Systemic Hypertension
Craig W. Belsha and Joseph T. Flynn
Although systemic hypertension occurs in less than 4% of the pediatric population, there is ample evidence that the roots of primary hypertension extend back to childhood. In young children, hypertension is often a sign of underlying renal or cardiac disease, but with the rise in childhood obesity, primary hypertension is now recognized as a frequent cause of hypertension in adolescents. Management of systemic hypertension in the pediatric population begins with correct blood pressure (BP) measurement using a standardized technique, categorization using current normative standards, evaluation of the etiology of the hypertension, and use of nonpharmacologic and pharmacologic therapies.
EPIDEMIOLOGY
Until more recently, the prevalence of hypertension in children has been low (1–2%). More recent data suggests, however, that blood pressure (BP) has risen among children and adolescents over the past decade attributable to an increase in weight in the pediatric population.1 Longitudinal studies begun in the 1970s in Muscatine, Iowa, and Bogalusa, Louisiana, established a relationship between body size and BP.2,3 Although height relates strongly to BP, weight remains a major determinant of BP even after adjustment for height. BP increases with age throughout childhood. Beginning with puberty, it is greater in boys than in girls. Ethnic differences in BP have also been described in some studies.
Longitudinal studies have established that the pattern of BP tracks over time. Systolic BP levels track from childhood better than diastolic BP levels. In the Bogalusa study, 40% of those with systolic BP and 37% of those with diastolic BP in the upper 20% in childhood continued to have BP above the 80th percentile 15 years later.3 Children in Muscatine, Iowa, with systolic BP levels above the 90th percentile for age and gender were at 2.5 times the risk for high adult BP than children with levels at the 50th percentile.2 Initial BP levels are the most predictive measure of the follow-up level, especially when combined with change in weight.
Obesity has risen dramatically in the United States. Among children and adolescents, rates of overweight have increased from 13.9% from 1999 to 2000 to 16% from 2003 to 2004.4 In a more recent study, it was projected that the increase in childhood obesity in the United States will result in a significant increase in obesity among 35-year-olds by 2020, which could then translate into a significant increase in adult coronary heart disease.5
Weight-related disorders such as hypertension, type 2 diabetes mellitus, hyperlipidemia, sleep disorders, and orthopedic problems are now commonly identified within pediatric practice. National survey data show a rise in the prevalence of hypertension from 2.7% from 1988 to 1994 to 3.7% from 1999 to 2002.6 Prehypertension is now reported to be present in approximately 10% of children and adolescents. National surveys have relied, however, on measurements of BP on a single occasion. More recent data from school-based screening in Houston confirm a ∼3% prevalence of hypertension after measurement on three occasions and report a prevalence of 4% to 5% among obese children.7
BLOOD PRESSURE STANDARDS AND DEFINITIONS
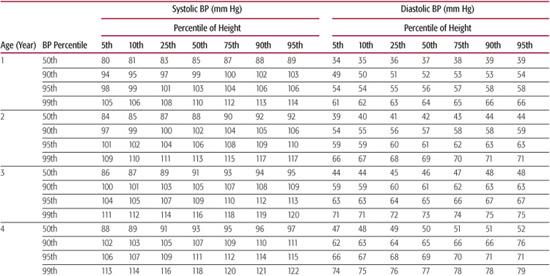
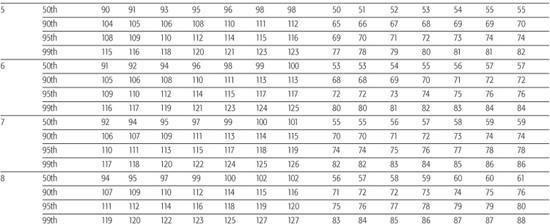
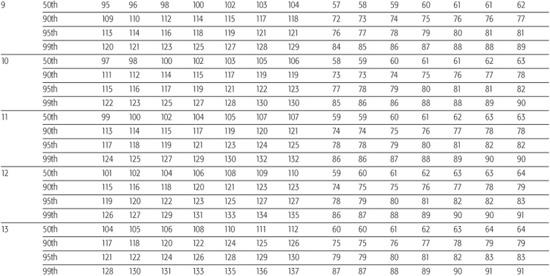
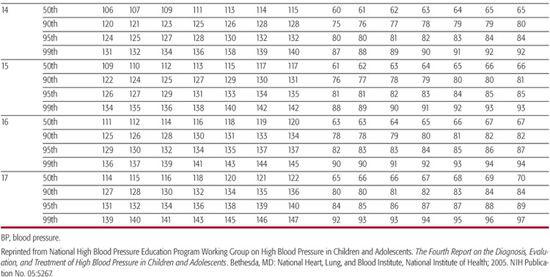
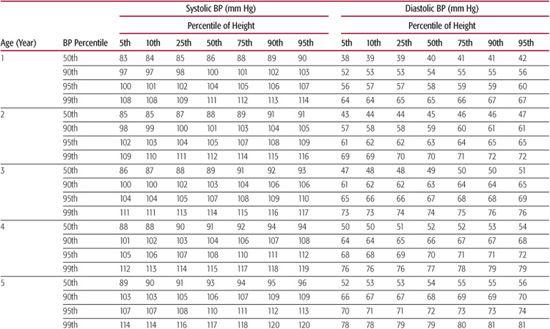
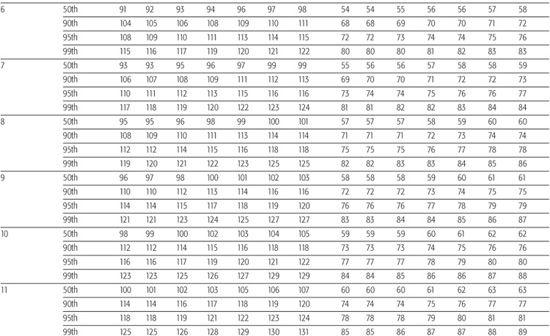
The “Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents” provides the most current information regarding normal blood pressure (BP) values from ages 1 to 17 years.8 Height is now used to define normal BP because taller children normally have higher average BP values than shorter children of the same age. A child’s height percentile, as ascertained using standard growth curves, along with his or her age and gender are used to determine the 90th and 95th percentile values as listed in Table 479-1 to classify their BP into the following three groups:
• Normal blood pressure is defined a systolic and diastolic BP below the 90th percentile for age, gender, and height.
• Prehypertension is an average systolic and/or diastolic BP between the 90th and 95th percentiles for age, gender, and height. As with adults, adolescents with BP > 120 mm Hg systolic or 80 mm Hg diastolic are considered prehypertensive.
• Hypertension is defined as an average systolic and/or diastolic BP greater than the 95th percentile for age, sex, and height.8 In asymptomatic children, it is recommended that elevated BP readings be documented on at least three occasions before labeling someone as hypertensive.
Table 479-1a. Blood Pressure Levels for Boys by Age and Height Percentile
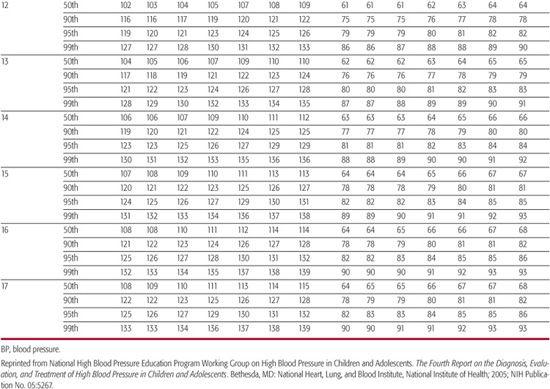
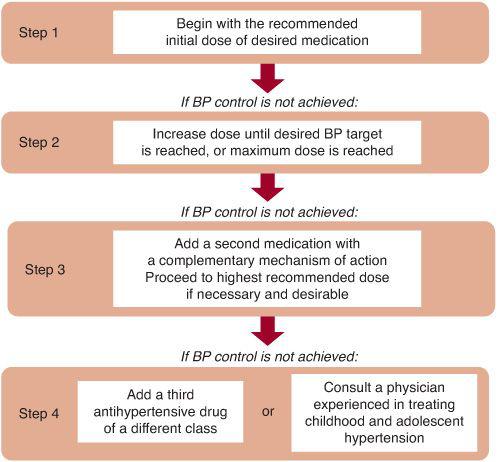
Staging of hypertension can assist in determination of children who require more immediate attention for hypertension. Stage 1 hypertension is defined as blood pressure (BP) levels that range from the 95th percentile to 5 mm Hg above the 99th percentile. If asymptomatic, these patients should undergo repeat BP measurement within 1 to 2 weeks at their source of primary care. Stage 2 hypertension is the designation for BP levels that are more than 5 mm Hg above the 99th percentile. Stage 2 hypertension requires prompt evaluation, and if persistent, is considered to be an indication for institution of antihypertensive therapy. Incorporation of BP staging in the evaluation of the child or adolescent with high BP is illustrated in Figure 479-1.
Table 479-1b. Blood Pressure Levels for Girls by Age and Height Percentile
MEASUREMENT OF BLOOD PRESSURE
Blood pressure (BP) is a constantly changing parameter. A number of factors can influence this variability, including mental and physical activity, random and systematic error(s) in measurement, and a diurnal pattern for BP.9 This variability points out the need for standardization in the BP measurement technique. The “Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents” lists the recommended technique for auscultatory BP measurement.8 This technique remains the preferred method for BP assessment because most current normative data were collected by this technique. An elevated measurement by an automated monitor using the oscillometric technique should be verified by an auscultatory measurement.8,10
It is recommended that all children beginning at age 3 years have their blood pressure (BP) measured with each medical encounter.8 Younger children also require BP measurement if they have a history of prematurity, heart or kidney disease, or other conditions that could potentially alter BP. Correct BP measurement requires an occluding cuff that is appropriate to the size of the child’s upper arm. The cuff should have an inflatable bladder width at least 40% of the mid-arm circumference and a cuff length that covers 80% to 100% of the arm circumference.8 At least seven different size cuffs are needed to appropriately fit the range of arm sizes in the pediatric population. The child needs to be cooperative with BP measurement and, if possible, not agitated or crying. Systolic BP is noted by the onset of the “tapping” Korotkoff sounds (K1). The disappearance of the Korotkoff sounds (K5) is now used as the definition of diastolic BP. BP sounds are often more difficult to hear in infants and young children. This may require that automated (oscillometric) BP measurement devices or the Doppler technique be used to determine BP in children younger than 3 years. More recent normative BP data by oscillometry for term infants in the first 12 months of life have been published.11
“White coat” hypertension is the name given to those children and adults who exhibit a persistently elevated BP in the clinic and normal BP at other times.12 To evaluate children for this problem and avoid incorrectly labeling them as having hypertension, it is often helpful to evaluate BP with out-of-office readings. Three types of “out-of-office” readings include taking BP at school, home, or with a 24-hour ambulatory BP monitor. The advantage of each method in comparison to clinic or office readings is that it allows for multiple readings over an extended period of time. There has been little formal evaluation, however, of the accuracy of home or school BP readings in the diagnosis of hypertension in pediatrics. Attention should be paid to the equipment and training of the BP observer, and circumstances surrounding the measurement. Home or school BP readings are often helpful in the day-to-day management of hypertension in children receiving antihypertensive medications to provide high and low limits for their BP on therapy.
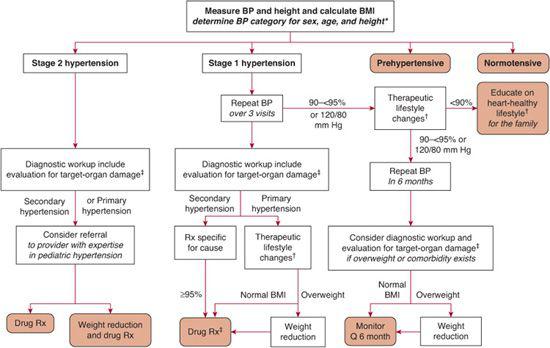
FIGURE 479-1. Management algorithm for the child or adolescent with elevated blood pressure. Rx indicates prescription; Q, every.*, See text definitions on p. 1758; †, diet modification and physical activity; ‡, especially if younger, very high BP, little or no family history, diabetic, or other risk factors.
Ambulatory blood pressure (BP) monitoring (ABPM) uses an automated device to obtain multiple (generally ∼70) BP readings in a 24-hour period. ABPM has been shown to correlate more closely with measures of hypertension end-organ damage in children such as left ventricular mass than causal BP readings.13 This method can help evaluate the child’s “usual” BP and avoid the “white coat” effect of in-office readings. Ambulatory monitoring has proven to be an extremely useful tool for the study of BP in children and adults.14-17 ABPM is now available at many pediatric referral centers and can be helpful in the evaluation of selected pediatric patients. Norms are available for children with this technique.18 Potential clinical uses for this technique in pediatrics would include (1) evaluation for “white coat” hypertension or to determine disparities in clinic and home BP readings, (2) to evaluate hypertension resistant to antihypertensive medication, (3) intermittent symptoms possibly related to BP, and (4) episodic hypertension.
ETIOLOGIES OF HYPERTENSION
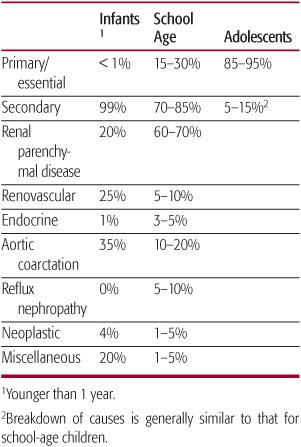
The etiologies of hypertension are typically classified into primary (essential with no identified cause) and secondary (where a specific cause is identified). The most common causes vary with age, as shown in Table 479-2. Coarctation of the aorta may be present in up to 35% of hypertensive infants younger than 1 year. Renal parenchymal disease is the most common cause of hypertension in school-age children, whereas adolescents with high blood pressure are most likely to have primary hypertension.
Table 479-2 Differential Diagnosis of Childhood Hypertension by Age
 PRIMARY HYPERTENSION
PRIMARY HYPERTENSION
The mechanisms that result in the development of primary hypertension have been the source of extensive research and controversy. Genetic and environmental factors may play a role in the development of this disorder. Primary hypertension develops more frequently among offspring of hypertensive than normotensive parents. Differences have been noted even in normotensive children with a positive versus negative family history of hypertension in carotid artery stiffness, blood pressure (BP) reactivity to mental stress, and change in BP with exercise. Twin and adoption studies have helped characterize the role of various factors on the variability of BP. Height and body mass may relate not only to genetic influence, but also to nutrition and genetic influences. High dietary sodium intake, low potassium intake, low birth weight, and serum uric acid levels may also influence risk for development of high BP. The more recent rise in obesity, however, has been the primary factor influencing the increase in this condition among adolescents.
 RENOVASCULAR
RENOVASCULAR
Renovascular hypertension results from narrowing of the arteries to one or both kidneys. This narrowing leads to relative hypoperfusion of kidney tissue, resulting in activation of the renin-angiotensin system. Renovascular hypertension may be present at all ages, but as shown in Table 479-2, is more common in younger children than adolescents. Causes of renovascular hypertension include fibromuscular dysplasia, inflammatory diseases such as Takayasu arteritis, and vascular malformations. In the neonatal period, thromboembolism from an umbilical artery catheter has been an important cause of hypertension, but the frequency of this complication has decreased in more recent years with lower (below the level of the renal arteries) placement of umbilical artery catheters. Renal artery stenosis may also develop in renal transplant recipients. Williams syndrome and neurofibromatosis are two inherited conditions with predisposition to renovascular hypertension.
Renal parenchymal disorders are commonly associated with high BP. Hypertension may develop in acute conditions, such as hemolytic uremic syndrome and acute poststreptococcal glomerulonephritis, or chronic conditions, such as polycystic kidney disease. The mechanism of hypertension is often volume mediated when renal function is reduced, but may be renin mediated in conditions such as reflux nephropathy. Children with glomerular forms of chronic kidney diseases (CKDs) in particular are at high risk for development of hypertension. Up to 80% of patients with stage 4 or 5 CKD (glomerular filtration rate < 30 mL/min/1.73 m2) have been reported to have hypertension in some pediatric centers.19
 SEVERE HYPERTENSION
SEVERE HYPERTENSION
Severe hypertension occurs when the blood pressure (BP) is significantly elevated above the normal range, usually well above BPs that would be categorized as stage 2 hypertension. In a hypertensive emergency, the patient has end-organ injury related to very high BP (eg, encephalopathy, pulmonary edema, cerebral hemorrhage). They usually have symptoms associated with high BP (eg, blurred vision, headache, nausea). The BP needs to be reduced quickly to a safer level. In hypertensive urgency, the BP may be rising or elevated, but there is no evidence of end-organ involvement. The patient may have symptoms similar to those seen in a hypertensive emergency or may be asymptomatic. The BP needs to be reduced to prevent it from continuing to rise or causing later injury (ie, becoming a hypertensive emergency). Due to confusion regarding this nomenclature, some clinicians prefer the term severe hypertension and then comment on the presence or absence of end-organ injury.
Most children with severe symptomatic hypertension have a secondary etiology for their hypertension. These etiologies are most commonly renal (renovascular or renal parenchymal) or cardiac (coarctation of the aorta) in origin. Although primary hypertension can present at diagnosis with severe (stage 2) BP elevation, this is more likely in a known hypertensive adolescent who has stopped taking antihypertensive medication. Acute cessation of clonidine and β-blockers, in particular, has been associated with a hypertensive crisis. Additional causes of severe hypertension may include use of illicit drugs such as cocaine and amphetamines. Endocrine causes such as pheochromocytoma may also cause severe hypertension.
DIAGNOSTIC EVALUATION
As alluded to in the preceding discussion, the differential diagnosis of childhood hypertension can be extensive. It is therefore important to develop some idea of likely causes before initiating any diagnostic testing. Important clues in this initial stage include the age of the child, the history, and the physical findings, especially the blood pressure (BP) values themselves.
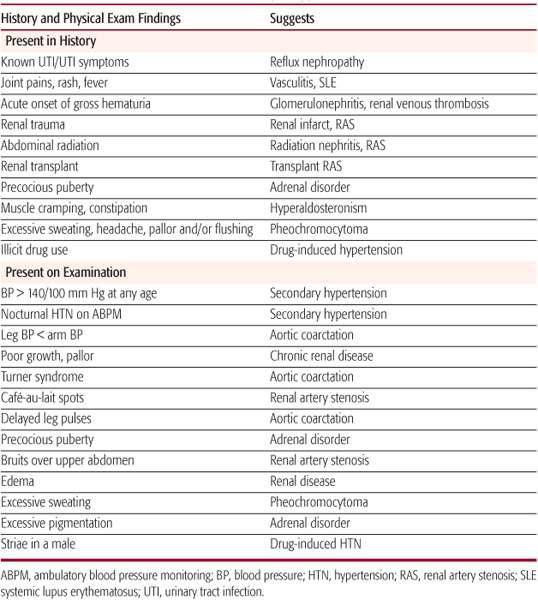
Hypertension in infants is nearly always related to an underlying cause (Table 479-2), which in many cases will be obvious once the history has been obtained and the physical examination completed. Secondary causes also account for most hypertension in preadolescent children, with renal disease being the most common. However, primary hypertension is increasing in prevalence in younger children, primarily due to the obesity epidemic. Therefore, the extensive evaluation once recommended for this age group may not be necessary if the child is significantly obese and if other findings such as a family history of hypertension are present. In adolescents, hypertension is almost always primary in origin, so a more limited diagnostic workup can be undertaken in most cases. Those teenagers with secondary causes usually have some clue to the presence of an underlying disorder in their history or physical examination (Table 479-3).
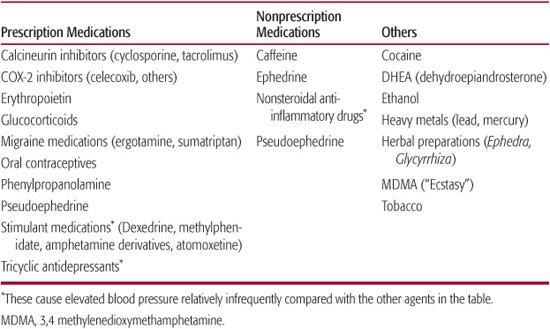
Except in infants, the history should begin by asking whether any symptoms suggestive of hypertension are present, such as headaches, dizziness, diplopia, vomiting, or epistaxis. The interviewer should then focus on eliciting symptoms of other underlying disorders, including symptoms of possible renal disease, heart disease, or diseases affecting other organ systems (Table 479-3). The past medical history should include questions about recent as well as chronic illnesses, prior hospitalizations or episodes of trauma, recurrent urinary tract infections or unexplained fevers, and neonatal history. Family history of hypertension, diabetes, kidney disease, and other cardiovascular disease (hyperlipidemia, myocardial infarction at an early age) should be elicited. Finally, it is important to ask about over-the-counter, prescription, and illicit drug use because many substances can either cause or exacerbate hypertension (Table 479-4).
The first step in the physical examination is to obtain the patient’s weight and height so that growth percentiles can be plotted and body mass index (BMI) calculated (Fig. 479-1). BPs should be obtained in both upper extremities in the seated position and in at least one arm and one leg in the supine position. If initial BPs are obtained using an automated oscillometric device, they should be confirmed by auscultation using an aneroid sphygmo-manometer. Cuff sizes should be chosen in accordance with the recommendations of the National High Blood Pressure Education Program (NHBPEP) Task Force.8 Given the high prevalence of white coat hypertension reported in more recent studies, ambulatory BP monitoring (ABPM) should be obtained if possible to confirm the diagnosis of hypertension. In addition to detecting white coat hypertension, ABPM has been shown to correlate with the presence of hypertensive target-organ damage and can also be used to help differentiate between primary and secondary hypertension.12-17,20
The remainder of the physical examination should focus on uncovering signs of specific underlying disorders that may be causing the elevated BP (Table 479-3). In obese children, there may be signs of insulin resistance such as acanthosis nigricans, or in older females, findings suggestive of polycystic ovarian syndrome (PCOS) such as hirsutism. The physical examination may also provide clues as to the severity/chronicity of the patient’s hypertension, such as left ventricular hypertrophy (signified by an apical heave) or hypertensive retinopathy.
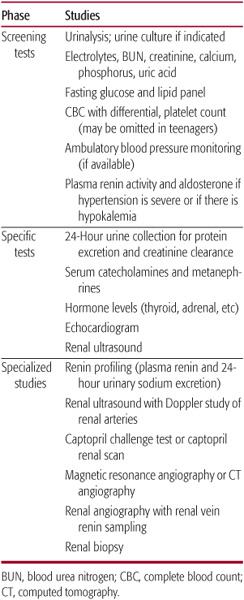
Patients with confirmed hypertension should then undergo diagnostic testing to follow up on findings from the history and physical examination, and to assess for other coexisting cardiovascular risk factors. As outlined in Table 479-5, it is customary to obtain a basic set of screening studies in all patients, which should also serve to screen for other coexisting conditions such as impaired glucose tolerance or dyslipidemia.8 Plasma renin activity and aldosterone are sometimes also included in this initial set of studies, especially when the patient’s hypertension is severe, or if both systolic and diastolic hypertension are present. Renin and aldosterone should also be obtained if there is hypokalemia on the screening electrolytes, as a suppressed renin in conjunction with hypokalemia strongly suggests a single gene disorder such as Liddle syndrome.21
Table 479-3. History and Physical Exam Findings Suggestive of Secondary Hypertension
Renal ultrasounds, which should be routinely obtained in all hypertensive preadolescent patients, may be omitted in adolescents and some older preadolescent children with stage 1 hypertension if the screening studies are normal, and if other features of primary hypertension are present, including obesity, positive family history, and isolated systolic hypertension. Those with stage 2 hypertension, with abnormal screening studies, or with diastolic hypertension should get an ultrasound. As recommended by consensus organizations,8 additional imaging studies, including renal angiography, nuclear renal scans, and voiding cystourethrograms, should only be obtained as indicated based on the results of the history, physical examination, and initial diagnostic studies.
Table 479-4. Substances That May Elevate Blood Pressure or Cause Hypertension
Given the high prevalence of left ventricular hypertrophy in hypertensive children,22,23 two-dimensional and m-mode echocardiography should be obtained to assess for the presence of hypertensive target-organ damage in patients with confirmed hypertension. Left ventricular mass should be indexed to height in meters to correct for the effect of obesity.8 Ophthalmologic exams should be obtained, but should be performed by an experienced pediatric ophthalmologist because hypertensive retinal changes are likely to be subtle in the young. At some point, carotid imaging and urine microalbumin testing may also find roles in the assessment of childhood hypertension, but more data are needed before these studies should be obtained routinely.
TREATMENT OF HYPTERTENSION
 NONPHARMACOLOGIC THERAPY
NONPHARMACOLOGIC THERAPY
Nonpharmacologic measures are currently recommended as the initial approach for children and adolescents with less severe hypertension, or those with primary hypertension and no hypertensive target-organ disease (Fig. 479-1).8 Although the magnitude of change in blood pressure (BP) may be modest, dietary modification, weight loss, and exercise have all been shown to successfully reduce BP in children and adolescents.
Although it is controversial whether excessive sodium intake may cause hypertension, once hypertension has been established, “salt sensitivity” becomes more common, and reduction in sodium intake is likely to be of benefit. Other nutrients that have been examined in patients with hypertension include potassium and calcium, both of which have been shown to have antihypertensive effects. Therefore, a diet that is low in sodium and enriched in potassium and calcium may be more effective in reducing BP than a diet that restricts sodium only. An example of such a diet is the so-called DASH (Dietary Approaches to Stop Hypertension) diet, which has been shown to have an antihypertensive effect in adults with hypertension, even in those receiving antihypertensive medication.24 Although this diet has not been systematically studied in the pediatric age group, studies in adults have shown substantial reduction of BP, particularly for individuals with hypertension with few, if any, adverse effects. Given these benefits, it is reasonable to recommend a similar diet for hypertensive children and adolescents.
Table 479-5. Laboratory Evaluation of the Child with Hypertension
Several studies have demonstrated that weight loss in obese adolescents can lower BP. Weight loss not only decreases BP, but it also improves other cardiovascular risk factors such as dyslipidemia and insulin resistance. In studies where a reduction in body mass index (BMI) of about 10% was achieved, short-term reductions in BP were in the range of 8 to 12 mm Hg. Unfortunately, weight loss is notoriously difficult and usually unsuccessful, especially in the primary care setting. However, identifying a medical complication of obesity such as hypertension can perhaps provide the necessary motivation for patients and families to institute appropriate lifestyle changes (see Chapter 32).
Increasing physical activity may also have beneficial effects on BP, particularly for children who are overweight and need to reduce their BMI. Increased physical activity may have a number of other beneficial effects such as improvement in vascular function and should be recommended for children with hypertension.25 In addition to increasing physical activity, children should have limitations placed on their sedentary time, with 2 hours/day spent on television, computers, video games, and other sedentary pursuits.26 More recent studies have demonstrated that short-term dietary and exercise interventions can result in weight loss, reduced BP, and improvements in laboratory abnormalities associated with the metabolic syndrome in overweight children and adolescents.27 Furthermore, exercise was proven to be more beneficial than metformin in preventing the development of type 2 diabetes in high-risk adults.28 These studies support the recommendation made by the National High Blood Pressure Education Program (NHBPEP) Working Group that therapeutic lifestyle changes should be considered primary therapy for obesity-related hypertension in children and adolescents. These measures should be incorporated into the treatment plan of all hypertensive children and adolescents, even those who require antihypertensive medications.
 PHARMACOLOGIC THERAPY
PHARMACOLOGIC THERAPY
The long-term adverse consequences of untreated or undertreated hypertension, specifically the development of cardiovascular and chronic kidney disease, have long been established in adults. To date, however, the long-term consequences of untreated hypertension in an asymptomatic, otherwise healthy child or adolescent remain unknown. Therefore, the decision to initiate pharmacologic therapy in the first or second decade of life can be anxiety-provoking for the pediatrician, child, and family. Lack of data on the benefits of therapy in the pediatric age group, as well as on the long-term effects of antihypertensive medications on growth and development, add further uncertainty to the decision to initiate drug treatment.
For these reasons, consensus statements issued by the National High Blood Pressure Education Program (NHBPEP)8 have emphasized that a definite indication for initiating pharmacologic therapy should be ascertained before medication is prescribed in a child or adolescent. These are generally self-explanatory:
• Stage 2 hypertension
• Symptomatic hypertension
• Secondary hypertension
• Hypertensive target-organ damage
• Diabetes (types 1 and 2)
• Persistent hypertension despite nonpharmacologic measures
Most of the indicators represent situations in which blood pressure (BP) reduction is likely to be beneficial in the treatment of another condition: for example, reduction of BP in patients with diabetes is an important strategy to prevent the development of diabetic nephropathy, and reduction of BP in patients with chronic kidney disease may slow its rate of progression.
Another uncertain area in use of antihypertensive medications in the young is how to choose the initial agent. In adults, studies such as ALLHAT have provided evidence that a diuretic or a beta-blocking agent should be the first choice of medication.29 No such evidence base exists for hypertensive children and adolescents. In addition, it should not necessarily be assumed that what works well for adults will also work well for children and adolescents. The pharmacokinetics of medications may vary by age, and the mechanism of BP elevation may also differ with age. This may lead to different classes of agents being chosen for pediatric patients. Until good data are available to discern one class of medication from another in the young, it is probably advisable to consider several classes of agents, including diuretics, beta-blocking agents, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blocker (ARB) agents, and calcium channel blockers as potentially acceptable first-line agents.8,30
Some authors have advocated a pathophysiologic approach to the choice of initial agent, for example, based on measurement of plasma renin. Those with high renin would be believed to have hypertension from renin-mediated vasoconstriction and should therefore be prescribed an antirenin agent, whereas those with low renin would be believed to have a volume overload–mediated hypertension and should be prescribed a diuretic.31 In some children, the presence of underlying renal, cardiac, or endocrine disease can guide the choice of initial agent. Drugs affecting the renin-angiotensin system are clearly preferred in those with glomerulonephritis and other forms of chronic kidney disease due to their benefit in preventing the progression to renal failure. In children with coarctation of the aorta, beta-blockade has been suggested as the appropriate choice when hypertension persists following surgical correction. Hypertensive adolescents with type 1 or type 2 diabetes should be treated with an ACE inhibitor or ARB because these agents may slow or prevent the development of diabetic nephropathy.
Other issues to consider in the choice of initial agent include the presence of another condition such as asthma or migraine headache, and the likelihood of adherence to treatment, which may be especially important in the treatment of hypertension in children and adolescents because most patients have so few symptoms. If BP control can be achieved with a single drug that is taken once a day, this will improve the likelihood of compliance with taking the medication and should be taken into consideration when the initial agent is chosen. Adverse effects of the chosen agent should also be considered. Some classes of antihypertensive agents, particularly newer ones such as ACE inhibitors and ARBs, have a lower incidence of adverse effects and may be preferable when compliance is a concern.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


