Chapter 25 The epidemiology of obstetrics
MATERNAL MORTALITY
A maternal death is defined by the International Classification of Diseases, Injuries and Causes of Death (ICD-10) as the death of a woman while pregnant or within 42 days after abortion, miscarriage or delivery that are due to direct or indirect maternal causes. These deaths are divided into direct, indirect, late and incidental (Box 25.1). The maternal mortality rate is the number of such deaths per 100 000 maternities.
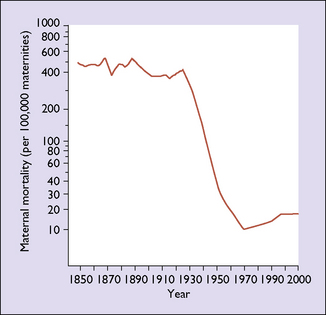
In most developed countries the maternal death rate remained about the same from 1850 to 1934, when it began to fall. In the period before the mid-1930s it was about 500 per 100 000; by the mid-1980s, in many industrialized countries it had fallen to fewer than 10 per 100 000 maternities (Fig. 25.1). The initial fall was due to the control of infections by better obstetric care and the introduction of antibiotics. The second factor was that most women availed themselves of good-quality antenatal care, which enabled complications to be detected early and treatment to be offered, usually in well-equipped hospitals staffed by trained medical attendants. Blood became increasingly and quickly available from blood banks, which considerably reduced the deaths due to haemorrhage. Sociological changes have also occurred in the past 60 years: fewer women now have more than three children, and most have their pregnancies before the age of 35. Higher parity and advancing age increase the risk of maternal death. There has been a small rise in the maternal mortality rates in some developed countries in the last decade. Whether this is due to women with medical conditions that previously precluded pregnancy having children, increasing maternal age, the rise in obesity or better ascertainment of cases is not clear.
Causes of maternal death
These reports have been published in the UK since 1952 and in Australia since 1965. The total direct and indirect deaths per 100 000 maternities had risen from 9.83 in the 1985–7 triennium to 12.45 in 2003–5. This may be due to underreporting in earlier years, but emphasizes that there is no room for complacency in modern maternity units in the developed world. The major contributing factors to suboptimal care are poor liaison between healthcare professionals, failure to appreciate the severity of the condition, and wrong diagnosis. Table 25.1 shows the most common causes of death, Table 25.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree