric Anesthesia
Donald Caton MD
For I heard a cry as of a woman in travail, anguish as of one bringing forth her first child, the cry of the daughter of Zion gasping for breath, stretching out her hands, “Woe is me!”
—JEREMIAH 4:31
Chapter Outline
MEDICAL OBJECTIONS TO THE USE OF ETHER FOR CHILDBIRTH
PUBLIC REACTION TO ETHERIZATION FOR CHILDBIRTH
THE EFFECTS OF ANESTHESIA ON THE NEWBORN
THE EFFECTS OF ANESTHESIA ON LABOR
“The position of woman in any civilization is an index of the advancement of that civilization; the position of woman is gauged best by the care given her at the birth of her child.” So wrote Haggard1 in 1929. If his thesis is true, Western civilization made a giant leap on January 19, 1847, when James Young Simpson used diethyl ether to anesthetize a woman with a deformed pelvis for delivery. This first use of a modern anesthetic for childbirth occurred a scant 3 months after Morton’s historic demonstration of the anesthetic properties of ether at the Massachusetts General Hospital in Boston. Strangely enough, Simpson’s innovation evoked strong criticism from contemporary obstetricians, who questioned its safety, and from many segments of the lay public, who questioned its wisdom. The debate over these issues lasted more than 5 years and influenced the future of obstetric anesthesia.2
James Young Simpson
Few people were better equipped than Simpson to deal with controversy. Just 36 years old, Simpson already had 7 years’ tenure as Professor of Midwifery at the University of Edinburgh, one of the most prestigious medical schools of its day (Figure 1-1). By that time, he had established a reputation as one of the foremost obstetricians in Great Britain, if not the world. On the day he first used ether for childbirth, he also received a letter of appointment as Queen’s Physician in Scotland. Etherization for childbirth was only one of Simpson’s contributions. He also designed obstetric forceps (which still bear his name), discovered the anesthetic properties of chloroform, made important innovations in hospital architecture, and wrote a textbook on the practice of witchcraft in Scotland that was used by several generations of anthropologists.3
FIGURE 1-1 James Young Simpson, the obstetrician who first administered a modern anesthetic for childbirth. He also discovered the anesthetic properties of chloroform. Many believe that he was the most prominent and influential physician of his day. (Courtesy Yale Medical History Library.)
An imposing man, Simpson had a large head, a massive mane of hair, and the pudgy body of an adolescent. Contemporaries described his voice as “commanding,” with a wide range of volume and intonation. Clearly Simpson had “presence” and “charisma.” These attributes were indispensable to someone in his profession, because in the mid-nineteenth century, the role of science in the development of medical theory and practice was minimal; rhetoric resolved more issues than facts. The medical climate in Edinburgh was particularly contentious and vituperative. In this milieu, Simpson had trained, competed for advancement and recognition, and succeeded. The rigor of this preparation served him well. Initially, virtually every prominent obstetrician, including Montgomery of Dublin, Ramsbotham of London, Dubois of Paris, and Meigs of Philadelphia, opposed etherization for childbirth. Simpson called on all of his professional and personal finesse to sway opinion in the ensuing controversy.
Medical Objections to the Use of Ether for Childbirth
Shortly after Simpson administered the first obstetric anesthetic, he wrote, “It will be necessary to ascertain anesthesia’s precise effect, both upon the action of the uterus and on the assistant abdominal muscles; its influence, if any, upon the child; whether it has a tendency to hemorrhage or other complications.”4 With this statement he identified the issues that would most concern obstetricians who succeeded him and thus shaped the subsequent development of the specialty.
Simpson’s most articulate, persistent, and persuasive critic was Charles D. Meigs, Professor of Midwifery at Jefferson Medical College in Philadelphia (Figure 1-2). In character and stature, Meigs equaled Simpson. Born to a prominent New England family, Meigs’ forebears included heroes of the American revolutionary war, the first governor of the state of Ohio, and the founder of the University of Georgia. His descendants included a prominent pediatrician, an obstetrician, and one son who served the Union Army as Quartermaster General during the Civil War.5
FIGURE 1-2 Charles D. Meigs, the American obstetrician who opposed the use of anesthesia for obstetrics. He questioned the safety of anesthesia and said that there was no demonstrated need for it during a normal delivery. (Courtesy Wood-Library Museum.)
At the heart of the dispute between Meigs and Simpson was a difference in their interpretation of the nature of labor and the significance of labor pain. Simpson maintained that all pain, labor pain included, is without physiologic value. He said that pain only degrades and destroys those who experience it. In contrast, Meigs argued that labor pain has purpose, that uterine pain is inseparable from contractions, and that any drug that abolishes pain will alter contractions. Meigs also believed that pregnancy and labor are normal processes that usually end quite well. He said that physicians should therefore not intervene with powerful, potentially disruptive drugs (Figure 1-3). We must accept the statements of both men as expressions of natural philosophy, because neither had facts to buttress his position. Indeed, in 1847, physicians had little information of any sort about uterine function, pain, or the relationship between them. Studies of the anatomy and physiology of pain had just begun. It was only during the preceding 20 years that investigators had recognized that specific nerves and areas of the brain have different functions and that specialized peripheral receptors for painful stimuli exist.2
In 1850, more physicians expressed support for Meigs’s views than for Simpson’s. For example, Baron Paul Dubois6 of the Faculty of Paris wondered whether ether, “after having exerted a stupefying action over the cerebro-spinal nerves, could not induce paralysis of the muscular element of the uterus?” Similarly, Ramsbotham7 of London Hospital said that he believed the “treatment of rendering a patient in labor completely insensible through the agency of anesthetic remedies … is fraught with extreme danger.” These physicians’ fears gained credence from the report by a special committee of the Royal Medical and Chirurgical Society documenting 123 deaths that “could be positively assigned to the inhalation of chloroform.”8 Although none involved obstetric patients, safety was on the minds of obstetricians.
The reaction to the delivery of Queen Victoria’s eighth child in 1853 illustrated the aversion of the medical community to obstetric anesthesia. According to private records, John Snow anesthetized the Queen for the delivery of Prince Leopold at the request of her personal physicians. Although no one made a formal announcement of this fact, rumors surfaced and provoked strong public criticism. Thomas Wakley, the irascible founding editor of The Lancet, was particularly incensed. He “could not imagine that anyone had incurred the awful responsibility of advising the administration of chloroform to her Majesty during a perfectly natural labour with a seventh child.”9 (It was her eighth child, but Wakley had apparently lost count—a forgivable error considering the propensity of the Queen to bear children.) Court physicians did not defend their decision to use ether. Perhaps not wanting a public confrontation, they simply denied that the Queen had received an anesthetic. In fact, they first acknowledged a royal anesthetic 4 years later when the Queen delivered her ninth and last child, Princess Beatrice. By that time, however, the issue was no longer controversial.9
Public Reaction to Etherization for Childbirth
The controversy surrounding obstetric anesthesia was not resolved by the medical community. Physicians remained skeptical, but public opinion changed. Women lost their reservations, decided they wanted anesthesia, and virtually forced physicians to offer it to them. The change in the public’s attitude in favor of obstetric anesthesia marked the culmination of a more general change in social attitudes that had been developing over several centuries.
Before the nineteenth century, pain meant something quite different from what it does today. Since antiquity, people had believed that all manner of calamities—disease, drought, poverty, and pain—signified divine retribution inflicted as punishment for sin. According to Scripture, childbirth pain originated when God punished Eve and her descendants for Eve’s disobedience in the Garden of Eden. Many believed that it was wrong to avoid the pain of divine punishment. This belief was sufficiently prevalent and strong to retard acceptance of even the idea of anesthesia, especially for obstetric patients. Only when this tradition weakened did people seek ways to free themselves from disease and pain. In most Western countries, the transition occurred during the nineteenth century. Disease and pain lost their theologic connotations for many people and became biologic processes subject to study and control by new methods of science and technology. This evolution of thought facilitated the development of modern medicine and stimulated public acceptance of obstetric anesthesia.10
The reluctance that physicians felt about the administration of anesthesia for childbirth pain stands in stark contrast to the enthusiasm expressed by early obstetric patients. In 1847, Fanny Longfellow, wife of the American poet Henry Wadsworth Longfellow and the first woman in the United States anesthetized for childbirth, wrote:
I am very sorry you all thought me so rash and naughty in trying the ether. Henry’s faith gave me courage, and I had heard such a thing had succeeded abroad, where the surgeons extend this great blessing more boldly and universally than our timid doctors. … This is certainly the greatest blessing of this age.11
Queen Victoria, responding to news of the birth of her first grandchild in 1860 and perhaps remembering her own recent confinement, wrote, “What a blessing she [Victoria, her oldest daughter] had chloroform. Perhaps without it her strength would have suffered very much.”9 The new understanding of pain as a controllable biologic process left no room for Meigs’s idea that pain might have physiologic value. The eminent nineteenth-century social philosopher John Stuart Mill stated that the “hurtful agencies of nature” promote good only by “inciting rational creatures to rise up and struggle against them.”12
Simpson prophesied the role of public opinion in the acceptance of obstetric anesthesia, a fact not lost on his adversaries. Early in the controversy he predicted, “Medical men may oppose for a time the superinduction of anaesthesia in parturition but they will oppose it in vain; for certainly our patients themselves will force use of it upon the profession. The whole question is, even now, one merely of time.”13 By 1860, Simpson’s prophecy came true; anesthesia for childbirth became part of medical practice by public acclaim, in large part in response to the demands of women.
