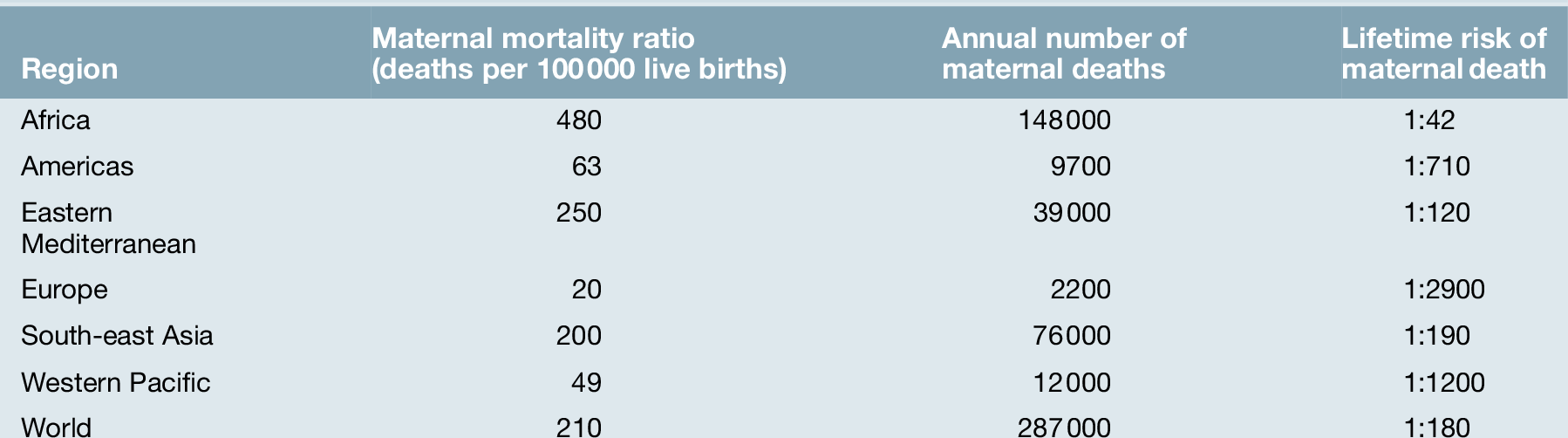
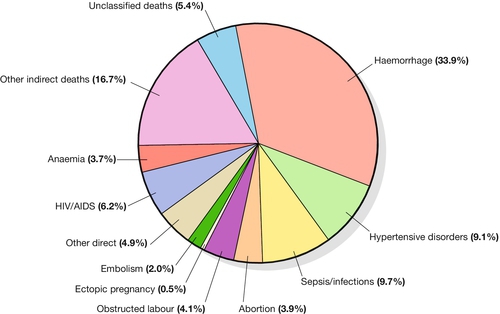
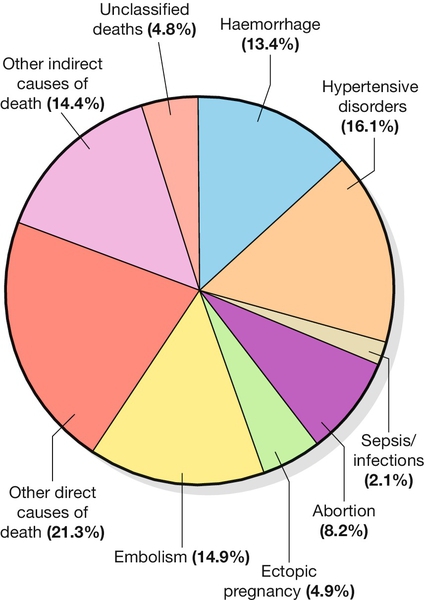
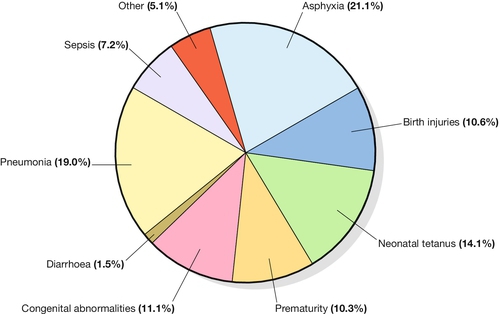
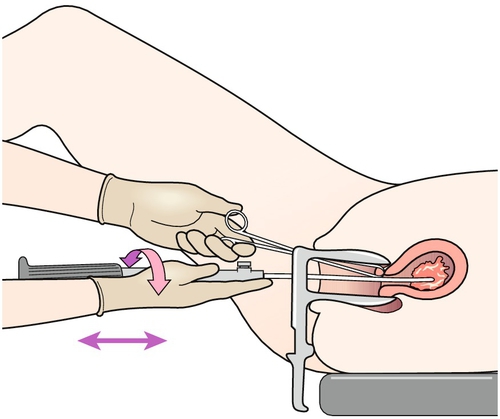
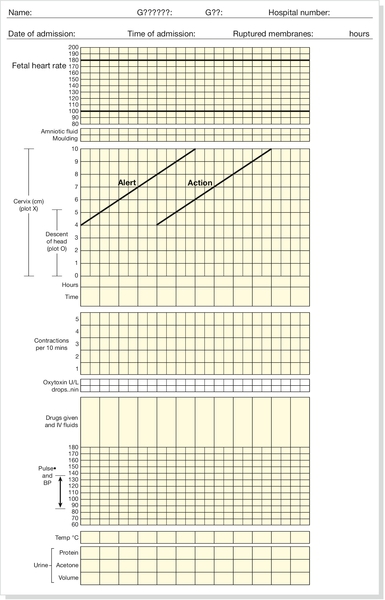
29 Estimates of global maternal and neonatal mortality Obstetric causes of maternal mortality Medical conditions contributing to maternal mortality and morbidity Strategies to improve global maternal and newborn health It is estimated that almost 300 000 women worldwide die each year from the complications of pregnancy and childbirth, with 99% of these occurring in developing countries. Estimates from 2010 by the World Health Organization (WHO) and other partners, show that just over half of all maternal deaths occur in sub-Saharan Africa alone and about one-third of all maternal deaths occur in South Asia. For every woman who dies, around 20 women have serious ill-health and lifelong disability as a result of these same complications. Eight Millennium Development Goals (MDGs) were adopted in 2000 following the Millennium Summit, two of which are directly related to maternal and newborn health: MDG 4 to reduce child mortality, and MDG 5, which sets a target of reducing maternal mortality by 75% between 1990 and 2015. Although the latest estimates of maternal deaths published in 2011 suggest a decline in maternal mortality since 1990, there is lack of progress in a number of developing countries especially in sub-Saharan Africa and South-east Asia (Table 29.1). At least 80% of all maternal deaths globally result from five complications that are well understood and can be readily treated: haemorrhage, sepsis, eclampsia, complications of obstructed labour and abortion. This is in contrast to cause of death in more developed countries where maternal deaths are more likely to be due to indirect causes (Figs 29.1 and 29.2). In addition to this high number of maternal deaths, an estimated 4 million neonatal deaths and 3 million stillbirths occur each year. Neonatal deaths account for at least 40% of all deaths of children under 5 years of age. MDG 4 is to reduce the under-5 mortality rate by two-thirds between 1990 and 2015. Progress on reducing child mortality has also been substantially slower than the annual target rate of decline for children, although more progress has been made compared to maternal mortality. The health of the neonate is closely related to that of the mother, and the majority of deaths in the first month of life could also be prevented if interventions were in place to ensure good maternal health (Fig. 29.3). Birth injuries, birth asphyxia and most neonatal tetanus could be prevented with skilled professional care at the time of the delivery as well as in antenatal and postnatal periods. Similarly, many cases of sepsis in the neonate are directly linked to the health of the mother and/or the care she received during childbirth. It is estimated that one-third of all stillbirths occur during labour and delivery. The five main causes of direct obstetric maternal mortality are discussed here. Many maternal deaths in resource-poor areas are caused by or associated with haemorrhage. This may be because of antepartum bleeding (e.g. abruption of the placenta), bleeding during delivery (e.g. with a ruptured uterus or placenta praevia) or postpartum (e.g. from an atonic uterus or retained placenta). The risk of dying from haemorrhage is higher if women are already anaemic in pregnancy (Hb < 11.0 g/dL). Oxytocics are very effective in preventing postpartum haemorrhage (active management of the third stage), as well as in treating uterine atony, but oxytocics may not be routinely used and/or available. Manual removal of a retained placenta can be carried out by trained midwives and doctors using simple general anaesthesia (e.g. with IM ketamine). The ability to give intravenous fluids, safe blood transfusion and anaesthesia is extremely important when pregnancy or delivery is complicated by haemorrhage. It is estimated that non-availability of blood for transfusion accounts for about a quarter of deaths associated with haemorrhage. Most cases of maternal death associated with obstructed labour (see also Chapter 44) are attributable to rupture of the uterus (Fig. 29.4). Persistent malposition, e.g. transverse lie which if unrecognized and allowed to progress is also a cause of rupture of the uterus (Fig. 29.5). The correct use of a simple partogram, with an ‘action line’ to prompt a response if labour does not progress normally, has been shown to be very helpful in making a timely diagnosis of cephalo-pelvic disproportion or simple failure to progress (Fig. 29.6). Fig. 29.6WHO modified partogram. The ‘alert’ and ‘action’ lines can be used to prompt referral or intervention if delay in progress of labour is apparent. In many cases of obstructed labour, women are referred to a health facility late. The presenting part may be deeply impacted in the pelvis and a vaginal examination may demonstrate oedema and overlapping of the fetal skull bones. The mother will be dehydrated, exhausted, in severe pain from a tonically contracted uterus or pyrexial as a result of infection and/or sepsis. If the uterus has ruptured, the fetal heartbeat is usually absent and the fetal parts can usually be palpated easily abdominally. In addition, the woman may be in shock as a result of bleeding or sepsis. Bleeding during delivery should always be a cause for alarm if cephalo-pelvic disproportion is suspected. A woman with cephalo-pelvic disproportion in labour may also have a Bandl’s ring. This is a visible constriction seen in the abdominal contour, which is a warning sign of impending rupture of the uterus. If the presenting part has been impacted in the pelvis for many hours, pressure necrosis of the genital tract, as it is compressed between the baby’s head and the bony pelvis, may lead to obstetric fistulae. Vesicovaginal fistulae are the most common, but rectovaginal and ureterovaginal fistulae also occur. Such fistulae may also occur after difficult obstetric abdominal surgery. Women who suffer from fistulae often have no living child, they become outcasts from their society, and may live in poverty. Very many women with fistulae are unable to access suitable care. In order to try to prevent fistulae, or to encourage small fistulae to close spontaneously, it is important that all women who have survived prolonged or obstructed labour (with or without a caesarean section) should be treated initially by continuous bladder drainage and preferably with antibiotics to minimize the risk of urinary tract infection. Spontaneous closure can occur within 6–8 weeks with such conservative management, but most fistulae do not heal spontaneously and require specialized surgical management. Such surgery requires considerable expertise and specialists (obstetrician–gynaecologists and urologists) will need to seek additional training to be able to offer a good surgical repair. Equally important is the provision of good nursing care, physiotherapy and steps towards rehabilitation and reintegration into society for women who have suffered fistulae. Sepsis following prolonged membrane rupture or retained products of conception (incomplete miscarriage or unsafe abortion) may lead to overwhelming septic shock, multisystem failure and death. Early recognition and prompt commencement of antibiotic treatment is important. If there are retained products of conception, manual vacuum aspiration (MVA) of retained products of conception can be life-saving (Fig. 29.7). This has, in many countries, replaced the traditional technique of dilatation and curettage (D&C), which requires general anaesthesia. Using good technique, MVA can be performed in early pregnancy under local anaesthesia. Unrecognized rupture of the membranes during pregnancy risks ascending infection and this can lead to chorioamnionitis, premature delivery and major systemic sepsis if not recognized and treated during the antenatal period. Prophylactic antibiotics must always be given after prolonged membrane rupture as well as at the time of a CS.
Strategies to improve global maternal and neonatal health
Estimates of global maternal and neonatal mortality
Obstetric causes of maternal mortality
Haemorrhage
Obstructed labour
Sepsis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree