TRAUMA IN OBSTETRICS
Key Points
• The pregnant patient with trauma should undergo evaluation, treatment, and care for her injuries similar to the nonpregnant patient.
• While the well-being of the unborn fetus is always important, it should be considered only after the pregnant woman has undergone necessary assessment to allow appropriate stabilization and treatment efforts to begin.
• The coordinated care of the pregnant trauma patient and her fetus depends on gestational age as well as maternal and fetal status.
• Fetal viability is currently accepted as equal to or greater than 23 to 24 weeks’ gestation.
Background
Definition
• Trauma is damage to the body caused by an external force.
• Trauma can result in fracture, dislocation, sprain, intracranial injuries, internal injuries of chest or pelvis, open wound, blood vessel injury, contusion, crush injury, burn, nerve, and spinal cord injury, and it can be caused by a variety of sources:
• Forces of nature: lightning strikes, animal bites
• Mechanical forces: motor vehicle collisions (MVCs) or assault
• Self-inflicted: attempted suicide
Etiology/Epidemiology
• Trauma occurs commonly in pregnancy:
• The leading cause of death for women of childbearing age is unintentional injury (accidents) with the majority being MVCs (1).
• Falls affect 27% of pregnancies (2).
• Women aged 18 to 35 have the highest incidence of intimate partner violence with the risk of physical abuse being 1% to 20% during pregnancy (1,3,4).
Evaluation
History and Physical Exam
• MVC
• Nature of MVC: Car, motorcycle, direction of collision, vehicle rollover, ejection from vehicle, etc
• Speed of MVC: High speed, low speed, stationary
• Patient’s location in vehicle and role as passenger or driver
• Patient restrained or unrestrained
• Loss of consciousness
• Alcohol or drugs involved
• Physical abuse
• Routine screening is recommended at first prenatal visit, then in each trimester, and at postpartum visit.
 Consider use of a questionnaire.
Consider use of a questionnaire.
 Ask the patient about violence away from the partner.
Ask the patient about violence away from the partner.
 Document statements in quotations.
Document statements in quotations.
• Document any injuries in detail, including diagrams and/or photos.
• Assess safety and notify law enforcement officials of suspected abuse.
• Falls: Circumstances, area of body struck, and loss of consciousness
• Obstetric information: gestational age, obstetric history, and complications
Initial Management
• Primary survey (ABCs [airway, breathing, circulation])
• Airway
 Clear foreign bodies and suction as necessary.
Clear foreign bodies and suction as necessary.
 Establish airway with head tilt (cervical spine must be evaluated prior to moving head) and jaw thrust. Apply cricoid pressure prior with positive pressure ventilation and with endotracheal tube placement to decrease aspiration (5).
Establish airway with head tilt (cervical spine must be evaluated prior to moving head) and jaw thrust. Apply cricoid pressure prior with positive pressure ventilation and with endotracheal tube placement to decrease aspiration (5).
 Consider inserting an artificial airway device early in resuscitation to decrease the risk of aspiration keeping in mind that a smaller endotracheal tube may be needed for the pregnant patient due to edema (5).
Consider inserting an artificial airway device early in resuscitation to decrease the risk of aspiration keeping in mind that a smaller endotracheal tube may be needed for the pregnant patient due to edema (5).
 If no other airway can be obtained, a cricothyroidotomy should be performed (6).
If no other airway can be obtained, a cricothyroidotomy should be performed (6).
• Breathing
 Consider mouth-to-mouth resuscitation or intermittent positive pressure ventilation.
Consider mouth-to-mouth resuscitation or intermittent positive pressure ventilation.
 Supplemental oxygen and monitoring of oxygenation status are standard for the trauma patient until evaluation is complete (6):
Supplemental oxygen and monitoring of oxygenation status are standard for the trauma patient until evaluation is complete (6):
– Maintain maternal pulse oxygen at ≥95% for pregnancies that are ≥23 to 24 weeks’ gestation (fetal viability).
– If the exact gestational age is not known, then the presumption should be that the fetus is viable until proven otherwise.
 If inadequate ventilation is noted, the differential diagnosis includes tension pneumothorax, massive hemothorax, or flail chest with pulmonary contusion (6). These are emergent situations and require immediate intervention.
If inadequate ventilation is noted, the differential diagnosis includes tension pneumothorax, massive hemothorax, or flail chest with pulmonary contusion (6). These are emergent situations and require immediate intervention.
• Circulation
 Control obvious external hemorrhage.
Control obvious external hemorrhage.
 Obtain intravenous access.
Obtain intravenous access.
 Modification to basic life support technique at ≥20 weeks’ gestation: Manually displace the gravid uterus to the left or position the patient with a wedge under the right hip or place the woman in a modified left lateral position to prevent compression of inferior vena cava. Perform chest compressions slightly above the center of the sternum to allow for increased abdominal contents and elevated diaphragm (5).
Modification to basic life support technique at ≥20 weeks’ gestation: Manually displace the gravid uterus to the left or position the patient with a wedge under the right hip or place the woman in a modified left lateral position to prevent compression of inferior vena cava. Perform chest compressions slightly above the center of the sternum to allow for increased abdominal contents and elevated diaphragm (5).
 Advanced cardiopulmonary life support: No additional modification.
Advanced cardiopulmonary life support: No additional modification.
• Shock
 Physiologic changes of pregnancy alter normal vital sign parameters and can mask hemorrhage (see below).
Physiologic changes of pregnancy alter normal vital sign parameters and can mask hemorrhage (see below).
 Volume resuscitation should be based on other parameters (peripheral perfusion, mental status changes, diaphoresis, pallor, fetal heart rate decelerations) as well as vital signs changes.
Volume resuscitation should be based on other parameters (peripheral perfusion, mental status changes, diaphoresis, pallor, fetal heart rate decelerations) as well as vital signs changes.
 Pneumatic antishock garment may be utilized, but the abdominal portion should not be inflated in pregnancies with fetal viability.
Pneumatic antishock garment may be utilized, but the abdominal portion should not be inflated in pregnancies with fetal viability.
 The underlying etiology of reversible causes of cardiac arrest in the pregnant patient may be related to cardiac disease (myocardial infarction, aortic dissection), iatrogenic magnesium sulfate toxicity, pulmonary embolism, preeclampsia/eclampsia, amniotic fluid embolism, and anesthetic complication (high spinal) (5).
The underlying etiology of reversible causes of cardiac arrest in the pregnant patient may be related to cardiac disease (myocardial infarction, aortic dissection), iatrogenic magnesium sulfate toxicity, pulmonary embolism, preeclampsia/eclampsia, amniotic fluid embolism, and anesthetic complication (high spinal) (5).
• Secondary survey
• Further evaluation: Complete the history and physical exam (including bimanual pelvic/speculum exam, exclusion of obvious rupture of membranes, and rectal exam), laboratory values, and radiographic evaluation.
• Assessment of fetal status:
 Fetal heart tones
Fetal heart tones
 Ultrasound to evaluate
Ultrasound to evaluate
– Intra-abdominal hemorrhage and organ damage
– Fetal cardiac activity
– Fetal number
– Fetal position
– Gestational age
– Placental location and status
– Amniotic fluid volume
 Prolonged electronic monitoring of the fetal heart rate and uterine activity should be performed for the viable fetus when the mother is stable. The length of time necessary for reassurance will vary with the type and severity of the trauma, but the recommended minimum time is 4 hours (7).
Prolonged electronic monitoring of the fetal heart rate and uterine activity should be performed for the viable fetus when the mother is stable. The length of time necessary for reassurance will vary with the type and severity of the trauma, but the recommended minimum time is 4 hours (7).
• Perimortem cesarean section:
 If maternal chest compressions do not produce a pulse, consider emptying the uterus to improve resuscitation.
If maternal chest compressions do not produce a pulse, consider emptying the uterus to improve resuscitation.
 The suggested time frame to initiate perimortem cesarean section is 4 minutes. Maternal neurologic damage occurs 6 minutes after cerebral blood flow ceases. Therefore, the goal is to initiate cesarean section in 4 minutes, complete evacuation of the uterus in 5 minutes, and achieve cerebral blood flow in 6 minutes (8).
The suggested time frame to initiate perimortem cesarean section is 4 minutes. Maternal neurologic damage occurs 6 minutes after cerebral blood flow ceases. Therefore, the goal is to initiate cesarean section in 4 minutes, complete evacuation of the uterus in 5 minutes, and achieve cerebral blood flow in 6 minutes (8).
 If the maternal injuries are fatal and there is a chance the fetus will survive, proceed with cesarean delivery (9).
If the maternal injuries are fatal and there is a chance the fetus will survive, proceed with cesarean delivery (9).
Laboratory Tests
• Complete blood count.
• Comprehensive metabolic panel (electrolytes, liver function, and renal function).
• Coagulation profile.
• Amylase.
• Lipase.
• Urinalysis.
• Urine drug screen and consider blood alcohol level.
• Urine pregnancy test in reproductive age females who are not obviously pregnant.
• Blood type and screen (or crossmatch if necessary).
• Rh status to determine if Rh immune globulin needs to be given to the patient.
• Kleihauer-Betke test may be of use, but has significant limitations (10).
Radiographic Tests
• Evaluation of the pregnant patient should utilize the same tests as the nonpregnant patient, but radiation exposure to the fetus should be considered.
• Focused abdominal sonography for trauma (FAST) has been shown to be efficacious in pregnant patients (11).
• Magnetic resonance imaging (MRI) has no radiation exposure or known adverse fetal effects (12).
• X-ray and computed tomography (CT) techniques have associated radiation exposure, and parents should be appropriately counseled if time permits (Table 28-1).
• The fetus is at greatest risk at 8 to 15 weeks’ gestation for teratogenic effects from radiation exposure (13).
• Exposure to less than 5 rad has not been shown to increase fetal loss or anomalies (14).
• The pregnant uterus should be shielded whenever possible.
Table 28-1 Estimated Fetal Exposure from Radiologic Procedures (13)
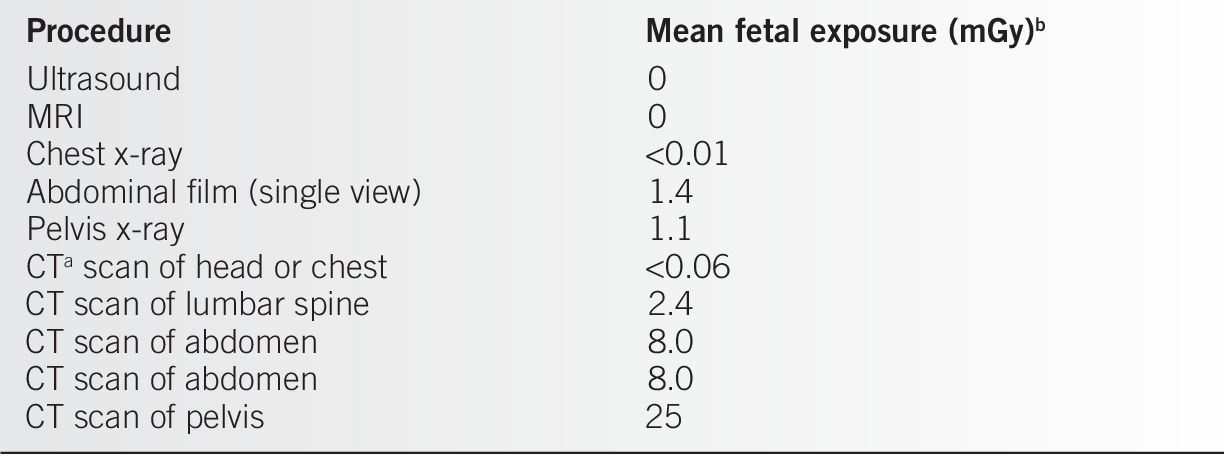
aCT, computed tomography.
b10 mGy = 1 rad
Modified from Gabbe SG, Niebyl JR, Simpson JL, et al. Obstetrics: normal and problem pregnancies. 6th ed. Philadelphia: Elsevier Saunders, 2012:140–165.
Diagnosis
Differential Diagnosis
• The differential diagnosis depends on the nature of the injury, examination of the patient, further history, and observation. For example, someone found unconscious and obtunded may have had a stroke, head injury, or overdosed on medication as just the most obvious possibilities.
• Blunt abdominal trauma.
• Etiology is frequently MVC, assault, and falls.
• Maternal injury.
 Intra-abdominal hemorrhage due to acceleration/deceleration injury with rupture or laceration of
Intra-abdominal hemorrhage due to acceleration/deceleration injury with rupture or laceration of
– Aorta, vena cava, or other vessels
– Solid organs
– Uterus
 Fetal injury
Fetal injury
– Includes skull fracture, splenic rupture, and intracranial hemorrhage (15).
– Most cases of fetal demise are related to placental abruption (7).
 Placental injury:
Placental injury:
– Frequently due to shearing force of abrupt deceleration
– Laceration
– Abruption or complete separation
– Fetal–maternal hemorrhage
• Penetrating abdominal trauma.
• Etiology is frequently gunshots or stab wounds.
• Mother or fetus may be injured by penetrating trauma.
• Uterus and/or solid organs may be penetrated, lacerated, or destroyed leading to intra-abdominal hemorrhage and/or disrupted anatomy.
• The criteria and decisions regarding proceeding with surgery are the same as in a nonpregnant female.
Clinical Manifestations
• Gestational age
• At 12 weeks’ gestation, the uterus is well protected by the bony pelvis.
• Before the fetus is viable, the mother’s health is the major concern.
• When the fetus is viable, rapid intervention may be necessary to save the mother, fetus, or both (see below).
• Type of trauma
• Motor vehicle accidents, falls, and assaults can present with minor injuries or multiple injuries involving multiple organ systems including the uterus, placenta, and fetus.
• Burns, electrical shock, and lightning strikes occur in pregnancy.
 Due to changes of pregnancy, aggressive and early fluid resuscitation is recommended (16).
Due to changes of pregnancy, aggressive and early fluid resuscitation is recommended (16).
 Carbon dioxide is readily bound by fetal hemoglobin, and therefore, supplemental oxygenation should be provided (17).
Carbon dioxide is readily bound by fetal hemoglobin, and therefore, supplemental oxygenation should be provided (17).
 Pregnant patients with these injuries should be treated the same as the nonpregnant patient.
Pregnant patients with these injuries should be treated the same as the nonpregnant patient.
Treatment
Medications
• Only medications safe in pregnancy should be administered if the fetus may survive.
• Advanced cardiac life support (ACLS) protocols and techniques do not require any dose modifications because of pregnancy.
Procedures
• Any radiologic evaluation or surgical procedure deemed necessary for treatment of the pregnant patient should be undertaken (see above).
• Surgical procedures should be performed as indicated for both fetal and maternal well-being (see section on Surgery).
Referrals/Counseling
• Obstetrician should be involved with the assessment of the mother and the fetus.
• Maternal–fetal medicine specialty consultation may be helpful in assessment and further management.
• Neonatologists may be helpful if delivery is necessary, especially in the preterm or compromised fetus.
• Involvement of other specialists is dictated by the nature of the injuries and further treatment: orthopedics, general surgery, trauma surgery, and neurosurgery, among others.
Risk Management
• As with any patient care, documentation and informed consent are paramount.
Complications
• Maternal death is uncommon (18).
• Fetal death can complicate up to 16% of pregnant trauma patients hospitalized at a level 1 trauma center (19).
• Pelvic fracture does not interfere with subsequent vaginal delivery:
• Seventy-nine percent (27/34) of women with a history of pelvic fractures (including 12 with displaced fractures) successfully delivered vaginally (20).
• Worse outcomes are typical of the pregnant trauma patient who is delivered at the time of admission due to trauma, with increased risk of maternal death, fetal death, uterine rupture, and placental abruption (18).
Patient Education
Prevention of trauma requires educating pregnant women to take specific protective measures.
• Seat belt use:
• Always wear seat belts.
• Use three-point restraint belts.
• Lap belt should be at the hips, not over the fundus.
• Improper seat belt use is a major risk factor for adverse outcomes in MVCs (21).
• Fire safety:
• Smoke detectors:
 At least one on each floor of the home is recommended.
At least one on each floor of the home is recommended.
 More than 90% of those surveyed in the United States report having smoke detectors, but fewer than 20% check every 3 months to see if they work (22).
More than 90% of those surveyed in the United States report having smoke detectors, but fewer than 20% check every 3 months to see if they work (22).
• Fire extinguisher: Only 71% of homes have a fire extinguisher (22).
• Burn prevention:
• Keep hot water heaters set at no greater than 120°F and measure the tap water temperature (22).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