Opioids and Obstetrics
The next major innovation in obstetric anesthesia came approximately 50 years later. Dämmerschlaff, which means “twilight sleep,” was a technique developed by von Steinbüchel14 of Graz and popularized by Gauss15 of Freiberg. It combined opioids with scopolamine to make women amnestic and somewhat comfortable during labor (Figure 1-4). Until that time, opioids had been used sparingly for obstetrics. Although opium had been part of the medical armamentarium since the Roman Empire, it was not used extensively, in part because of the difficulty of obtaining consistent results with the crude extracts available at that time. Therapeutics made a substantial advance in 1809 when Sertürner, a German pharmacologist, isolated codeine and morphine from a crude extract of the poppy seed. Methods for administering the drugs remained unsophisticated. Physicians gave morphine orally or by a method resembling vaccination, in which they placed a drop of solution on the skin and then made multiple small puncture holes with a sharp instrument to facilitate absorption. In 1853, the year Queen Victoria delivered her eighth child, the syringe and hollow metal needle were developed. This technical advance simplified the administration of opioids and facilitated the development of twilight sleep approximately 50 years later.16
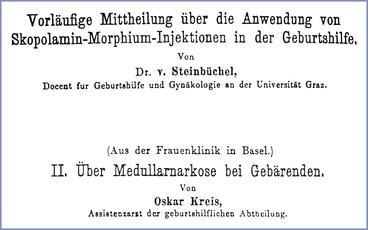
FIGURE 1-4 Title pages from two important papers published in the first years of the twentieth century. The paper by von Steinbüchel introduced twilight sleep. The paper by Kreis described the first use of spinal anesthesia for obstetrics.
Although reports of labor pain relief with hypodermic morphine appeared as early as 1868, few physicians favored its use. For example, in an article published in Transactions of the Obstetrical Society of London, Sansom17 listed the following four agents for relief of labor pain: (1) carbon tetrachloride, the use of which he favored; (2) bichloride of methylene, which was under evaluation; (3) nitrous oxide, which had been introduced recently by Klikgowich of Russia; and (4) chloroform. He did not mention opioids, but neither did he mention diethyl ether, which many physicians still favored. Similarly, Gusserow,18 a prominent German obstetrician, described using salicylic acid but not morphine for labor pain. (Von Baeyer did not introduce acetylsalicylic acid to medical practice until 1899.) In retrospect, von Steinbüchel’s and Gauss’s descriptions of twilight sleep in the first decade of the century may have been important more for popularizing morphine than for suggesting that scopolamine be given with morphine.
Physicians reacted to twilight sleep as they had reacted to diethyl ether several years earlier. They resisted it, questioning whether the benefits justified the risks. Patients also reacted as they had before. Not aware of, or perhaps not concerned with, the technical considerations that confronted physicians, patients harbored few doubts and persuaded physicians to use it, sometimes against the physicians’ better judgment. The confrontation between physicians and patients was particularly strident in the United States. Champions of twilight sleep lectured throughout the country and published articles in popular magazines. Public enthusiasm for the therapy subsided slightly after 1920, when a prominent advocate of the method died during childbirth. She was given twilight sleep, but her physicians said that her death was unrelated to any complication from its use. Whatever anxiety this incident may have created in the minds of patients, it did not seriously diminish their resolve. Confronted by such firm insistence, physicians acquiesced and used twilight sleep with increasing frequency.19,20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree