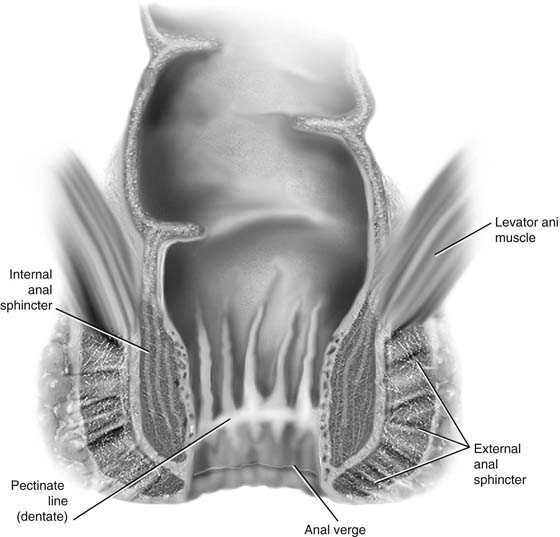
CHAPTER 100 Fecal control is a complex process that involves an intricate interaction between anal function and sensation, rectal compliance, stool consistency, stool volume, colonic transit, and mental alertness. Alteration of any of these can lead to incontinence of gas, liquid, or solid stool. Disruption of the normal anatomy of this area, usually secondary to obstetric trauma, may result in some degree of incontinence. The intact anatomy of the internal anal sphincter, external anal sphincter, and puborectalis division of the levator ani muscle must be understood to fully appreciate anatomic abnormalities that may lead to anal incontinence (Fig. 100–1). The rectum extends from its junction with the sigmoid colon to the anal orifice. The distribution of smooth muscle is typical for the intestinal tract, with inner circular and outer longitudinal layers of muscle. At the perineal flexure of the rectum, the inner circular layer increases in thickness to form the internal anal sphincter. The internal anal sphincter is under autonomic control (sympathetic and parasympathetic) and is responsible for 85% of resting anal pressure. The outer longitudinal layer of smooth muscle becomes concentrated on the anterior and posterior walls of the rectum, with connections to the perineal body and coccyx, and then passes inferiorly on both sides of the external anal sphincter. The external anal sphincter is composed of striated muscle that is tonically contracted most of the time and can also be voluntarily contracted. The external anal sphincter functions as a unit with the puborectalis portion of the levator ani muscle. The anal sphincter mechanism comprises the internal anal sphincter, the external anal sphincter, and the puborectalis muscle portion of the levator ani (see Fig. 95–1). A spinal reflex causes the striated sphincter to contract during sudden increases in intra-abdominal pressure. The anorectal angle is produced by the anterior pole of the puborectalis muscle. This muscle forms a sling posteriorly around the anorectal junction. The two sphincters are somewhat separated by the conjoint longitudinal layer formed by a merger of the longitudinal layer of the smooth muscle of the rectum and the pubococcygeal fibers of the levator ani muscle. These sphincters encircle the anal canal just distal to the anorectal angle. As was previously mentioned, the internal sphincter is thought to exert most of the resting pressure. The external sphincter, which is innervated by the inferior rectal branch of the pudendal nerve and the perineal branch of the fourth sacral nerve, exerts most of the maximal squeeze pressure. It is felt that a more anatomic repair and perhaps better restoration of a high-pressure zone will result if the repair incorporates both internal and external anal sphincters. These structures are approximately 2 cm thick and 3 to 4 cm long. The actual role of the puborectalis muscle in the incontinence mechanism is somewhat controversial. It has been thought that it supports the rectum above the level of the anorectal angle, keeping the pressure of the enteric contents as well as changes in intra-abdominal pressure away from the sphincteric complex. Recent studies suggest that fecal incontinence is often related to denervation of the pelvic diaphragm and to disruption and denervation of the external anal sphincter. FIGURE 100–1 Normal anatomy of the distal anal region. When a defect in the sphincteric complex is identified and testing reveals that this is the major factor contributing to the patient’s incontinence of gas, liquid stool, or solid stool, reapproximation of the sphincter should dramatically improve the condition. Following is a description of an overlapping sphincteroplasty repair for fecal incontinence: 1. The author prefers to perform this repair with a finger in the rectum. An initial inverted-U incision is made above the anal opening from the 9- to the 12- to the 3-o’clock position, followed by a midline incision extending up the remainder of the perineum and into the vagina (Figs. 100–2 through 100–5). 2.
Surgery for Anal Incontinence
Anatomy of the Rectum and Anal Sphincters
Repair of the Anal Sphincter
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree