Substance Use in Adolescence
Anna Maria S. Ocampo
John R. Knight
I. Description of the problem. Use of alcohol and drugs by adolescents is a major national problem. Alcohol use is associated with the leading causes of death among U.S. teenagers; including unintentional injuries (e.g., motor vehicle crashes), homicides, and suicides. Greater than 30% of all deaths from injuries can be directly linked to alcohol, and substance use is also associated with a wide range of serious problems, including school failure, respiratory diseases, high-risk sexual behaviors, transmission of HIV, gang membership, use of firearms, and other illegal activities. Early age of first use increases the risk of developing a substance use disorder during later life, and the age of onset of use among U.S. teens is falling.
A. Epidemiology.
1. According to the Monitoring the Future Study (2008), 72% of adolescents have begun to drink, 55% have gotten drunk, 47% have tried an illicit drug, and 25% have tried an illicit drug other than cannabis by the time they reach senior year in high school. Because of relatively high prevalence, experimentation with alcohol or cannabis, or getting drunk once, can arguably be considered developmental variations. However, health care clinicians should always consider recurrent drunkenness, recurrent cannabis use, or any use of other drugs as serious risks.
2. Alcohol is the most commonly used psychoactive substance among youth, more than tobacco and illicit drugs. Marijuana continues to be the most widely used illicit drug. Cigarette use among adolescents is declining and has reached its lowest level in many years. Perhaps antismoking campaigns have resulted in an increased perception of risk and disapproval. During recent years, adolescents have increasingly reported misuse of anabolic steroids, prescription medications (e.g., narcotic analgesics, stimulants, and sedatives), and over-the-counter drugs (e.g., cough and cold remedies). Adolescents may perceive pharmaceutical products as inherently less risky. The preponderance of advertisements directed at consumers gives the impression of “a pill for every ailment.” Some adolescents take these medications from parents’ medicine cabinets or homes of relatives and friends, some misuse their own prescription, and others obtain them from acquaintances or drug dealers.
3. Misuse of alcohol is found among all demographic subgroups, with higher risk associated with being male, white, and from middle to upper socio-economic status families. Despite common stereotypes, drug use may be less prevalent among inner city minority students compared to their white suburban counterparts. Rises in usage of specific illicit drugs are positively associated with the perceived availability of the drug and negatively associated with the perceived risk of harm associated with use of the drug.
B. Etiology/contributing factors.
1. Substance use during adolescence is associated with a variety of risk and protective factors, which may be characteristics of the individual, family, or community.
a. Individual risk factors include male gender, school failure, attention-deficit/hyperactivity disorder (ADHD) and learning disabilities, other co-occurring mental disorders (e.g., anxiety and mood disorders, conduct disorder), poor coping skills, nonconformity, and low religiousness. Family factors include genetic risks, a family member who is actively abusing alcohol or drugs, parent-child conflict, permissive or authoritarian parenting style, and unstable parent relationships or parental divorce. Community risks include widespread alcohol advertising, density of alcohol outlets, availability of other drugs, and substance using peers.
b. Individual protective factors include high self-esteem, internal locus of control, emotional well-being, resilient temperament, and school achievement. Family protective factors include frequent communication about alcohol and drug use, good parental modeling, involvement and monitoring, and eating meals together regularly as a family. Community protective factors include use of evidence-based prevention programs, availability of after school programs and mentoring, and monitoring of alcohol outlets.
2. Substance use disorders (SUDs) are diagnosed based on the following DSM-IV criteria: Substance abuse is defined by one or more of four criteria occurring repeatedly over the course of the past 12 months, but not meeting criteria for diagnosis of dependence:
a. Substance-related problems at school, work, or home
b. Use of substance in hazardous situations (e.g., driving a car)
c. Substance-related legal problems
d. Continued use despite problems or harm
Substance dependence is defined by meeting any three of seven criteria during the past twelve months:
a. Tolerance
b. Withdrawal (may be either physiological or psychological)
c. Using more of substance for longer periods of time than intended
d. Unsuccessful attempts to quit or cut down use of substance
e. Spending a great deal of time obtaining, using, or recovering from effects of the substance
f. Giving up important activities because of substance use
g. Continued use of substance despite medical or social problems caused by the substance
SUDs have a multi-factorial etiology, including interaction between genetic predisposition, environmental exposures during childhood, and personal choice. Twin and adoption studies have shown that alcoholism has strong genetic determinants, and recent genomic studies have shown that a number of specific genes are likely involved. Exposure to parental heavy drinking, especially during adolescence, is also associated with higher risk of substance abuse. Animal studies suggest that early nicotine use may independently increase the risk of a SUD by altering the dopaminergic pathways within the brain’s reward system.
C. ADHD and SUD.
1. Given the risk-taking tendency and impulsivity of adolescents with ADHD, they may begin experimenting with tobacco, alcohol, and drugs at an earlier age compared to those without the disorder. Furthermore, children with ADHD are at elevated risk of developing a substance use disorder later in life, and the presence of other co-occurring mental disorders raise the risk even higher. In adults, there is an overrepresentation of ADHD among those with substance use disorders (i.e., one in five adults with a SUD also has ADHD). SUDs in individuals with ADHD tend to emerge at an earlier age, follow a more severe and aggressive course, and are associated with higher rates of substance-related motor vehicle crashes and injuries.
2. Misuse and diversion of prescribed stimulants may occur among adolescents with ADHD and their peers. This is especially true among college students who are male, white, have a grade point average less than 3.5, belong to social fraternities, reside off campus, and attend the most competitive colleges. Greater than half of college students being treated with stimulant medication for ADHD are approached by their peers and asked to divert their medication. Long-acting stimulants are less likely to be misused or diverted, compared to short-acting forms.
3. Although adolescents with ADHD are at higher risk for SUD, appropriate treatment does not increase that risk. Psychostimulant therapy initiated during childhood reduces the risk of future SUD.
II. Making the diagnosis.
A. Signs and symptoms. The signs of substance use during adolescence are largely nonspecific and include: declining school performance, change in dress and friends; sudden mood swings (either depression or euphoria); drug or drug paraphernalia found in room, car or clothes; diluted or missing alcohol from parent’s home supply; stealing, lying, or missing money, including unexplained withdrawals from a bank account. Physical signs include as dilated pupils (stimulants, cocaine); constricted pupils (alcohol, opioids, sedatives); odor of alcohol on breath or appearance of obvious intoxication, or volatile odor on person or clothes (inhalants).
B. Differential diagnosis. Considerations include metabolic disorder, neurological disease, accidental poisoning, ADHD, depression, anxiety, bipolar disorder, post-traumatic stress disorder, oppositional defiant disorder, schizophrenia, bulimia nervosa, and social phobia. All of these may also co-occur with substance abuse.
C. History.
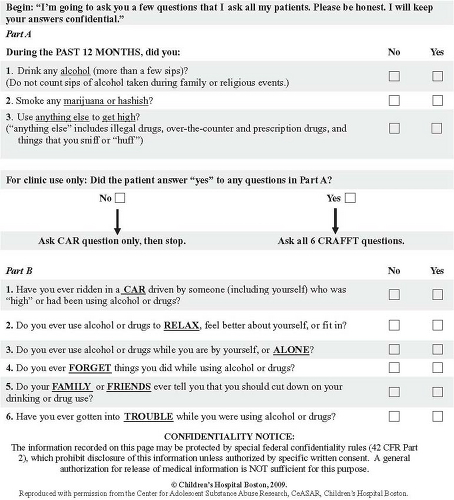
1. Screening. As part of a routine history, every adolescent should be asked about use of alcohol and drugs. “During the past 12 months, did you drink any alcohol, smoke any marijuana or hashish, or use anything else to get high”? A yes answer to any of these questions should be followed by a structured substance abuse screening tool. One
such screen is the CRAFFT test, which consists of six yes/no questions that are easy to score (each “yes” answer = 1). Key words in the test’s six items form its mnemonic (“CRAFFT”). (Fig. 78-1)
A CRAFFT total score of two or higher indicates 50% probability of a SUD diagnosis; this probability reaches 100% for a CRAFFT total score of six.
2. Assessment. A positive CRAFFT should be followed by additional alcohol and drug use history, including age of first use, current pattern of use (quantity and frequency), and impact on physical and emotional health, school and family, and other negative consequences from use (e.g., legal problems). Taking a good substance use history begins the process of therapeutic intervention. Other helpful questions:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree