KEY POINTS
• Chemical dependence or abuse is not an uncommon complication of pregnancy.
• Abuse or addiction behaviors generally do not directly impair fertility. Behaviors associated with addiction or abuse may lead to unplanned pregnancy.
• Chemical use or addiction may lead to significant adverse effects on the mother and developing child.
• Addiction is a brain disorder.
• Treatment of addiction may be successful, although success is not a certainty.
• Substitution therapy improves overall outcome in pregnant opioid addicts.
BACKGROUND
Definition
• Table 26-1 lists common agents of abuse and addiction.
• Substance-related disorders:
• A mental disorder resulting from use of a legal or illicit substance
• Examples (partial list):
 Alcohol
Alcohol
 Tobacco
Tobacco
 Sedative–hypnotics
Sedative–hypnotics
 Stimulants
Stimulants
 Psychotropic agents
Psychotropic agents
 Over-the-counter medicines
Over-the-counter medicines
• Background—diagnostic criteria:
• Recently (2013), The American Psychiatric Association (APA) revised diagnostic categorization for what are now called Substance-Related and Addictive Disorders (1).
 Dependence and abuse have been replaced with a vernacular that recognizes the dynamic spectrum of substance use disorders.
Dependence and abuse have been replaced with a vernacular that recognizes the dynamic spectrum of substance use disorders.
• Continuum Classification
• Disorders based upon a number of individual criteria—basic list (more extensive criteria for specific diagnosis for a particular substance)
 Tolerance—the need to use larger and larger amounts of the substance in order to obtain an effect
Tolerance—the need to use larger and larger amounts of the substance in order to obtain an effect
 Withdrawal—adverse physical or psychological manifestations from discontinuation of the substance
Withdrawal—adverse physical or psychological manifestations from discontinuation of the substance
 Increased usage
Increased usage
 Ineffective self-efforts to cut down on use
Ineffective self-efforts to cut down on use
 Drug-seeking behaviors (going to multiple pharmacies, theft of medication)
Drug-seeking behaviors (going to multiple pharmacies, theft of medication)
 Important social, recreational, or occupational activities discontinued in order to consistently facilitate the use of the substance (abandonment of children, repeated loss of job)
Important social, recreational, or occupational activities discontinued in order to consistently facilitate the use of the substance (abandonment of children, repeated loss of job)
 Continued use of substance despite known physical or mental problems resulting from the substance (smoking despite the diagnosis of emphysema, drinking in the face of hepatic cirrhosis)
Continued use of substance despite known physical or mental problems resulting from the substance (smoking despite the diagnosis of emphysema, drinking in the face of hepatic cirrhosis)
• Specific diagnosis criteria for a particular substance should be specifically referenced through the Diagnostic and Statistical Manual of Mental Disorders.
• “Addiction” operationally implies loss of control and increased use of the agent(s) despite overwhelming reasons not to.
• Instead of classification as abuse or dependence, classification based upon severity:
 Mild disease—presence of two to three criteria or symptoms
Mild disease—presence of two to three criteria or symptoms
 Moderate disease—presence of four to five symptoms
Moderate disease—presence of four to five symptoms
 Severe disease—presence of six or more symptoms
Severe disease—presence of six or more symptoms
• Environment and duration of remission are important.
 Early remission—criteria for full diagnosis no longer present for 3 to 12 months
Early remission—criteria for full diagnosis no longer present for 3 to 12 months
 Sustained remission—criteria for full diagnosis no longer present for greater than 12 months
Sustained remission—criteria for full diagnosis no longer present for greater than 12 months
 Specify if in a controlled environment (treatment facility, incarceration, etc.)
Specify if in a controlled environment (treatment facility, incarceration, etc.)
• Substance use disorder in pregnancy:
• Involves substance abuse or dependence in the periods immediately prior to conception, during pregnancy, or postdelivery
Table 26-1 Common Drugs of Abuse and Addiction
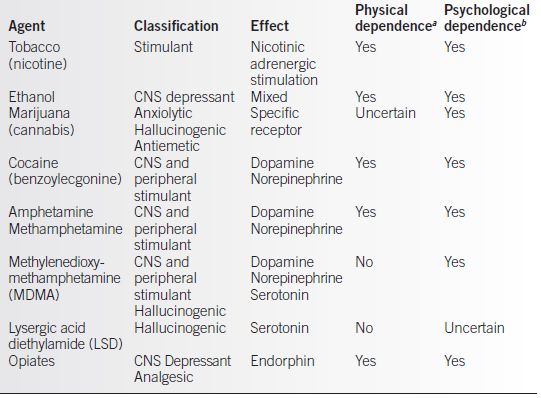
aPhysical dependence, evidence suggestive of at least some physical effects or systems after abrupt discontinuation of chemical use.
bPsychological dependence, evidence suggestive of at least some desire of altered neurobehavior, or host neurochemistry after chronic use.
CNS, central nervous system
Data referenced in text.
Pathophysiology
• The pathophysiology of dependence is complex. Addiction, like other disease processes, requires the following interactions (2,3):
• Agent or substance of abuse:
 Availability of an agent may affect its use.
Availability of an agent may affect its use.
– Cost may affect use habits (crack cocaine availability and cost reduced the financial burden necessary to be exposed to cocaine).
 Societal influences:
Societal influences:
– Acceptability of social drinking makes alcohol widely available.
– Negative implications of illegal use of drugs of abuse.
 Psychoactive efficacy:
Psychoactive efficacy:
– Greater pleasurable efficacy increases the addictive potential of an agent.
– Onset of action and cerebral bioavailability.
∗ Rapid onset of action and cerebral bioavailability increases the addictive potential of an agent (e.g., crack cocaine, intravenous fentanyl).
• Host susceptibility
 Genetic influences:
Genetic influences:
– Genetic differences may exist with agent absorption, brain receptor susceptibility to the effects of an agent, or the remodeling of brain receptors caused by exposure to a substance.
 Familial host vulnerability:
Familial host vulnerability:
– Chemical exposure.
 Comorbidity with other psychiatric disorders has been shown to occur.
Comorbidity with other psychiatric disorders has been shown to occur.
– The cause-and-effect relationship between other psychiatric disorders and addiction is not fully established.
• Environmental effect
 Occupations that allow less structured exposure to a given substance may increase the likelihood of abuse or dependence (e.g., bartenders, anesthesiologists, those with solitary unstructured jobs, sex trade industry worker).
Occupations that allow less structured exposure to a given substance may increase the likelihood of abuse or dependence (e.g., bartenders, anesthesiologists, those with solitary unstructured jobs, sex trade industry worker).
 Peer group influences may affect exposure and choice of the agent.
Peer group influences may affect exposure and choice of the agent.
– An alcoholic spouse increases the chance that his or her mate is an alcoholic.
 Cultural perspective and perceptions may affect the mechanisms of and types of substance exposure (4).
Cultural perspective and perceptions may affect the mechanisms of and types of substance exposure (4).
 Social instability may increase both the population exposure to a substance and may reduce social disincentives to abuse or become dependent.
Social instability may increase both the population exposure to a substance and may reduce social disincentives to abuse or become dependent.
• Substance use and dependence in women often exhibit specific pathophysiologic manifestations:
• Chemically dependent women are more likely to have other concurrent psychiatric diagnoses than women without addiction disorder (5).
• Spousal abuse, domestic violence, and prostitution are seen more frequently in women with chemical dependence (6,7).
• A smaller circulatory volume of distribution gives women, on average, a greater exposure, effect, and abuse liability than men given a similar substance use history (8).
 The progression of addiction, with the inevitable deterioration of the dependent patient, frequently occurs much more rapidly in women than in men (9).
The progression of addiction, with the inevitable deterioration of the dependent patient, frequently occurs much more rapidly in women than in men (9).
Epidemiology
• The prevalence of substance abuse or dependence during pregnancy is not precisely defined.
• More than 10 years ago, the National Institute on Drug Abuse (NIDA) surveyed 2613 women (10).
 20.4% of women smoked cigarettes during pregnancy.
20.4% of women smoked cigarettes during pregnancy.
 18.8% of women used alcohol during pregnancy.
18.8% of women used alcohol during pregnancy.
 5.5% of pregnant women used illicit drugs during pregnancy.
5.5% of pregnant women used illicit drugs during pregnancy.
• A more recent assessment (11) of substance abuse among women during and after childbirth indicates
 Alcohol, tobacco, and illicit substance use was higher in nonpregnant adult women.
Alcohol, tobacco, and illicit substance use was higher in nonpregnant adult women.
 Pregnancy use declines as pregnancy progresses.
Pregnancy use declines as pregnancy progresses.
 Resumption of intemperate use often occurs within the first 3 months after childbirth.
Resumption of intemperate use often occurs within the first 3 months after childbirth.
• Despite conventionally held wisdom to the contrary, socioeconomic and ethnic differences were not noted in at least one large study (12).
• Substance abuse and dependence disorders are more common in males than in females; however, trends in usage may be changing (13).
 In a recent survey of 12- to 17-year-olds, comparable rates of alcohol, tobacco, cocaine, and heroin use were found among males and females (14).
In a recent survey of 12- to 17-year-olds, comparable rates of alcohol, tobacco, cocaine, and heroin use were found among males and females (14).
 Tobacco use during pregnancy for women 18 and 19 years of age was higher than that of any other age range (15).
Tobacco use during pregnancy for women 18 and 19 years of age was higher than that of any other age range (15).
 Adolescent girls and women greater than 35 years of age have greater rates of abuse and dependence on psychotherapeutic drugs than men (16).
Adolescent girls and women greater than 35 years of age have greater rates of abuse and dependence on psychotherapeutic drugs than men (16).
EVALUATION
Laboratory Tests
• Drug screen testing
• Most illicit substances and prescription drugs may be detected in maternal body fluids (16).
• Factors affecting performance of testing include
 Volume of distribution and elimination of specific agents
Volume of distribution and elimination of specific agents
– Ethanol is difficult to effectively screen for more than a few hours after ingestion, and urine testing is not reliable (17,18).
– Agent persistence makes marijuana and long-acting benzodiazepines detectable for several weeks after exposure.
 Tissue or body fluid analyzed
Tissue or body fluid analyzed
 Time from last exposure until testing performed
Time from last exposure until testing performed
 Cumulative dose of agent ingested by host
Cumulative dose of agent ingested by host
 Performance characteristics of specific testing methodology
Performance characteristics of specific testing methodology
 Cross-positive results from legitimately administered substances (e.g., testing of the postoperative patient may demonstrate positive test results secondary to anesthetic or analgesic agents legitimately prescribed)
Cross-positive results from legitimately administered substances (e.g., testing of the postoperative patient may demonstrate positive test results secondary to anesthetic or analgesic agents legitimately prescribed)
• Drug screen testing involves several ethical and legal issues (19,20):
 Consent:
Consent:
– Depending on the locale, general “consent for diagnosis and treatment” versus specific permission for drug testing may be required.
 Chain of custody issues (21):
Chain of custody issues (21):
– In most hospital emergency departments, clinical laboratories, or clinic reference labs, testing is evidentiary in a general sense (not unlike other hospital lab tests).
– Chain of custody testing generally implies specific relevance insofar as the legal system and employment are concerned.
 Chain of custody testing usually requires specific consent from the screened individual.
Chain of custody testing usually requires specific consent from the screened individual.
• Clinical testing policy:
 Selective toxicology testing is the testing of patients based on an increased, perceived risk of abuse or dependence.
Selective toxicology testing is the testing of patients based on an increased, perceived risk of abuse or dependence.
 Universal toxicology testing is blanket testing of all pregnant patients presenting for care.
Universal toxicology testing is blanket testing of all pregnant patients presenting for care.
 Selective testing is less intrusive, while universal testing is more sensitive for detection in a mixed or less rigorously screened population.
Selective testing is less intrusive, while universal testing is more sensitive for detection in a mixed or less rigorously screened population.
 Universal testing is more costly than selective testing.
Universal testing is more costly than selective testing.
• Types of drug testing:
 Blood
Blood
 Urine
Urine
 Salivary
Salivary
 Hair
Hair
 Amniotic fluid or meconium
Amniotic fluid or meconium
– May detect fetal exposure for some time after maternal exposure (22)
DIAGNOSIS
Clinical Manifestations
• The clinical diagnosis of addiction is made based upon diagnostic criteria previously described (refer to the definitions in the substance abuse and substance dependence sections).
• Frequently, substance abuse and substance dependence in women are seen in association with several other comorbid conditions and psychosocial cofactors (7):
• Domestic violence
• Poor general health
• Sexually transmitted diseases
• Sexual exploitation, maternal incest, or sexual victim history
• Obstetric conditions that may be associated with substance abuse or dependence include
 Intrauterine growth restriction
Intrauterine growth restriction
 Preterm labor or preterm birth
Preterm labor or preterm birth
 Abruptio placentae
Abruptio placentae
• As evidenced by the broad socioeconomic prevalence of substance abuse and dependence in pregnancy:
 Medical and social comorbidities often do not become clearly apparent until fairly late in the natural progression of addiction.
Medical and social comorbidities often do not become clearly apparent until fairly late in the natural progression of addiction.
 Behavioral signs or symptoms in the early-stage disease may be confused with other factors such as noncompliance with care.
Behavioral signs or symptoms in the early-stage disease may be confused with other factors such as noncompliance with care.
• Continued tobacco use (smoking) during pregnancy, without apparent efforts to reduce use, is evident more frequently in those with other abuse or dependence disorders (11,22,23).
• Psychiatric comorbidity is seen more commonly in women than in men with the diagnosis of chemical abuse or dependence.
 One in five women with alcohol abuse or dependence also fulfill the diagnostic criteria for depression (four times more common than in males) (22,24).
One in five women with alcohol abuse or dependence also fulfill the diagnostic criteria for depression (four times more common than in males) (22,24).
 Anxiety disorders are the most common group of psychiatric disorders in women (7).
Anxiety disorders are the most common group of psychiatric disorders in women (7).
 The most common psychiatric disorders in addicted pregnant women are personality—the diagnosis may not be accurate secondary to inherent inaccuracy in codiagnosis of addition and personality disorders (7,25).
The most common psychiatric disorders in addicted pregnant women are personality—the diagnosis may not be accurate secondary to inherent inaccuracy in codiagnosis of addition and personality disorders (7,25).
 Women with borderline personality disorder diagnosis frequently have an associated history of childhood or partner sexual trauma.
Women with borderline personality disorder diagnosis frequently have an associated history of childhood or partner sexual trauma.
• For alcohol abuse and dependence assessment, several interview-based screens have been validated for use in pregnancy (26):
 T-ACE (27)
T-ACE (27)
– Tolerance
– Annoyed
– Need to cut down
– Eye opener (morning drinking)
 TWEAK (28)
TWEAK (28)
– Tolerance
– Others worried about your drinking
– Eye opener
– Amnesia
– Need to (K) cut down
 NIAAA Questionnaire (Table 26-2) (29)
NIAAA Questionnaire (Table 26-2) (29)
• General substance screening in pregnant women may not only identify addictive behavior but may also identify maternal at-risk behavior and fetal exposure–directed intervention.
 Use of the 4P + screen is a good general screen for all illicit substances (30).
Use of the 4P + screen is a good general screen for all illicit substances (30).
 Composite scales that result in a screening profile score may be useful for screening in a diverse pregnant population (31).
Composite scales that result in a screening profile score may be useful for screening in a diverse pregnant population (31).
TREATMENT
General Principles
• There are currently no singularly effective treatments for chemical dependence.
• There are currently no Food and Drug Administration–approved pharmacologic treatments for chemical dependence in pregnancy.
 Medical treatment of chemical dependence during pregnancy involves the balancing of the known risks to the mother and fetus from the use of the agent, with the possible or unknown effects from use of a medication to treat detoxification or help manage recovery.
Medical treatment of chemical dependence during pregnancy involves the balancing of the known risks to the mother and fetus from the use of the agent, with the possible or unknown effects from use of a medication to treat detoxification or help manage recovery.
• Pregnancy notwithstanding, pharmacotherapy regimens are available for dependence disorders of the following agents:
 Alcohol
Alcohol
 Tobacco
Tobacco
 Narcotics (opiates)
Narcotics (opiates)
• Detoxification and withdrawal management are different from recovery treatments.
 Detoxification and withdrawal treatment involves the short-term management of acute cessation of regular use of the agent of dependence.
Detoxification and withdrawal treatment involves the short-term management of acute cessation of regular use of the agent of dependence.
– Detoxification is stopping the use of the agent of addiction.
 Recovery treatment involves initiation of the process of managing the addiction itself, with the goal of therapy being long-term abstinence from the use of the agent and elimination or reduction of the behaviors associated with the addiction.
Recovery treatment involves initiation of the process of managing the addiction itself, with the goal of therapy being long-term abstinence from the use of the agent and elimination or reduction of the behaviors associated with the addiction.
– Recovery treatment is increasing the likelihood of the dependent individual not wanting and not starting the use of the agent again.
• Because addiction is a medical–psychological–social disease, pharmacotherapy alone is rarely successful.
• Additional nonpharmacologic treatments of dependence disorders include
 Twelve-step programs
Twelve-step programs
 Treatment of medical complications of addiction
Treatment of medical complications of addiction
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


