Background
There are a number of poor birth outcomes with advancing maternal age. Although there is some evidence of a higher risk of trauma to obstetric anal sphincter and the levator ani muscle with advancing age, findings to date are inconclusive.
Objective
The aim of this study was to assess the risk of pelvic floor injury using translabial 3- and 4-dimensional ultrasound relative to advancing maternal age in primiparous women after a singleton vaginal delivery at term and to determine any association between maternal age and obstetric trauma, including obstetric anal sphincter injuries, levator avulsion, and irreversible overdistension of the levator hiatus.
Study Design
This is a subanalysis of a perinatal intervention trial conducted in a specialist urogynecology referral unit at 2 tertiary units. All primiparous women with singleton birth at term underwent 3- and 4-dimensional translabial pelvic floor ultrasound both ante- and postnatally for the assessment of the obstetric trauma including levator ani muscle avulsion, hiatal overdistension to 25 cm 2 or more, and obstetric anal sphincter injuries. A multivariate logistic regression analysis was performed to examine the association between maternal age and obstetric trauma diagnosed on 3- and 4-dimensional translabial ultrasound. Multiple confounders were included, and the most significant (forceps and vacuum delivery) were used for probability modeling.
Results
Of 660 women recruited for the original study, a total of 375 women who had a vaginal delivery with complete data sets were analyzed. A total of 174 women (46.4%) showed evidence of at least 1 form of major pelvic floor trauma. Advancing maternal age at first delivery carries with it a significant incremental risk of major pelvic floor trauma with an odds ratio of 1.064 for overall risk of injury for each increasing year of age past age 18 years ( P = .003). The probability of any type of trauma appears to be substantially higher for forceps delivery. Vacuum delivery appears to increase the risk of obstetric anal sphincter injuries but not of levator avulsion.
Conclusion
There is a significant association between the risk of major pelvic floor injury and increasing maternal age at first delivery.
There has been a marked increase in developed countries in the age of women giving birth to their first child. Pregnancy at an advanced maternal age is associated with a higher risk of adverse outcomes such as miscarriage, preeclampsia, small for gestational age, gestational diabetes mellitus, and emergency operative deliveries.
However, there is limited information in the literature regarding any association between advancing maternal age at the time of vaginal delivery with a risk of maternal obstetric trauma. A retrospective study utilizing 3- and 4-dimensional translabial ultrasound in women with pelvic floor dysfunction showed a higher risk of levator ani muscle injuries (avulsion) in mothers who had their first child at a more advanced age. However, most mothers involved in the study were multiparous. Therefore, it is not clear which delivery might have caused the injury diagnosed many years later.
In retrospective epidemiological studies of primiparous women, older mothers appear to have a higher risk of obstetric anal sphincter injuries compared with younger mothers. Whereas there is some suggestion of a higher risk of obstetric anal sphincter injuries and levator ani muscle injuries in older mothers having their first child, to date this has not been conclusively demonstrated in a prospective study examining the effects of advanced maternal age on obstetric trauma.
This study is a subanalysis of a multicenter randomized controlled trial, the Epi-No trial, which tested an antenatal intervention for its effect on postnatally diagnosed obstetric trauma. The Epi-No trial is a birth trainer device developed to gradually stretch the vagina and perineum with the aim of reducing perineal trauma.
The aim of this subanalysis is to assess the risk of pelvic floor injury using 3- and 4-dimensional ultrasound relative to advancing maternal age in primiparous women after singleton vaginal delivery at term. We aim to define a statistical association between maternal age and sonographically diagnosed defects of the external anal sphincter, levator ani muscle avulsion, and irreversible hiatal overdistension in the context of both simple and operative vaginal deliveries.
Materials and Methods
This study is a subanalysis of a prospective perinatal interventional trial at 2 tertiary obstetric units in Australia. Women in their first ongoing pregnancy in the third trimester were recruited between July 2007 and September 2013. They all underwent a standardized interview, clinical examination including International Continence Society Pelvic Organ Prolapse Quantification assessment and a 3- and 4-dimensional translabial pelvic floor ultrasound, at 35–37 weeks of gestation and 3–6 months postpartum. The assessor at the postpartum follow-up was blinded to the intrapartum data.
Ultrasound volume acquisition was performed using either a GE Voluson 730 Expert or E8 System (GE Medical Systems, Zipf, Austria), with an 8–4-MHz curved array volume transducer, supine and after voiding, at rest, on maximum valsalva maneuver (the best of at least 3 attempts) and on maximal pelvic floor muscle contraction. At least 1 volume data set was obtained on pelvic floor muscle contraction, ensuring that the entire anal canal was included in the volume for the assessment of anal sphincter.
Ultrasound volume data sets were analyzed for levator avulsion, hiatal overdistension (microtrauma), and external anal sphincter integrity independently at a later date on a desktop personal computer using the proprietary software GE Kretz 4D View version 10.0 (GE Medical Ultrasound Kretz GmbH, Zipf, Austria) with the assessors blinded to all clinical data.
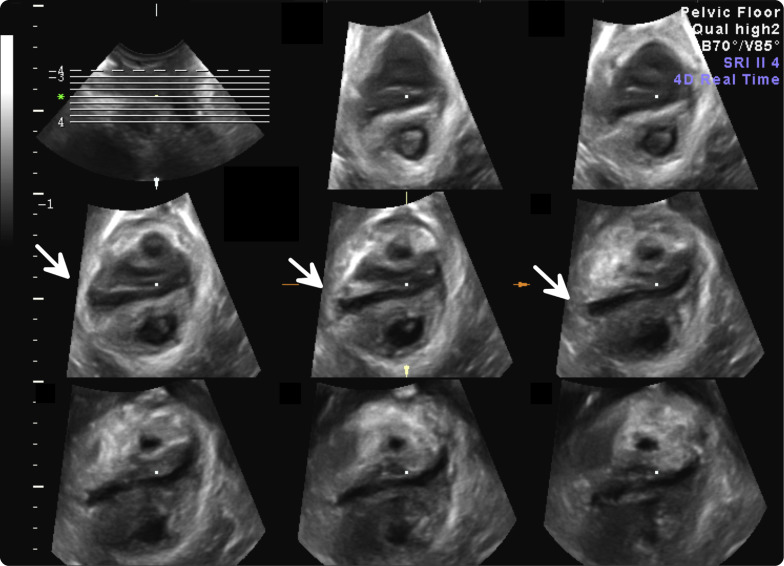
Levator avulsion was diagnosed on tomographic ultrasound imaging of the pelvic floor at 2.5 mm interslice interval incorporating slices 5 mm caudal to 12.5 mm cranial of the plane of minimal hiatal dimensions on volumes obtained at maximal pelvic floor muscle contraction. A data set was rated positive for avulsion upon observing an abnormal insertion of the puborectalis muscle on the inferior pubic ramus in the 3 central slices (reference slice and the slices 2.5–5 mm cranial (ie, slices 3–5 in Figure 1 ).
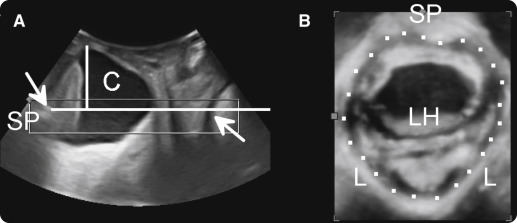
Significant hiatal overdistension (microtrauma) was defined as a peripartum increase in the hiatal area on valsalva of at least 20%, resulting in a hiatal area of ≥25 cm 2 (ballooning) in the absence of levator avulsion. The plane of minimal hiatal dimensions was identified in the midsagittal orthogonal plane, in which the distance between the hyperechogenic posterior aspect of the symphysis pubis and the hyperechogenic anterior border of the levator ani muscle, just posterior to the anorectal muscularis, is shortest. The hiatal area was measured in rendered volumes of 1–2 cm thickness containing this plane of minimal hiatal dimensions ( Figure 2 ).
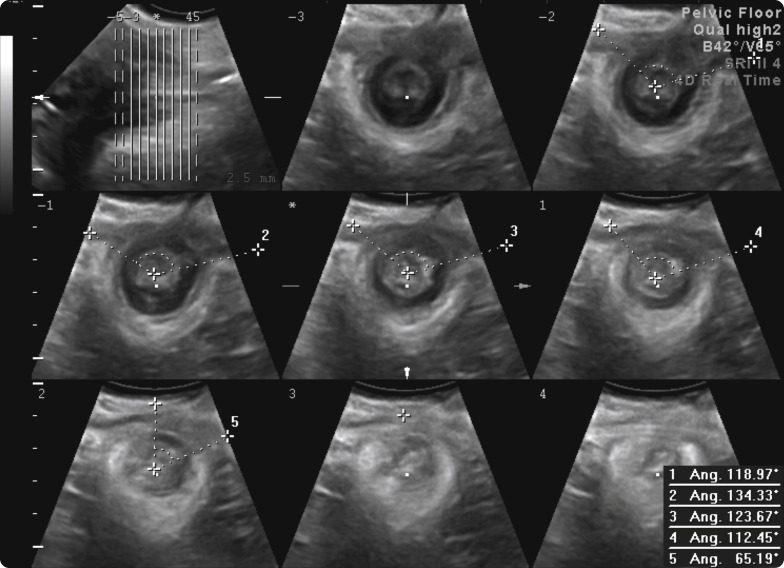
External anal sphincter integrity was assessed utilizing volumes acquired on pelvic floor muscle contraction. A set of 8 tomographic ultrasound imaging slices in an oblique coronal plane was obtained encompassing the entire external anal sphincter by tailoring the interslice interval to the individual’s external anal sphincter length, from the level of the puborectalis muscle to the subcutaneous part of the external anal sphincter ( Figure 3 ). A significant external anal sphincter defect is defined as the presence of a gap of ≥30° in its circumference, in at least 4 of 6 central slices.
The ultrasound data were analyzed against obstetric data retrieved from the local maternity database. Statistical analysis was performed using Minitab version 16 (Minitab Inc, State College, PA) and SAS version 9.3 (SAS Institute Inc, Cary, NC). A logistic regression analysis was performed to determine the association between maternal age and the risk of the 3 types of pelvic floor damage as described in the previous text and also the overall combinations of any 3 types of injury.
We adjusted for multiple confounders including gestational age at delivery, body mass index, birthweight, head circumference, and delivery mode. Confounders were selected on the basis of prior evidence and used for full multivariate modeling. A backward elimination approach was utilized, with covariates eliminated in order of lack of significance.
A value of P < .05 was considered statistically as significant. We did not undertake power calculations for this particular subanalysis. Because the intervention tested in the parent trial (antenatal use of the Epi-No device) was shown to have no effect on any of the tested outcome measures, we felt justified to perform this subanalysis not just in the control arm but also in the entire study population. The parent randomized controlled trial was approved by the Sydney West and Sydney South Area Health Service Human Research Ethics Committee (SWAHS HREC 07-022 and SSAHS HREC X09-0384).
Results
Six hundred sixty nulliparous women carrying an uncomplicated singleton pregnancy were recruited for the Epi-No trial, at a mean gestation of 35.8 weeks (SD, 0.75, range, 31.6–37.6 weeks). A total of 498 of 660 women (75.5%) returned for a follow-up appointment at a mean interval of 5 months (SD, 2.5, range, 1.8–24.3 months).
In 5 women, we were unable to retrieve ultrasound data sets or the imaging was unsatisfactory, and delivery record data were missing in 6 subjects. Of the remainder, 112 women (23%) had a cesarean delivery, leaving a total of 375 women who had a vaginal delivery for analysis.
Mean age was 30.5 years (SD, 5.1, range, 18.8–42.5) years, mean body mass index was 27.9 kg/m 2 (range, 18.0–28.6 kg/m 2 ) at the time of recruitment, and the mean gestation at delivery was 39.7 weeks (range, 36.3–42.2 weeks). Mean birth weight was 3.41 kg (range, 2.2–4.7 kg). Eighty percent of the study group was white. Of those 375 women, 269 (72%) had a normal vaginal delivery, 69 (18%) had a vacuum extraction, and 37 (10%) had a forceps delivery. Of those with a vaginal delivery, 102 (27%) had a mediolateral episiotomy. The mean length of the first stage was 455 minutes (SD, 267, range, 50–1720 minutes), and the mean second stage was 80 minutes (SD, 67, range, 0–472 minutes).
Levator avulsion was diagnosed in 70 of 375 (18.7%), microtrauma in 48 of 375 (12.8%), and obstetric anal sphincter injuries in 88 of 361 (24.4%; missing data in 14). One hundred seventy- four women (46.4%) showed evidence of at least one form of major pelvic floor trauma. The associations between maternal age and the different forms of pelvic floor trauma on univariate analysis are summarized in the Table .
A backward elimination approach was applied to a full multivariate model comprising age, mode of delivery, group allocation, gestational age at delivery, body mass index, and head circumference, giving a best subset model comprising only mode of delivery and age. The former was highly significant at P = .0002; the latter remained significant at P = .0268.
The trial intervention was not a confounder for the relationship between age and injury and was ineffective in preventing any form of trauma. The data were subanalyzed for each type of vaginal delivery and estimated probability of any major injury and each type of trauma as summarized in Figure 4 .



