Stroke and Cerebrovascular Disease
Michael J. Rivkin
Stroke denotes the sudden onset of a focal neurologic deficit and most often includes the abrupt appearance of weakness. Interruption of blood flow to a part of the central nervous system (CNS) usually underlies the resultant weakness. Because most strokes in children are related to focal cerebral involvement, the most common clinical manifestation is the abrupt appearance of hemiparesis. Less frequently, the cause of stroke involves the brainstem, cerebellum, or spinal cord. The functional consequences always reflect the neuroanatomic features of the affected CNS region. Either focal cerebral ischemia or hemorrhage may cause the clinical manifestations of stroke. Further, ischemic stroke in children is attributable to either arterial ischemic stroke (AIS) or to cerebral sinovenous thrombosis (CSVT). This chapter addresses these causes of focal cerebral injury in children. First, epidemiologic features of stroke in children will be presented. Consideration will then be directed to the occurrence of pediatric cerebrovascular disease in neonates as well as in older children. Emphasis will be placed on the pathogenetic, clinical, diagnostic, and therapeutic aspects of the varied causes of strokes in children.
EPIDEMIOLOGY
Stroke in children follows a biphasic pattern of occurrence. Its occurrence is highest among newborns and occurs less frequently in children greater than 30 days of age. Among neonates, studies indicate an occurrence of stroke that approximates a frequency of 1 in 4000 births.1-3 Arterial ischemic stroke accounts for 80% of these occurrences, although 20% are due to cerebral sinovenous thrombosis (CSVT) and hemorrhage (excluding intraventricular and subarachnoid hemorrhages).4,5
Several studies of stroke in children older than age 1 month, performed over the last three decades have reported an occurrence of stroke at a rate of approximately 2 in 100,000 per year.6-8 However, recent studies suggest that the frequency may be greater and as high as 13 in 100,000 per year.5,9 Strokes occur more often in males than in females and more frequently in African Americans and Caucasians.
PATHOGENESIS
Ischemic injury to the brain occurs as a result of one of three different mechanisms: embolism, thrombosis, or diminished systemic perfusion. Embolic damage to the brain occurs when material formed at a site in the vascular system proximal to the brain lodges in a blood vessel, blocking cerebral perfusion. Emboli originate most commonly from the heart, arising from clots on cardiac chamber walls or from vegetations on valve leaflets. Congenital heart disease that includes right-to-left shunt predisposes to such embolus formation. Artery-to-artery emboli are composed of clot or platelet aggregates that originate in vessels proximal to the brain but ultimately come to rest and to occlude flow in vessels critical for cerebral perfusion. Intravascular embolus formation is promoted by some forms of thrombophilia (see below). Thrombosis denotes vascular occlusion resulting from a localized process within a blood vessel or vessels. Although atherosclerosis underlies most thrombotic processes affecting adults, it is a very uncommon cause of thrombosis in children. Localized luminal clot formation occurs in polycythemia or in a hypercoaguable state. Alternatively, anatomic abnormalities may lead to clot formation or mechanical obstruction in fibromuscular dysplasia, focal arteriopathies, or vascular malformations. Should systemic pressure decline enough to compromise cerebral perfusion, the central nervous system may suffer injury as a result of diminished systemic perfusion. Cardiac pump failure (related to congenital heart disease and its surgical repair), as well as systemic hypotension due to hypovolemia, represents common causes of hypotensive cerebral ischemic injury. Often, in the circumstance of diminished cerebral perfusion, brain injury is much more diffuse than that found in the more focal injuries characteristic of thrombotic and embolic cerebral events. Cerebral ischemia serves as the final common pathway leading to brain injury irrespective of whether an embolic, thrombotic, or hypoperfusive mechanism has caused the stroke.
Both thrombotic and embolic strokes may be heralded by the occurrence of transient ischemic attacks (TIAs). Transient ischemic attacks are brief episodes of focal, nonconvulsive neurologic deficit attributable to interruptions of cerebral perfusion. Similar to stroke, the onset is abrupt. However, a TIA episode lasts less than 24 hours and recovery is complete. Despite full recovery, the TIA can serve as a sentinel event of subsequent episodes that may result in fixed deficits. Importantly, signal correlates of a TIA may not be present on magnetic resonance imaging (MRI) of the brain.10
Hemorrhage occurs when blood is released into the extravascular, intracranial, or intraspinal space. In this circumstance, focal injury of brain or spinal tissue occurs as a result of pressure exerted by the space-occupying mass of blood, as well as hemorrhage-related ischemia. Such injury can be exacerbated by the damaging effects upon neural tissue of substances released in the blood. Epi- and subdural hemorrhages represent intracranial collections of blood separated from brain parenchyma by dural or arachnoid membranes. Subarachnoid hemorrhage occurs when blood flows out of the intracranial vascular bed and onto the surface of the brain to admix with cerebrospinal fluid in the subarachnoid space. Intracerebral hemorrhage denotes bleeding into the parenchyma of the brain.
NEONATAL STROKE
Stroke in neonates may be considered as perinatal stroke, which has been defined to occur during the fetal or neonatal periods but before 28 days after birth.4,11 Stroke differs from the intraventricular hemorrhage observed in premature infants and discussed in Chapter 58. Eighty percent of strokes in neonates are arterial and ischemic (AIS). The remaining 20% are attributable to either cerebral sinovenous thrombosis (CSVT) or hemorrhage. Interestingly, a left hemispheric location has been noted to be the most common in neonatal AIS, a lateralization for which no proven explanation has been found.12 Neonatal CSVT may cause focal infarction or hemorrhage. Cerebral veins conduct deoxygenated blood from the parenchyma to the dural sinuses. These sinuses—the sagittal, straight, transverse, cavernous, and petrous—convey the blood to the jugular vein for return to the cardiopulmonary circulation. Thrombotic occlusion of flow anywhere in these venous conduits can lead to increased venous pressure, ischemia, and sometimes, infarction that can be hemorrhagic (Fig. 552-1).13
Risk factors associated with perinatal stroke have received limited investigation but include maternal and placental disorders, perinatal asphyxia, blood disorders including polycythemia, congenital cardiac disorders, infection, trauma, and drug exposures. In particular, the role of hypercoaguable states associated with prothrombotic risk factors such as factor V Leiden (FVL), prothrombin 20210 mutations, elevated concentrations of lipoprotein (a), homocysteine, factor VIIIC, anticardiolipin antibodies (ACA), and deficiencies of protein C and protein S have been implicated14 (see also Chapter 438). Although recurrent thromboembolic stroke is not common in infants, abnormality of lipoprotein (a), hyperhomocysteinemia, and protein C deficiency in the setting of underlying systemic disease may increase the chance of recurrence. Both maternal and infant characteristics may be related to the occurrence of cerebral sinovenous thrombosis (CSVT). Maternal risk factors may include preeclampsia, gestational diabetes, and chorioamnionitis.15,16 Frequent association between systemic illness and CSVT has been recognized in infants and includes dehydration, sepsis, congenital cardiac defects, extracorporeal membrane oxygenation, and meningitis.13,16,17 Although the role of thrombophilia in neonatal CSVT has not been proven, factor V Leiden (FVL), prothrombin 20210, and methylene tetrahydrofolate reductase (MTHFR) mutations have been suggested as factors that may promote the occurrence of CSVT in neonates.15,18 Importantly, more than one risk factor has been found simultaneously among many infants with CSVT.16,19 Thus, a combinatorial or synergistic mechanism may underlie many occurrences.
Seizure often is the first indication of AIS in the neonate.20,21 However, seizure may also be accompanied by signs of encephalopathy in newborns with AIS.22 Neonatal CSVT also commonly presents as seizure.15,23,24 However, other symptoms can include apnea, respiratory distress, feeding difficulty, hypotonia, and apnea. Indeed, CSVT can present in an infant as unexplained lethargy, alone.24
Because both AIS and CSVT in the newborn commonly present as seizure, an electroencephalogram (EEG) is often obtained. Evidence of localized dysfunction of the brain found on an EEG consists of focal persistent voltage reduction or of marked focal slowing and sharp wave activity. Periodic lateralized epileptiform discharges (PLEDS) may be present. In some instances electrographic evidence of clinically observed seizures may be found. Each of these findings may exist while the EEG remains relatively less affected over other regions of the brain. The areas of electrical abnormality should correspond to the affected areas of the brain revealed by neuroimaging.
Head ultrasound (HUS) serves as a noninvasive method of neuroimaging that offers the considerable advantage of bedside use. The sensitivity of head ultrasound is low and acute stroke in the neonate can be missed.25 Cranial computerized tomography (CCT) provides good fidelity in the identification of focal ischemia. However, magnetic resonance imaging (MRI) provides superior ability to identify ischemic foci in brain. The addition of diffusion tensor MR imaging provides superior sensitivity to that of CCT for identification of early focal ischemia. Moreover, MRI imparts no exposure to ionizing radiation, a considerable advantage of this modality over CCT.26 A combination of T1-weighted (T1W), T2-weighted (T2W), and diffusion weighted imaging (DWI) is most effective in the early identification of focal stroke in the neonate.27
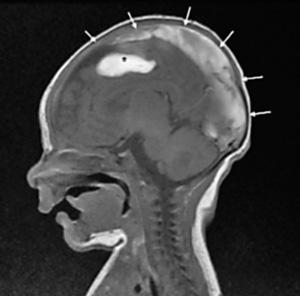
FIGURE 552-1. Neonate with cerebral sinovenous thrombosis (CSVT). Sagittal T1-weighted image shows enlarged and thrombosed superior sagittal sinus (arrows). An associated area of hemorrhagic infarction is seen within the subjacent frontal lobe (asterisk).
Treatment is supportive and symptomatic. Anticonvulsant treatment is given if seizures have occurred. Phenobarbital remains the preferred drug and is administered as a loading dose of 20 mg/kg. Maintenance therapy of 3 to 5 mg/kg/day can be divided into twice daily doses. Attention should be given to hydration state, acid-base balance, and hematocrit. Deficits should be corrected. Treatment of underlying infection, metabolic disarray, or coagulopathy is necessary. Anticoagulation therapy with low molecular weight heparin (LMWH) or unfractionated heparin (UFH) is not used as a matter of routine in this age group but can be considered in selected neonates with severe thrombophilic disorders, multiple emboli to brain, or evidence of propagating CSVT despite supportive therapy (see below).28 Further investigation on the use of anticoagulation in neonates with focal stroke is needed.
Both motor and cognitive disabilities have been associated with perinatal stroke. Seizure during the neonatal period or neurologic abnormality on discharge have been associated with both these deficits.12 Infants with perinatal stroke due to thrombophilia have been identified to be at risk for long-term neurologic deficit.29 Cognitive deficits often manifest by two years of age.30 Magnetic resonance imaging appears to be helpful in predicting outcome. Concomitant involvement of ipsilateral basal ganglia, corpus callosum, and the posterior limb of the internal capsule has been found to predict lasting hemiparesis.31 Further work is needed concerning neurodevelopmental outcome.
ETIOLOGIES AND CLINICAL FEATURES OF STROKE IN CHILDREN OLDER THAN ONE YEAR
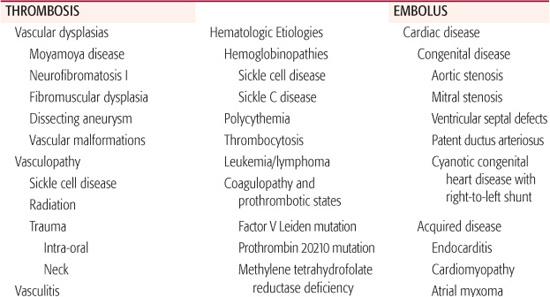
Stroke occurs less frequently in older children than it does in newborns. Despite its relative infrequency in this age group, myriad etiologies exist. Nonetheless, the etiologies may be grouped according to whether the stroke is attributable to an embolic, thrombotic, or hemorrhagic cause. Causes of stroke in children are listed in Table 552-1 and are discussed below
 THROMBOSIS
THROMBOSIS
Vascular Dysplasia
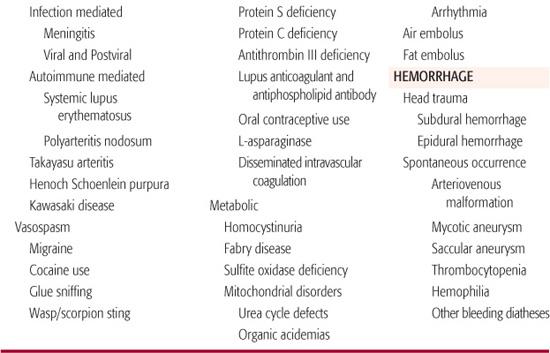
Moyamoya disease is observed most commonly in children under the age of 15 years. This chronic condition is characterized by stenosis or occlusion of the terminal internal carotid arteries resulting in a characteristic development of an abnormal vascular network in the vicinity of the arterial occlusion (Fig. 552-2). The Japanese word moyamoya (meaning “puff of cigarette smoke”) was selected to describe this condition because of the characteristic appearance of this reactive vascular network on angiography. The network of collateral vessels arises principally from the external carotid circulation in response to relative tissue hypoxia. This phenomenon has been associated with increased central nervous system concentrations of angiogenic factors and creates an intricate latticework of compensatory blood flow.32,33 Most commonly, moyamoya disease presents bilaterally, but unilateral presentations have been reported.34 Affected children most commonly come to medical attention due to stroke or transient ischemic attacks (TIA). Commonly, Moyamoya disease causes acute hemiplegia resulting from uncompensated occlusion of the internal carotid artery. When the condition is present bilaterally, bilateral motor deficits may be found. Both fine motor and extrapyramidal motor function can be adversely affected. It has been found as a sequela to a diverse array of conditions in children including sickle cell disease, neurofibromatosis, postcranial irradiation vasculopathy, Down syndrome, and Williams syndrome. Recently, genetic linkage analyses have revealed associations between Moyamoya disease and loci at 3p24-p26.1, 8q23, and 17q25.3.35 No specific medical therapy has been identified to halt progression of this disorder. However, aspirin has been used to prevent thrombotic events. Importantly, two surgical revascularization techniques have been employed to treat this condition (see below).
Table 552-1. Etiologies of Stroke in Children
Fibromuscular dysplasia may involve multiple sites throughout the systemic arterial tree, most commonly the renal arteries. However, cervicocephalic vasculature comprises the second most common site of this vasculopathy.36 Pathologic or radiologic evidence of fibromuscular dysplasia has been found in carotid, vertebral, and intracranial arteries. Commonly, fibromuscular dysplasia involves irregularly spaced focal zones of dysplastic fibrous tissue in the media muscularis of the arterial wall. These findings can extend to the intima, as well.37 The resulting constricted regions of vascular fibrosis alternate with regions of lumenal dilation to create the characteristic beaded appearance on angiography. Its association with alpha-1-anti-trypsin disease has led to speculation about its possible relationship to other connective tissue disorders. Fibromuscular dysplasia is more common in adult females who range in age from the third decade to middle age, but has been found in adolescent and younger children. Familial occurrence has also been described. If renal arteries are affected, hypertension may be present. Neurologic symptoms signifying cerebrovascular involvement consist of headache, TIA, and stroke. A thrombotic mechanism for stroke has been postulated but has not been proven.
Vasculopathy
Acute hemiplegia due to stroke may occur in children with sickle cell disease. By age 14, up to 11% of children with sickle cell disease will have had clinical stroke and 22% will have had silent cerebral infarction. Low hemoglobin concentration and saturation, high hemoglobin S concentration, and chronically increased cerebral blood flow have all been observed to bear a relationship to the increased occurrence of stroke among children with sickle cell disease.38-41 However, large and middle-sized vessel vasculopathy comprises an important mechanism related to stroke in this patient population. Cerebral vessels can reveal endothelial proliferation, disruption of the elastic lamina, fibrin deposition, and stenosis. Stenosis is found most commonly in the distal internal carotid artery at the site where it bifurcates into the middle cerebral and anterior cerebral arteries.42 The stenoses may be severe in this region producing Moyamoya disease detectable by magnetic resonance imaging (MRI) or catheter angiography (Fig. 552-2).43 Indeed, among children with sickle cell disease, the presence of Moyamoya disease is associated with a twofold increase in the risk of stroke as compared to children undergoing transfusion therapy but who do not have this finding.44
The neurologic signs of stroke in this patient group often consist of hemiparesis, aphasia or visual disturbances. Magnetic resonance imaging studies reveal that clinically evident infarction frequently involves both gray matter and white matter although silent cerebral infarction most commonly involves white matter alone.45 Not only motor but cognitive deficits found among children with sickle cell disease correlate with MRI findings.46 Blood transfusion therapy has proven effective for the prevention of stroke in patients with sickle cell disease. The goal of therapy has become reduction of the hemoglobin S concentration to below 30% with transfusions given roughly monthly. Chronic transfusion therapy imparts increased risk for iron overload. Recently, encouraging results have been obtained with hydroxyurea therapy as an adjunct to transfusion therapy.47-49
A transient form of cerebral vasculopathy unrelated to atherosclerosis has emerged as an important clinical associate of stroke in children. Neurovascular imaging reveals stenoses of the distal internal carotid artery or of the proximal anterior, middle, or posterior cerebral arteries. The arteriopathy is monophasic and reversible. It has been associated with viral pathogens, such as parvovirus, enterovirus, and cytomegalovirus. In addition, mycoplasma pneumoniae and borrelia burgdorferii have been suspected as etiologic agents.50 When neuroimaging prompted by the occurrence of stroke in a child leads to the discovery of such a pattern of mulitfocal stenoses and has been preceded in the previous 12 months by the occurrence of varicella, postvaricella arteriopathy can be contemplated as the cause of the cerebrovascular event.51 The recurrent association of cerebral vasculopathy and stroke with viral infection underscores the importance of these agents in the pathogenesis of stroke in children.
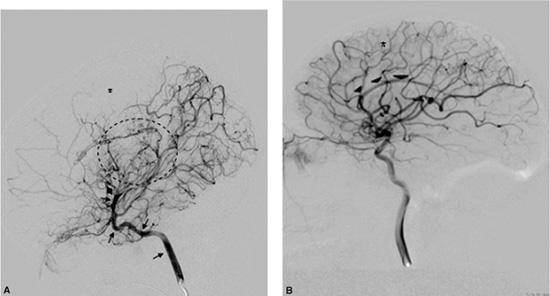
FIGURE 552-2. Moyamoya disease. A: Injection of left internal carotid artery (ICA) on percutaneous cerebral angiogram of a 13-year-old male with sickle cell disease. The ICA (indicated by arrows) ends abruptly at the supraclinoid portion of the artery (marked by arrow and diamond. Note the consequent dearth of middle cerebral artery (MCA) vasculature due to the ICA occlusion (asterisk). While collateral circulation is abundant throughout the brain, especially numerous and tiny vessels are apparent within the circled region indicating intense compensatory vascular proliferation in response to the ICA occlusion. B: Left ICA injection from a normal child in which the full extent of the ICA is evident. A greater extent of vasculature from the MCA (asterisk) and anterior cerebral artery (arrowheads) territories is evident but is not found in (A).
Cervical vessel injury caused by head, neck, or intraoral trauma may cause stroke. Neurologic symptoms may be delayed more that 24 hours relative to the time of inciting trauma. Stroke due to carotid artery injury has been well documented. A typical presentation follows intraoral trauma to the internal carotid artery in a toddler who falls with a pencil or other object in the mouth. In older children, these cerebrovascular events occur after head/neck trauma sustained during motor vehicle or bicycle accidents, or following fights or falls. Conventional angiography may reveal internal carotid artery occlusion. Neuropathologic findings vary from an intimal tear with resulting thrombus formation leading, to arterial occlusion or frank arterial dissection. Vertebral artery injury may also lead to stroke in the posterior circulation of the brain. The serpentine course of the vertebral arteries through the cervical spine imparts vulnerability to traction injury. Thus, neurologic signs referable to brainstem, cerebellar, thalamic, temporal, or occipital lesions should lead to consideration of a vertebrobasilar etiology of stroke. Indeed, spontaneous arterial dissection of vessels in the anterior and posterior cerebral circulations have been reported in children.52-55 Finally, cranial radiation therapy, received as part of cancer therapy, may induce an occlusive vasculopathy leading to focal cerebral ischemia.56,57
Vasculitis
Bacterial infection constitutes an important and treatable cause of stroke in children. Inflammation of cerebral arteries and veins may occur in the course of bacterial meningitis. The subarachnoid arteries become immersed in purulent exudate and smaller vessels are affected as exudate moves down the Virchow-Robin spaces. Autopsy studies have revealed white cell invasion beneath the arterial intima; focal necrosis and mural thrombi have been observed in veins.58 Stroke may occur due to occlusion of either arteries or veins. Antibiotic treatment early in the course of the infection forms the cornerstone of therapy. Viral infections may promote vascular inflammation that may involve the cerebral vessels and culminate in stroke (see above). Indeed, cerebral vasculitis and stroke have been described in association with HIV infection in children.
Autoimmune disorders can include vasculitis that may involve the central nervous system (Table 552-2). Cerebrovascular involvement is well documented. Central nervous system symptoms of abrupt onset have long been associated with systemic lupus erythematosus (SLE). A CNS vasculitis had been presumed to underlie the brain cerebrovascular manifestations of SLE. However, autopsy study of patients suffering from SLE revealed a virtual absence of cerebrovascular inflammation. Rather, small areas of infarction relate to proliferative changes in cerebral arterioles leading to luminal occlusion.59 Large areas of infarction are sometimes found and may be related to anitphospholipid antibody related thromboembolism or to lupus-related embolism from sterile cardiac leaflet vegetations associated with SLE.60
Table 552-2. Autoimmune Disorders Associated with Central Nervous System (CNS) Involvement
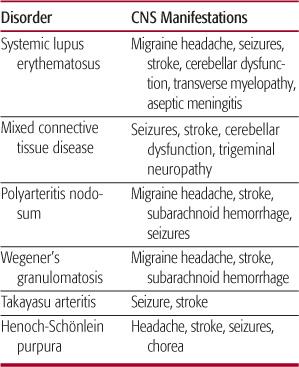
Stroke may occur in the course of polyarteritis nodosa. Involvement of the CNS is found in 20% to 40% of patients.61,62 Mixed connective tissue disease (MCTD), which clinically overlaps with polymyositis, SLE, and progressive systemic sclerosis, can involve the CNS. Cranial neuropathy, most commonly trigeminal nerve dysfunction has been the most frequently cited deficit. However, stroke has been reported in children afflicted with MCTD.63 Necrotizing arteritis with inflammatory infiltrate has been found in both meningeal and cerebral vessels of children suffering from Henoch-Schoenlein purpura. Both fixed and transient central neurologic deficits may occur in this disorder. Treatment with steroid or with other immunosuppressive agents may prove helpful. Long-term anticoagulation has not been studied. Neurologic complications have been reported to accompany Kawasaki disease. Hemiplegia and neuroimaging findings indicative of focal cerebral infarction have been observed.64-66 Takayasu arteritis involving the aorta and its principal branches has been associated with thrombotic stroke. Inflammation-induced luminal constriction leading to thrombosis is thought to cause cerebral ischemia in these children. Angiographic improvement of vessels in the carotid tree has been observed following immunosuppressive therapy. The central nervous system may be involved in children with hemolytic-uremic syndrome (HUS). Stroke accompanied by radiographic evidence of focal CNS injury has been observed in 5% of children with HUS. Focal infarction is found primarily in cerebral hemisphere and basal ganglia. Damage to endothelial vascular lining due to Shiga toxin produced by Escherichia coli O157:H7 is thought to activate platelets and coagulation cascades to culminate in thromboembolic stroke.67,68
Vasospasm
Stroke may occur in the setting of migraine headache. The occurrence of focal deficits during migraine headache denotes a complicated migraine and is believed to reflect the involvement of either the carotid or vertebrobasilar circulation. Symptoms may include hemiparesis, ataxia, cortical blindness, and cranial nerve dysfunction and may be either fixed or transient. Angiographic studies have been performed on patients suffering focal deficits consistent with stroke in the setting of migraine headache. Vasoconstriction of vessels in either the vertebrobasilar or carotid circulations has been documented. In these cases, the neuroan-atomic position of the constricted vessels correlated with the location of the observed deficits. As a result, ischemia provoked by vasoconstriction during prolonged migraine has been hypothesized as a mechanism of stroke in these patients.
Drug abuse may promote thrombotic stroke. Cerebral infarction and peripheral neuropathy have been associated with glue sniffing in children. Cerebral infarction and subarachnoid hemorrhage have both been observed in association with cocaine use. Cocaine blocks the reup-take of catecholamines at the synaptic cleft. As a result of elevated synaptic concentration of epinephrine and norepinephrine, the neural activity of adrenergic systems is markedly enhanced. Tachycardia, hypertension, and vasoconstriction result. The probability of subarachnoid hemorrhage is higher in cocaine users with occult intracranial vascular abnormalities than in those with normal cerebral vasculature. The resultant sudden rise in systemic blood pressure is thought to precipitate subarachnoid hemorrhage. Ischemic lesions have also been found in patients who have used cocaine or who have been exposed to it prenatally. The physiologic evidence favors vasoconstriction as the underlying etiology of ischemic stroke found after cocaine use.69
Hematologic Etiologies
Several disorders of coagulation have been associated with embolic or thrombotic stroke. Adverse consequences of antiphospholipid antibodies including the lupus anticoagulant (LAC) and anticardiolipin antibody (aCL) have been identified in all age groups. However, cerebrovascular consequences of these antibodies are found in children, adolescents, and young adults. Antiphospholipid antibodies are polyclonal antibodies in serum which can bind to both neutral and negatively charged phospholipids. Recently, antibodies to beta-2-glycoprotein-1, a plasma cofactor that facilitates the binding of anticardiolipin antibodies to phospholipid, has also been demonstrated to be elevated in young children with cerebral thrombosis.70-72 Antiphospholipid antibodies prolong the partial thromboplastin time (PTT) in vitro, but act as a procoagulant in vivo. In addition to a prolonged PTT, its presence is indicated by a falsely positive serum Venereal Disease Research Laboratory (VDRL) test result and can be confirmed by functional and immunologic tests for antiphospholipid antibodies. Its presence has been associated with up to a six-fold increase in risk of stroke in children.73 Further, transplacental passage of the antibody from mother to infant has been invoked as a cause of presumed prenatal, perinatal, and neonatal stroke.74
Absence of specific serum proteins that act as inhibitors of coagulation may lead to stroke in children. Deficiencies of protein S and protein C have been associated with thrombotic or embolic cerebrovascular disease in the young. Protein C and its cofactor protein S act as anticoagulants and synergistically attenuate coagulation by deactivating the thrombin-activated forms of factors V and VIII. Absence of either of these proteins may tip the scale of balanced coagulation toward increased spontaneous clotting and can result in stroke. Anti-thrombin-III inhibits serine esterase activity and opposes not only the action of thrombin but also the activated forms of II, IX, X, XI, and XII. Deficiencies of protein S or C or of antithrombin-III may cause arterial thrombotic or embolic stroke or venous infarction.14,75,76 Although these deficiencies are often congenital, they may be acquired through liver disease (reduced synthesis), inflammatory bowel disease, or nephritic syndrome (protein wasting).77 Screening tests, including prothrombin time (PT), partial thromboplastin time (PTT), and specific immunologic and functional testing of the proteins suspected of being deficient are essential for diagnosis.
Elevation of lipoprotein (a) represents a recently identified characteristic that has been suggested as a risk factor for stroke in both neonates and older children. Lipoprotein (a) is a low-density lipoprotein with apolipoprotein (a) as a substituent. Bearing regions of homology very similar to the fibrin binding sites of plasminogen, lipoprotein (a) appears to compete with plasminogen and thereby contributes to a procoaguable state. It has been associated with stroke in neonates and in older children.78-80
Cancer and its treatment may predispose children to cerebrovascular ischemic events. Promyelocytic leukemia and its treatment have been observed to provoke disseminated intravascular coagulation leading to stroke. Lymphoreticular cancers, more than solid tumors, have been linked to thrombotic and embolic strokes. Transient ischemic attacks (TIAs) following induction chemotherapy for acute lymphoblastic leukemia have been reported. In addition, dural sinus and cerebral sinovenous thrombosis (CSVT) have been found after therapy with L-asparaginase.81
Oral contraceptives continue to engender concern as a risk factor for stroke among young women, especially those with migraine. Migraine in young women is associated with increased risk for ischemic stroke. This risk is higher in migraine with aura and is further increased by tobacco smoking and use of oral contraceptives. As a result, among young women who are prescribed oral contraceptives, abstinence from tobacco use and use of low-estrogen-content oral contraceptive pills, or those with progestogens only, has been advised.82 Pregnancy and the post partum state have been considered periods of hypercoaguability. In addition, venous stasis increases. These two factors are believed to promote the occurrence of cerebral venous thrombosis and cerebral infarction, often venous in nature, in pregnant and immediately postpartum females. Frequently, the initial manifestation is headache. Seizures, either focal or generalized, are common. Acute hemiparesis is the most common focal finding on the neurologic examination. Papilledema can appear as a consequence of increased intracranial pressure resulting from obstruction of cerebral venous outflow. The appearance of these signs or symptoms in a gravid or postpartum adolescent should raise suspicion about the existence of the underlying cerebral venous thrombosis. Finally, insect stings have caused focal cerebral infarction in children. Wasp and scorpion venom activate platelets, promoting thrombogenesis, which can culminate in focal infarction.
Genetic and Metabolic Etiologies
Table 552-3 provides a summary of the genetic and metabolic causes of stroke. Three genetic mutations have been found to lead to protein dysfunction that has been associated with prothrombotic features that may culminate in stroke. These are the factor V Leiden mutation (FVL), the prothrombin 20210 mutation, and deficiency of methylene tetrahydofolate reductase (MTHFR). The factor V Leiden mutation, due to a single nucleotide G→A transition in exon 10 of the factor V gene, results in replacement of arginine by glutamine at amino acid 506 in the protein. This substitution imparts striking resistance of the factor to inactivation by protein C and consequently abnormally sustained ability to advance coagulation. It accounts for greater than 95% of activated protein C resistance. Neonatal stroke and stroke in older children has been associated with this mutation.83,84
The prothrombin 20210 (PTG20210A) mutation, like the FVL mutation, involves a G→A transition and occurs at nucleotide 20210 in the prothrombin gene. Although this occurs in the terminal untranslated portion of the gene, it nonetheless imparts an increased level of activity to the prothrombin protein. The prothrombin 20210 mutation has been associated with childhood and neonatal stroke.78,79,85 In addition, it has been associated with recurrence of stroke in children.86
Genetically determined dysfunction of cystathionine reductase is widely recognized for consequent elevation of serum homocysteine level (see below). However, the level of this amino acid can become abnormally high by other means. The enzyme 5,10-methylenetetrahydrofolate reductase (MTHFR) catalyzes the regeneration of fully reduced methyl tetrahydrofolate, the major circulating form of folate. Folate participates in the remethylation of homocysteine to methionine. A mutation at the 677 position of the MTHFR gene causes an alanine to valine substitution in the resulting protein and impairs enzyme function that results in elevated plasma homocysteine levels in the setting of folate deficiency. Although increased risk for childhood stroke has been associated with both homozygosity and heterozygosity for this mutation, it remains unclear whether this increased risk relates to elevation of the homo-cysteine level or to some other consequence of the genetic mutation itself.87-92
Table 552-3. Genetic and Metabolic Causes of Stroke



