Surgical management of deep infiltrating rectal endometriosis: arguments for a conservative technique
The debate concerning the choice of the best surgical approach in the treatment of deep infiltrating endometriosis of the rectum is far from being over. Globally, the literature shows that 2 approaches are being practiced: radical rectal surgery and conservative rectal surgery.
Radical rectal surgery includes colorectal resection by complete excision of the rectal segment affected by the disease. Conservative techniques may be performed by the practice of rectal shaving, in which the rectum is not opened, or by full-thickness disc excision, in which only the endometriosis nodule along with the surrounding rectal wall is removed. Available data concerning direct comparison of those 2 approaches are provided by retrospective case series reported by surgeons who generally perform only 1 technique, and therefore those studies cannot lead to a conclusion and may only provide a hypothesis. The choice of surgeons who perform colorectal resection worldwide is supported by those retrospective studies reporting significant improvement in pain and quality of life following such a radical technique.
However, success in rectal surgery should also be evaluated in relation to both rectal function and rectal recurrence. Isolated improvement of pelvic pain and deep dyspareunia are not strong arguments supporting the success of rectal surgery, but rather supporting the success of overall endometriosis surgery. It is therefore not reasonable to justify a technique for the treatment of rectal endometriosis based only on the improvement of such general symptoms.
Conservative surgery is a philosophy opposed to that of the radical approach. The goal of such a conservative technique is maximum rectal preservation by selective excision of macroscopic endometriosis implants, in order to prevent several unfavorable outcomes in relation to rectal resection. Historically, deep endometriosis of the rectum was first treated by a conservative approach; then the practice of colorectal resection progressively increased.
To date, available data regarding postoperative digestive function do not seem to support the aggressive radical rectal surgery. In a couple of case series in which postoperative digestive function was assessed following colorectal resection, incomplete relief of preoperative digestive symptoms, including constipation, tenesmus, and dyschesia, was noted in more than half of the patients. Even though nerve-sparing techniques were prioritized, postoperative constipation was recorded in 20% of patients.
In a retrospective study comparing the digestive outcomes of those 2 surgical philosophies, patients managed during the period of time when the conservative philosophy was dominant had lower risk of postoperative constipation and an overall improvement of gastrointestinal quality of life. Extending the follow-up of this series of patients over 5 years (from 60 to 116 months) did not modify the results, as patients managed by the conservative philosophy continued to have a lower risk of constipation, better anal continence, better gastrointestinal quality of life, and no significantly increased risk of endometriosis recurrence on the digestive tract (personal communication with Horace Roman).
Data concerning colorectal resection show that such a procedure may result in major consequences, which may include the following: (1) rectal denervation due to the mobilization and section of the mesocolon; (2) stenosis of the colorectal anastomosis, which seems to be higher in incidence than that recorded in patients managed for rectal cancer; (3) reduction of the volume and compliance of the rectal reservoir, resulting in changes in both the quality and frequency of bowel movements; (4) high intracolic pressure with impact on the anal sphincter, weakening it in the long run, with consecutive urgency and fecal incontinence. As the pathophysiology of postoperative digestive dysfunction is multifactorial, prevention is aleatory even in the hands of experienced surgeons.
Conversely, a conservative technique by either rectal shaving or full-thickness disc excision requires neither mobilization of the colon nor section of the mesorectum. The shaving restores digestive function, preserves both sensitive and motor intestinal function, and improves the digestive complaints and pain symptoms. Moreover, disc excision, performed either laparoscopically or by employing transanal staplers, results in semicircular rectal sutures that are less likely to lead to digestive tract stenosis. Furthermore, the overall length of the rectum and the volume of the rectal reservoir are less reduced in the conservative technique than after colorectal resection.
Main arguments justifying systematic colorectal resection
Colorectal resection still has its place in certain conditions and should be practiced when necessary. However, it would be difficult to routinely employ such a technique whenever the rectal muscular layer is infiltrated. In the literature, myriad scientific articles support this radical policy, and the arguments for such support are mainly the same.
Reduction of recurrence risk
The literature lacks comparative studies, and therefore no evidence supports the claim of the supposedly higher risk of recurrence in patients managed by conservative surgery. It has been shown that the rate of patients with residual digestive microscopic implants may be as high as 40% when disc excision is performed. However, colorectal resection also results in specimens with positive bowel margins in 15% of cases, which may thus be responsible for colorectal proven recurrence. This leads to the fact that when radical surgery is performed instead of the conservative disc excision, colorectal resection would avoid residual microscopic implants in 25% of patients. Therefore, 4 patients should undergo colorectal resection to avoid residual microscopic disease in only 1 patient.
A large meta-analysis pooled more than 1600 patients from 49 retrospective studies, most of them being noncomparative. Seventy-one percent of patients had undergone colorectal resection, 10% had undergone full-thickness disc excision and 17% were treated with superficial surgery. Overall, the proven endometriosis recurrence rate appeared to be significantly lower in the resection-anastomosis group (2.5%; 20/812) when compared to the conservative group (5.7%; 49/865). However, the results are not as precise as they appear to be: the rate of patients lost to follow-up reached as high as 4-fold greater than that of the recurrence reported (respectively, 10% and 20% on average). The authors emphasized that the recurrence rate of endometriosis was reported in only 43% (21/49) of the included studies, while the cumulative recurrence rate was reported in only 1 study, 1 and 4 years after the surgery. The majority of studies reported a short- or mid-term follow-up (2–4 years), with a tendency of an increased recurrence rate in longer follow-up. Moreover, little data exists about the use of postoperative medical treatment, which is known to have a major impact on the rate of symptoms and lesion recurrence (8% of studies on average). For these reasons, no clear conclusion may reasonably be drawn about the actual recurrence rate related to each approach. On the other hand, if the recurrence rate is 2.5% vs 5.7%, would 3.2% excess of recurrence justify that 33 patients should undergo colorectal resection to avoid only 1 recurrence?
In a recent study where 77 patients were followed up between 5 and 10 years, and of which 4% were lost to follow-up, the risk of colorectal recurrence was 8% in the conservative approach group (4 patients out of 49) vs 0% in the radical approach group (no patient out of 25, P = .30). A second intervention due to colorectal recurrence was performed in 4 patients, among whom 2 underwent colorectal resection and 2 underwent another shaving. This means that 25 patients would have required colorectal resection to avoid a recurrence in 1 patient (Roman H, personal communication). One would wonder whether the price would not be too expensive to pay, in terms of risk of unfavorable digestive functional outcomes.
Rectal nodules responsible for digestive lumen stenosis
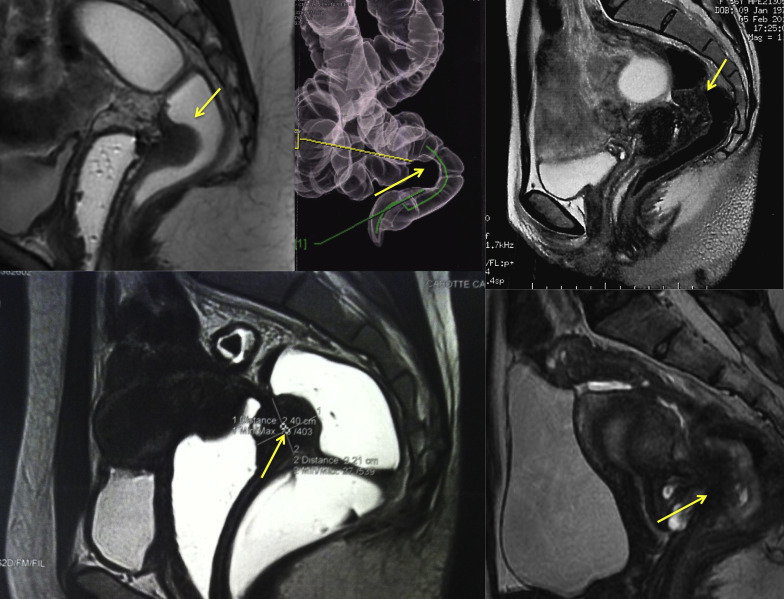
A majority of surgeons believe that rectal nodules responsible for stenosis cannot be managed by conservative surgery. However, in the ENDORE randomized trial, the feasibility of conservative surgery reached up to 93%, even though the narrowness of the rectal lumen was revealed in 73% of patients enrolled in theconservative surgery arm (Roman H, personal communication). In these circumstances, disc excision and deep rectal shaving can be routinely performed, with good functional outcomes. ( Figure 1 ).
In older women with no further pregnancy desire and who agree with a continuous postoperative therapeutic amenorrhea, deep rectal shaving is preferred, as it is enough to relieve the stenosis, and because of its good functional outcomes and low risk of postoperative complications. As microscopic endometriosis foci are likely to be left behind, in young patients the risk of recurrence is higher and may outweigh the benefit of low perioperative and postoperative complication risk. Thus, in these latter patients, the shaved area can be removed by a transanal disc excision. Deep shaving is first required in nodules responsible for rectal stenosis before disc excision, in order to completely relieve the narrowness and thus allow the administration of the transanal stapler. A superficial shaving does not allow the introduction of the stapler’s anvil further to the stenosed area and the procedure fails.
Multiple colorectal nodules
When deep endometriosis affects the rectosigmoid colon, multifocal bowel lesions can be observed in 40% or more of patients. The majority of surgeons believe that colorectal resection is the ideal treatment in those patients, even though the procedure may lead to the excision of lengthy colorectal specimens, which could reach as long as 40 cm in length. However, a conservative approach may be safely proposed, taking into consideration the distance between the 2 successive colorectal lesions.
It is most likely that conserving rectal ampulla decreases the risk of postoperative bowel dysfunction. In our series of patients managed by disc excision for deep rectal endometriosis, concomitant nodules located on the sigmoid colon were treated by either disc excision (10%) or sigmoid colon resection (6%). No unfavorable outcome was recorded, and postoperative digestive function was satisfactory. The minimum safe distance between 2 consecutive bowel sutures is not definitively defined. In our series the distance could be as short as 50 mm ( Figure 2 ). Surgeons should, however, be aware of the risk of bowel wall ischemia between 2 close sutures. The risk is reduced when performing disc excision by the preservation of the mesorectum and the mesocolon.
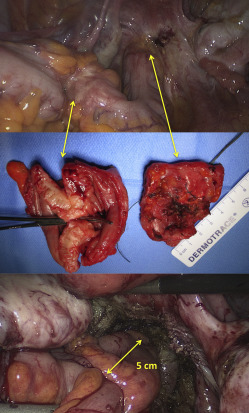
Among the patients enrolled in the ENDORE randomized trial, 1 of the patients presented with 3 distinct bowel nodules: the largest involved the low and mid rectum, measuring more than 4 cm in length; the second infiltrated 3 cm of the sigmoid colon; and the third was localized on the transverse colon extending over a length of 2 cm. Using the radical approach, a coloproctectomy would have been performed, allowing the conservation of only 3–4 cm of the low rectum, thus making the risk of bowel dysfunction more likely. The patient was instead offered the option of enrolling in the ENDORE trial and was randomized to the conservative arm. She therefore underwent 3 disc excisions, and the 4-year-postoperative close follow-up revealed a pain-free patient with normal rectal function and bowel movements.
Significant improvement in general health
In literature, the majority of scientific articles reporting series of patients managed by colorectal resection recommend such a procedure owing to the significant improvement in pelvic pain, deep dyspareunia, and overall quality of life. Fortunately an improvement is observed when such a radical surgery is performed in young women! However, the majority of series do not focus on women with impaired quality of life due to debilitating postoperative bowel dysfunction related to low rectal resection and subsequent rectal resection syndrome. As such patients only represent a minority of cases, their outcomes may have little impact on overall postoperative assessment, and are generally overlooked.
The main question is whether performing conservative surgery allows for a supplementary improvement rate, by avoiding unfavorable outcomes related to low colorectal resection. The answer is probably affirmative, since it is supported by our own results in patients managed conservatively for mid and low rectal endometriosis and in patients treated following 2 opposite surgical philosophies during 2 consecutive periods of time. A more consistent answer will be provided within a few months by the full report of the ENDORE randomized trial, where radical and conservative approaches have been directly compared.
Main arguments justifying systematic colorectal resection
Colorectal resection still has its place in certain conditions and should be practiced when necessary. However, it would be difficult to routinely employ such a technique whenever the rectal muscular layer is infiltrated. In the literature, myriad scientific articles support this radical policy, and the arguments for such support are mainly the same.
Reduction of recurrence risk
The literature lacks comparative studies, and therefore no evidence supports the claim of the supposedly higher risk of recurrence in patients managed by conservative surgery. It has been shown that the rate of patients with residual digestive microscopic implants may be as high as 40% when disc excision is performed. However, colorectal resection also results in specimens with positive bowel margins in 15% of cases, which may thus be responsible for colorectal proven recurrence. This leads to the fact that when radical surgery is performed instead of the conservative disc excision, colorectal resection would avoid residual microscopic implants in 25% of patients. Therefore, 4 patients should undergo colorectal resection to avoid residual microscopic disease in only 1 patient.
A large meta-analysis pooled more than 1600 patients from 49 retrospective studies, most of them being noncomparative. Seventy-one percent of patients had undergone colorectal resection, 10% had undergone full-thickness disc excision and 17% were treated with superficial surgery. Overall, the proven endometriosis recurrence rate appeared to be significantly lower in the resection-anastomosis group (2.5%; 20/812) when compared to the conservative group (5.7%; 49/865). However, the results are not as precise as they appear to be: the rate of patients lost to follow-up reached as high as 4-fold greater than that of the recurrence reported (respectively, 10% and 20% on average). The authors emphasized that the recurrence rate of endometriosis was reported in only 43% (21/49) of the included studies, while the cumulative recurrence rate was reported in only 1 study, 1 and 4 years after the surgery. The majority of studies reported a short- or mid-term follow-up (2–4 years), with a tendency of an increased recurrence rate in longer follow-up. Moreover, little data exists about the use of postoperative medical treatment, which is known to have a major impact on the rate of symptoms and lesion recurrence (8% of studies on average). For these reasons, no clear conclusion may reasonably be drawn about the actual recurrence rate related to each approach. On the other hand, if the recurrence rate is 2.5% vs 5.7%, would 3.2% excess of recurrence justify that 33 patients should undergo colorectal resection to avoid only 1 recurrence?
In a recent study where 77 patients were followed up between 5 and 10 years, and of which 4% were lost to follow-up, the risk of colorectal recurrence was 8% in the conservative approach group (4 patients out of 49) vs 0% in the radical approach group (no patient out of 25, P = .30). A second intervention due to colorectal recurrence was performed in 4 patients, among whom 2 underwent colorectal resection and 2 underwent another shaving. This means that 25 patients would have required colorectal resection to avoid a recurrence in 1 patient (Roman H, personal communication). One would wonder whether the price would not be too expensive to pay, in terms of risk of unfavorable digestive functional outcomes.
Rectal nodules responsible for digestive lumen stenosis
A majority of surgeons believe that rectal nodules responsible for stenosis cannot be managed by conservative surgery. However, in the ENDORE randomized trial, the feasibility of conservative surgery reached up to 93%, even though the narrowness of the rectal lumen was revealed in 73% of patients enrolled in theconservative surgery arm (Roman H, personal communication). In these circumstances, disc excision and deep rectal shaving can be routinely performed, with good functional outcomes. ( Figure 1 ).




