Faigenbaum AD et al: Youth resistance training: updated position statement paper from the national strength and conditioning association. J Strength Cond Res 2009;23(Suppl):S60–S79 [PMID: 19620931].
Myer GD et al: When to initiate integrative neuromuscular training to reduce sports-related injuries and enhance health in youth? Curr Sports Med Rep 2011;10(3):155–166 [PMID: 21623307].
FITNESS & CONDITIONING
Compared to children who are sedentary, physically active youth tend to develop greater agility and skills and maintain better fitness throughout their lifetime. Young children and adolescents should participate in physical activity for 60 minutes or more each day. To improve overall fitness and reduce the risk of injury, children and adolescents should focus on three different components of exercise:
1. Resistance (strength) training (progressive resistive loads in a variety of modalities).
2. Neuromuscular conditioning (mixture of basic fundamental and specialized motor control exercises aimed at improving general health and sports performance). Examples include core strength exercises, agility, and plyometrics.
3. Integrative training (curriculum of diverse skills, increasing fitness, and appropriate rest periods). Examples include developing fundamental skills and technique, learning proper movement mechanics, aerobic and anaerobic conditioning.
Periodization is a training concept that emphasizes variations in the volume and intensity of training throughout the year in a conditioning program. Continuously varying the specific type and goals of training provides adequate recovery from each strenuous exercise session and avoids overtraining, burnout, and overuse injuries.
Myer GD et al: When to initiate integrative neuromuscular training to reduce sports-related injuries and enhance health in youth? Curr Sports Med Rep 2011;10(3):155–166 [PMID: 21623307].
SPORTS NUTRITION
Proper nutrition in young athletes focuses on maintaining an appropriate energy balance; creating healthy eating and hydration habits; and avoiding harmful food, drink, and supplement choices. Keeping an adequate nutritional intake will increase lean muscle mass, maximizing strength, endurance, immunity, and training benefit. Athletes should be encouraged to balance caloric intake with energy expenditure, eat whole grains, avoid processed foods, focus on healthy fats and proteins, and maintain proper hydration. Carbohydrates should compose 55%–60% of a young athlete’s diet, with fat and protein making up 25%–30% and 12%–15%, respectively. Hydration can come mainly from water if the exercise lasts less than 1 hour, after which time a carbohydrate-containing sports drink is appropriate. Water or sports drinks should be consumed every 15–20 minutes during prolonged exercise greater than 1 hour or in hot playing conditions. A light snack and hydration are recommended prior to and immediately after an extended workout. To avoid excessive caloric and sugar intake, sports drinks are not recommended at meals or times other than prolonged exercise. The average athlete eats a well-balanced diet not necessitating nutritional supplementation. However, if food allergies or improper dietary intake is confirmed, an athlete may benefit from a daily multivitamin. In general, nutritional sports supplements are not recommended and extreme caution is suggested when considering their use. The supplement industry is not well-regulated and contamination with toxic and banned substances has been noted in the past. Similarly, energy drinks are not recommended for use in any youth under the age of 18 years due to high levels of caffeine and other stimulants contained in such beverages.
ACSM, ADA, DOC: Nutrition and athletic performance. Med Sci Sports Exerc 2009;709–731 [PMID: 11128862].
Committee on Nutrition and Council on Sports Medicine and Fitness: Sports drinks and energy drinks for children and adolescents: are they appropriate? Pediatrics 2011;127(6): 1182–1189 [PMID: 21624882].
Kleinman R (ed): Pediatric Nutrition Handbook, 6th ed. AAP; 2009.
PREPARTICIPATION PHYSICAL EVALUATION
The ultimate goal of the preparticipation physical evaluation (PPE) is to promote the health and safety of athletes. Its primary objectives are to screen for conditions that may be life threatening or disabling and for conditions that may predispose to injury or illness. Secondary objectives of the PPE include establishing a medical home, determining the general health of the individual, assessing fitness for specific sports, and counseling on injury prevention and health- related issues. The ideal timing of the examination is at least 6–8 weeks before training starts. This allows time to further evaluate, treat, or rehabilitate any identified problems.
Preparticipation History
The medical history is the most important part of the encounter, identifying 65%–77% of medical and musculoskeletal conditions. Therefore, obtaining a thorough and accurate history is essential in identifying conditions that may affect a child’s ability to safely participate in sports. Many key elements should be explored with the athlete. A standardized PPE form, endorsed by six medical societies including the American Academy of Pediatrics (AAP), is available in the fourth edition of the PPE monograph (Bernhardt and Roberts 2010) or on the Internet. This monograph, formulated based on current literature, policies, consensus statements, expert opinion, and extensive peer review, is currently the recommended standard for the preparticipation physical examination in the United States. Figure 27–1A and B contain copies of the PPE form. The history includes the following areas:
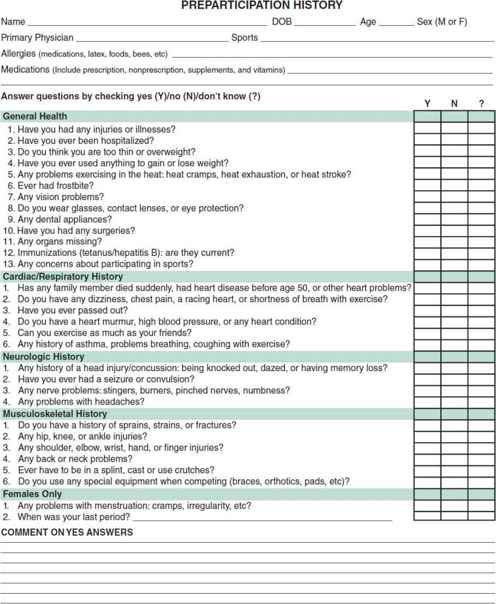
 Figure 27–1. A: Preparticipation Physical Evaluation form.
Figure 27–1. A: Preparticipation Physical Evaluation form.
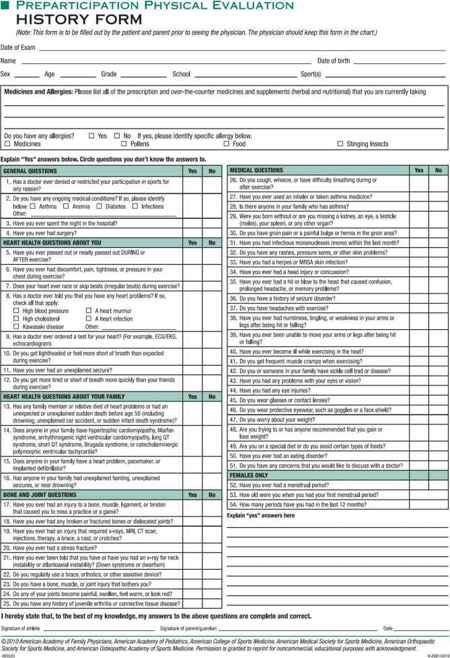
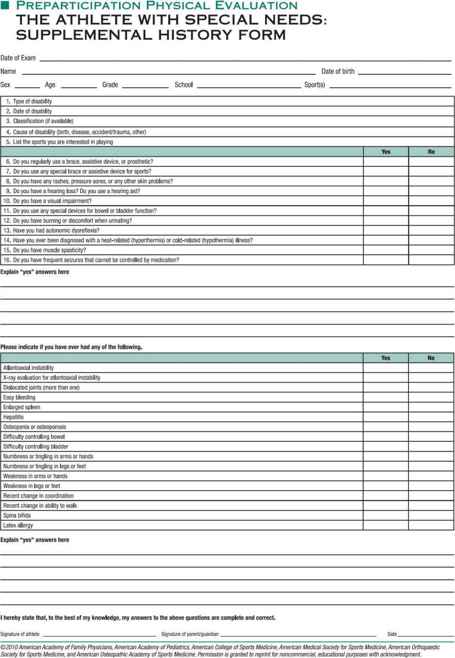
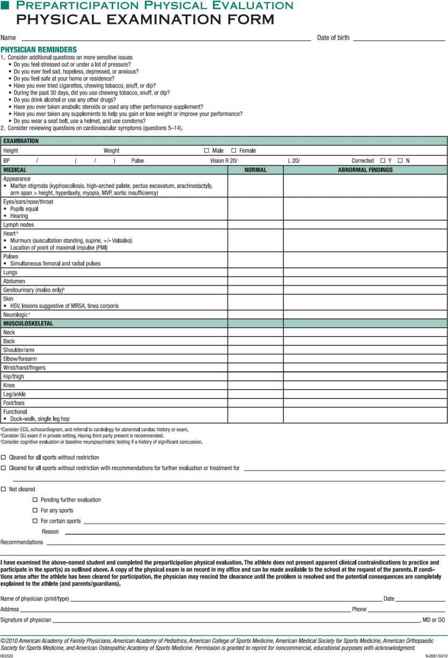
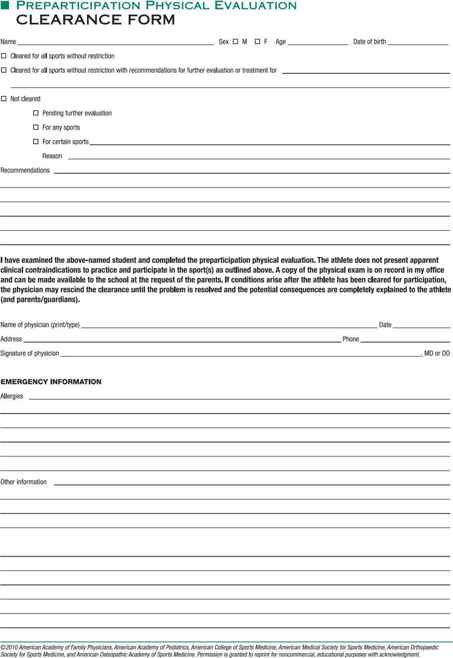
 Figure 27–1. B: Preparticipation examination.
Figure 27–1. B: Preparticipation examination.
A. Cardiovascular History
The routine use of electrocardiogram (ECG) and echocardiography in the preparticipation cardiovascular screening in athletes remains a highly debated topic in sports medicine and sports cardiology. Despite ongoing controversy, the American Heart Association (AHA) currently recommends against its routine usage in asymptomatic athletes because of its low sensitivity, high false-positive rate, limited resources, lack of trained physicians to interpret the ECG, and poor cost-effectiveness due to the low prevalence of disease. In 2007, the AHA updated its consensus statement on cardiovascular screening stating its position to this effect. According to the AHA, the goal of the PPE is to reduce cardiovascular risk associated with physical activity. The 2007 AHA recommendations for cardiovascular screening are incorporated in the fourth edition PPE monograph and include the following 12-point screen:
Personal Medical History:
1. Chest pain or discomfort with exercise
2. Syncope or near syncope associated with exercise
3. Excessive shortness or breath or fatigue associated with exertion
4. History of heart murmur
5. History of elevated blood pressure
Family Medical History:
6. Premature death before age 50 years due to heart disease
7. Disability from heart disease in a close relative younger than 50 years
8. Knowledge of specific cardiac conditions: hypertrophic or dilated cardiomyopathy, long QT syndrome, other ion channelopathies, Marfan syndrome, or arrhythmias
Physical Examination:
9. Auscultation of heart murmur in supine and standing position
10. Palpation of radial and femoral pulses
11. Physical stigmata of Marfan syndrome
12. Brachial blood pressure taken in seated position
Sudden cardiac arrest is the leading cause of death in young athletes, accounting for 75% of all sudden deaths. Addressing these areas may help identify potentially life-threatening cardiac lesions. However, clinicians should keep in mind that there are currently no outcome-based studies that demonstrate the effectiveness of the PPE in preventing sudden cardiac death in athletes. In the United States, the most common causes of sudden cardiac death on the playing field are hypertrophic cardiomyopathy (HCM) and congenital coronary artery anomalies, with HCM accounting for one-third of sudden cardiac deaths in young athletes. Any athletes with cardiovascular symptoms require further evaluation before allowing them to participate in sports. Any activity restrictions or sports disqualification for an athlete should be made in consultation with a cardiologist.
B. History of Hypertension
Any history of hypertension requires investigation for secondary causes of hypertension and target organ disease. An athlete with hypertension who exercises may cause their blood pressure to rise even higher, placing them at increased risk for complications. Athletes should also be asked about the use of stimulants (ie, caffeine, nicotine) and a family history of hypertension. The diagnosis of hypertension in children younger than 18 years is based on gender, age, and height, and the blood pressure must be measured on three separate occasions. Blood pressure measurements with values from 90% to 95% of gender, age, and height-based norms are considered prehypertension; values from 95% to 5 mm Hg above the 99% of norms are defined as stage 1 hypertension; and values greater than 5 mm Hg above the 99% of norms are defined as stage 2 hypertension.
Athletes with prehypertension are eligible to participate in sports. Counseling regarding lifestyle modifications should be made, including healthy dietary changes, weight management and daily physical activity. Those with stage 1 hypertension, in the absence of end-organ damage, may also participate in competitive sports but with appropriate subspecialist referral if the individual is symptomatic, have associated heart disease or structural abnormality, or have persistent elevated blood pressure on two additional occasions despite lifestyle modifications. Athletes who have stage 2 hypertension or end-organ damage should not be cleared to participate in competitive sports until their blood pressure is evaluated, treated, and is under control.
C. Central Nervous System
A history of frequent or exertional headaches, seizure disorders, concussion or head injuries, recurrent stingers or burners, or cervical cord neuropraxia may affect an athlete’s ability to participate in sports. These conditions require further evaluation, rehabilitation, or informed decision-making prior to clearance for sports participation. The fourth edition PPE monograph provides an updated review and recommendations on concussions in sports. (See also section Concussion.)
D. History of Chronic Diseases
Diseases such as reactive airway disease, exercise-induced asthma, diabetes, renal disease, liver disease, chronic infections, or hematologic diseases should be noted.
E. Surgical History
Surgical history may influence participation in certain sports. Full recovery with no long-term impact on athletic performance is required prior to clearance.
F. Infectious Mononucleosis
Ask about infectious mononucleosis in the last 4 weeks. The risk for splenic rupture is highest within the first 3 weeks of illness and can occur in the absence of trauma. Therefore, physical activity should be avoided during the first 3–4 weeks after the infection starts. The athlete may return to play once clinical symptoms are resolved and risk for splenic rupture is assessed as minimal. The use of serial abdominal ultrasound to assess spleen size to aid in return to play decisions is debatable. Parameters for spleen size based on ethnicity, sex, height, and weight have not yet been established so determining when spleen size has normalized based on imaging becomes difficult.
G. Musculoskeletal Limitations and Prior Injuries
The physician should inquire about joints with limited range of motion, muscle weakness, and prior injuries that may affect future performance. Chronic pain or soreness long after activity may reflect overuse syndromes that should be evaluated.
H. Menstrual History in Females
The physician should pay particular attention to the so-called female athlete triad: amenorrhea disordered eating and osteoporosis.
I. Nutritional Issues
The physician should record methods the athlete uses to maintain, gain, or lose weight. Eating disorders or inadequate nutritional intake could lead to persistent or recurrent injury, including stress fractures. Vitamin D deficiency has become increasingly common in female athletes due to inadequate dietary intake or decreased sunlight exposure.
J. Medication History
Inquire about the use of prescription, over-the-counter medications, and supplements. Not only will medications reveal problems omitted in the medical history, but the information will also provide data on current medications whose side effects may suggest activity modifications. Documenting drug use may provide the opportunity to explore with the patient the drawbacks of performance-enhancing compounds such as anabolic steroids, creatine, stimulants, and narcotics.
Armsey TD, Hosey RG: Medical aspects of sports: epidemiology of injuries, preparticipation examination and drugs in sports. Clin Sports Med 2004;23:255 [PMID: 15183571].
Bernhardt DT, Roberts WO: Preparticipation Physical Evaluation, 4th ed. American Academy of Pediatrics; 2010.
Burrows M et al: The components of the female athlete triad do not identify all physically active females at risk. J Sports Sci 2007;25:12 [PMID: 17786682].
McCambridge TM et al: Council on Sports Medicine and Fitness: Policy Statement—athletic participation by children and adolescents who have systemic hypertension. American Academy of Pediatrics. Pediatrics 2010 Jun;125(6):1287–1294 [PMID: 20513738].
Maron BJ., Doerer JJ., Haas TS., et al: Profile and frequency of sudden death in 1463 young competitive athletes: from a 25 year U.S. national registry: 1980-2005. Circulation 2006; 114(Suppl II): 830.
Maron BJ et al: Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation 2007;115(12):1643–1655. [PMID: 17353433].
National Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents: The fourth report on the diagnosis, evaluation and treatment of high blood pressure in children and adults. Pediatrics 2004;114:555–576 [PMID: 15286277].
Putukian M, O’Connor FG, Stricker P: Mononucleosis and athletic participation: An evidence-based subject review. Clin J Sport Med 2008;18(4):309–315 [PMID: 18614881].
Seto C: The preparticipation physical examination: an update. Clin Sports Med 2011;30:491–501 [PMID: 21658544].
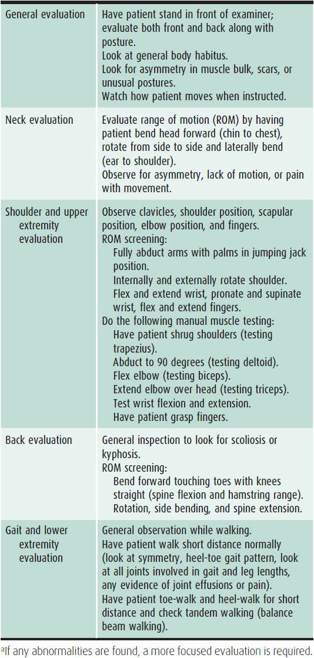
Physical Examination
The physical examination should be focused on the needs of the athlete. It may be the only time an athlete has contact with medical personnel and can be used to promote wellness along with screening for physical activity. Figure 27–1B is an example of a preparticipation physical examination form endorsed in the fourth edition of the PPE monograph (Bernhardt and Roberts 2010). The examination should include routine vital signs, including blood pressure measurements obtained in the upper extremity. The cardiovascular examination should include palpation of pulses, auscultation for murmurs while sitting and standing, evaluation for physical stigmata of Marfan syndrome, and assessment of any cardiovascular symptoms as previously described. The musculoskeletal examination is used to determine strength, range of motion, flexibility, and previous injuries. Included is a quick guide that can be used to screen for musculoskeletal abnormalities (Table 27–1). The remainder of the examination should emphasize the following areas:
Table 27–1. The screening sports examination.a
A. Skin
Are there any contagious lesions such as herpes or impetigo?
B. Vision
Are there any visual problems? Is there any evidence of retinal problems? Are both eyes intact?
C. Abdomen
Is there any evidence of hepatosplenomegaly?
D. Genitourinary System
Are any testicular abnormalities or hernias present?
E. Neurologic System
Are there any problems with coordination, gait, or mental processing?
F. Sexual Maturity
What is the individual’s Tanner stage?
Recommendations for Participation
After completing the medical evaluation, the physician can make recommendations about sports clearance. The options include the following:
• Cleared for all sports without restrictions
• Cleared for all sports without restrictions with recommendations for further evaluation or treatment
• Not cleared: pending further evaluation, for any sports, or for certain sports
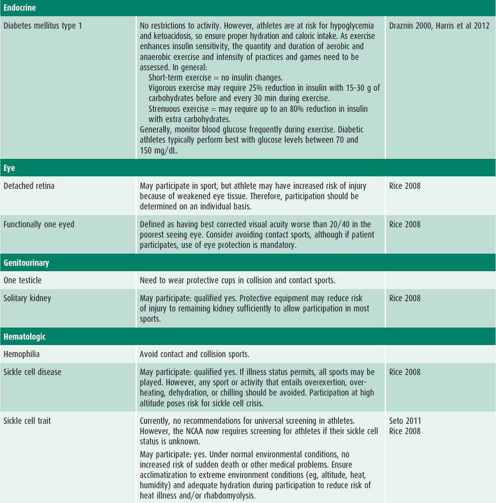
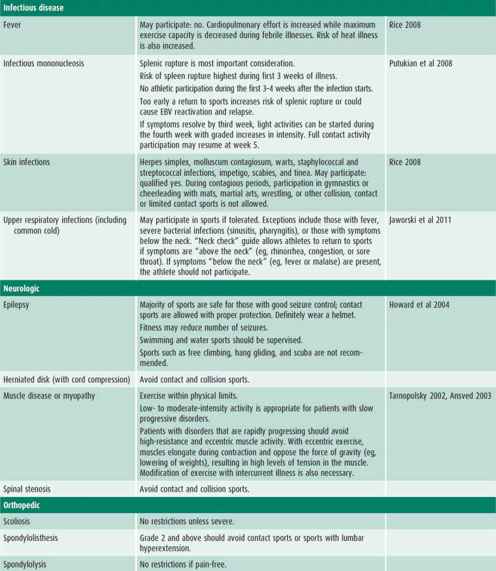
Table 27–2 is a composite of recommendations for sports participation organized by body system. Recommendations for sports participation with specific medical conditions can be found on the AAP website.
Table 27–2. Recommendations and considerations for participation in sports.


Anderson BR, Vetter VL: Return to play? Practical considerations for young athletes with cardiovascular disease. Br J Sports Med 2009;43:690 [PMID: 19734504].
Ansved T: Muscular dystrophies: influence of physical conditioning on the disease evolution. Curr Opin Clin Nutr Metab Care 2003;6:435 [PMID: 12806128].
Bernhardt DT, Roberts WO: Preparticipation Physical Evaluation, 4th ed. American Academy of Pediatrics; 2010.
Braith RW: Exercise for those with chronic heart failure. Phys Sportsmed 2002;31:29 [PMID: 20086544].
Draznin MB: Type 1 diabetes and sports participation: strategies for training and competing safely. Phys Sportsmed 2000;28:49 [PMID: 20086616].
Firoozi S et al: Risk of competitive sport in young athletes with heart disease. Heart 2003;89:710 [PMID: 12807837].
Harris G et al: Diabetes in the competitive athlete. Curr Sports Med Rep 2012 Nov/Dec; 11(6):309–315 [PMID: 23147019].
Howard GM et al: Epilepsy and sports participation. Curr Sports Med Rep 2004;3:15 [PMID: 14728909].
Hull J et al: Managing respiratory problems in athletes. Clin Med 2012;12(4):351–356 [PMID: 22930882].
Jaworski C et al: Infectious disease. Clin Sports Med 2011; 30: 575–590 [PMID: 21658549].
Maron BJ et al: Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism. Circulation 2007;115:1643–1655 [PMID: 17353433].
Maron BJ: Hypertrophic cardiomyopathy: Practical steps for preventing sudden death. Phys Sportsmed 2002a;30:19 [PMID: 11984027].
Maron BJ: The young competitive athlete with cardiovascular abnormalities: causes of sudden death, detection by pre- participation screening, and standards for disqualification. Card Electrophysiol Rev 2002b;6:100 [PMID: 11984027].
Maron BJ et al: 36th Bethesda Conference. Eligibility recommendations for competitive athletes with cardiovascular abnormalities. J Am Coll Cardiol 2005;45(8):1318–1321 [PMID: 15837280].
Platt LS: Medical and orthopaedic conditions in Special Olympics athletes. J Athl Train 2001;36:74 [PMID: 16404438].
Putukian M, O’Connor FG, Stricker P: Mononucleosis and athletic participation: an evidence-based subject review. Clin J Sport Med 2008;18(4):309–315 [PMID: 18614881].
Rice SG; Council on Sports Medicine and Fitness, American Academy of Pediatrics: Medical conditions affecting sports participation. Pediatrics 2008;121(4):841–848 [PMID: 18381550].
Salim MA, Alpert BS: Sports and Marfan syndrome. Phys Sportsmed 2001;29:80 [PMID: 20086576].
Sanyer O: Down syndrome and sport participation. Curr Sports Med Rep 2006;5:315–318 [PMID: 17067499].
Tarnopolsky MS: Metabolic myopathies and physical activity: when fatigue is more than simple exertion. Phys Sportsmed 2002;30:37 [PMID: 20086530].
REHABILITATION OF SPORTS INJURIES
Participation in sports benefits children not only by promoting physical activity but also by the acquisition of motor and social skills. All sports participation, however, carries an inherent risk of injury. Injuries are classified as either acute or chronic. Chronic injuries occur over time as a result of overuse, repetitive microtrauma, and inadequate repair of injured tissue. When the demands of exercise exceed the body’s ability to recover, overuse injury may occur. Overuse injury accounts for up to 50% of all injuries in pediatric sports medicine. Risk factors for overuse include year round participation, participation in more than one sport at a time, poor mechanics, and training errors such as increasing exercise volume, load, frequency, or intensity too quickly. To avoid overuse injury, athletes should train with a regular variety of resistances, power, speed, agility, skills, and distance. Adequate periods of rest and recovery should be incorporated into every training regimen in order to ensure proper healing of stressed tissues. Treatment measures such as corticosteroid or platelet-rich plasma injections are more commonly used in skeletally mature athletes.
Present trends in injury rehabilitation and prevention focus on core stability training and dynamic warm-up and stretching. Core exercises emphasize isometric holds that activate the core and pelvis. They utilize light single limb movements to challenge endurance over protracted time periods. Programs should be age-appropriate and modified as needed to exercise in a pain-free range. The development of back pain during a core program signifies poor technique, overly complicated curriculum, or a prior back injury. Exercise programs can be obtained from the website resource: http://www.webexercises.com.
Dynamic warm-up and stretching programs concentrate on light movement prior to exercise. Dynamic programs use controlled, full active range of motion of each joint for an overall excitatory and stretching effect prior to exercise. The aim is to initiate light perspiration and increase heart rate, peripheral circulation, and connective tissue suppleness through simple excitatory activity. In contrast to traditional static stretching regimens in which athletes hold a stretching position for a distinct period of time, an appropriate dynamic curriculum will incorporate aerobic activity and moving stretches into sport-specific movement preparation. Areas of focus include joint range of motion, proprioception, coordination, balance, flexibility, muscular contraction, and stimulation of the central nervous system and energy resources. For example, athletes may work through a series of exercises such as side shuffle, high knee stepping, bear crawls, and double-leg hopping over cones three times. Static stretching is appropriate after exercise is complete. A useful website to design a dynamic stretching program can be found at: http://www.webexercises.com
Acute injuries or macrotrauma are one-time events that can cause alterations in biomechanics and physiology. Response to an acute injury occurs in predictable phases. The first week is characterized by an acute inflammatory response. During this time, initial vasoconstriction is followed by vasodilation. Chemical mediators of inflammation are released, resulting in the classical physical findings of local swelling, warmth, pain, and loss of function. This phase is essential in healing of the injury. The proliferative phase occurs over the next 2–4 weeks and involves repair and clean-up. Fibroblasts infiltrate and lay down new collagen. Lastly, the maturation phase allows for repair and regeneration of the damaged tissues.
The management of acute sports injuries focuses on optimizing healing and restoring function. The goals of immediate care are to minimize the effects of the injury by reducing pain and swelling, to educate the athlete about the nature of the injury and how to treat it, and to maintain the health and fitness of the rest of the body. The treatment for an acute injury is captured in the acronym PRICE:
• Protect the injury from further damage (taping, splints, braces)
• Rest the area
• Ice
• Compression of the injury
• Elevation immediately
Nonsteroidal anti-inflammatory drugs (NSAIDs) may reduce the inflammatory response and reduce discomfort. These medications may be used immediately after the injury. When safely and appropriately managed, therapeutic use of physical modalities, including early cold and later heat, hydrotherapy, massage, electrical stimulation, iontophoresis, and ultrasound, can enhance recovery in the acute phase.
The recovery phase can be lengthy and requires athlete participation. Physical therapy prescription is a common treatment modality. Initial treatment is focused on joint range of motion and flexibility. Range-of-motion exercises should follow a logical progression of starting with passive motion, then active assistive and finally active movement. Active range of motion is initiated once normal joint range has been reestablished. Flexibility exercises, particularly dynamic stretches, are sport-specific and aimed at reducing tightness of musculature. Strength training can begin early in this phase of rehabilitation. Initially only isometric exercises (static muscle contraction against stable resistance without movement of a joint or change in length of a muscle) are encouraged. As recovery progresses and flexibility increases, isotonic (change in length of a muscle without varying resistance) and isokinetic (change in length of a muscle against variable resistance without varying speed) exercises can be added to the program. These should be done at least three times per week.
As the athlete approaches near-normal strength and is pain-free, the final maintenance phase can be introduced. During this phase, the athlete continues to build strength and work on endurance. The biomechanics of sport-specific activity need to be analyzed and retraining incorporated into the exercise program. Generalized cardiovascular conditioning should continue during the entire rehabilitation treatment. Typically, return-to-play guidelines after an injury include the attainment of full joint range of motion, nearly full and symmetric strength, full speed, and nearly full sport-specific agility and skill.
Brooks GP et al: Musculoskeletal injury in the young athlete: overview of rehabilitation for nonoperative injuries. UpToDate 2012, Aug 22.
Faccioni A: Dynamic warm-up routines for sports. Faccioni Speed and Conditioning Consultancy 2004 [web PDF].
COMMON SPORTS MEDICINE ISSUES & INJURIES
INFECTIOUS DISEASES
Infectious diseases are common in both recreational and competitive athletes. These illnesses have an effect on basic physiologic function and athletic performance. Physicians, parents, and coaches can adopt the guidelines listed in Table 27–3.
Table 27–3. Sports participation guidelines: infectious diseases.
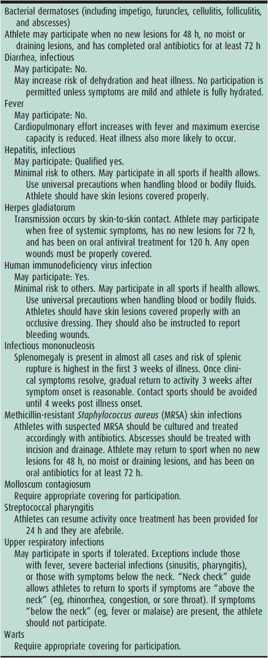
Active skin infections are common reasons to exclude athletes from sports participation. Herpes simplex, staphylococcal, molluscum, and tinea skin infections are commonly seen and most easily transmitted in sports with skin-to-skin contact and shared equipment usage. In particular, athletes are at high risk for infection with community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA). Recent reports of outbreaks in sports teams have prompted many sports organizations to adopt specific protocols to deal with the problem. Transmission is primarily by skin-to-skin contact and clinical manifestations are most commonly skin infections and soft tissue abscesses. Early treatment of CA-MRSA soft tissue infections by incision and drainage followed by appropriate antibiotic treatment is important to prevent significant morbidity and possible mortality.
Benjamin HJ, Nikore V, Takagishi J: Practical management: community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA): the latest sports epidemic. Clin J Sport Med 2007;17:393–397 [PMID: 17873553].
Selected Issues for the Adolescent Athlete and the Team Physician: A consensus statement. Med Sci Sports Exerc Nov 2008;40(11):1997–2012 [PMID: 19430330].
Rice SG and the Council on Sports Medicine and Fitness, American Academy of Pediatrics: Medical conditions affecting sports participation. Pediatrics 2008;121(4):841–848 [PMID: 18381550].
HEAD & NECK INJURIES
Head and neck injuries occur most commonly in contact and individual sports. The sports with the highest incidence of brain injury are football, bicycling, baseball, and horseback riding. Concussions most commonly occur in football, ice hockey, rugby, boxing, basketball, lacrosse, soccer, bicycling, judo, and baseball/softball. The optimal treatment of these injuries has not been established and multiple guidelines have been developed. As a general rule, treatment of head and neck injuries in young children should be more conservative because of their developing central nervous systems.
1. Concussion
Concussion is a complex process that occurs when a direct blow to the body or head translates forces into the brain. Even in the presence of neurologic symptoms, concussions are usually not associated with structural changes in brain tissue detectable by standard imaging studies. Instead, they may cause metabolic and vascular changes in cerebral tissues. Consequently, there are complex alterations in physiologic function, such as catecholamine surges and failure of cerebral blood flow autoregulation, leading to the common symptoms we ascribe to this type of injury. Symptoms may appear and evolve over the first few hours after injury. Confusion, headache, visual disturbance, posttraumatic amnesia, and balance problems are common symptoms. It is important to note that concussion does not have to involve loss of consciousness. Concussion should be suspected in any athlete with somatic, cognitive, or behavioral complaints as listed in Table 27–4. Observers may notice physical signs, behavioral changes, or cognitive impairment in the injured athlete. Diagnosis may be aided by the use of the Sport Concussion Assessment Tool v.3 (SCAT3) and the Child-SCAT3 (ages 5–12 years), which also provide standardized patient handouts (available at http://bjsm.bmj.com/content/47/5/259.full.pdf and http://bjsm.bmj.com/content/47/5/263.full.pdf). Regardless of level of participation or elite status, any athlete suspected of sustaining a concussion in a practice or competition should be immediately removed from play. The athlete should not be left alone in the initial hours after the injury in order to monitor for deterioration. An athlete diagnosed with a concussion should not be permitted to return to sport on the day of injury. In the acute setting, computed tomography (CT) is rarely indicated beyond the first 24 hours after injury. CT should be considered during initial evaluation if the patient displays deteriorating or altered mental status, prolonged loss of consciousness, repeated vomiting, severe headache, signs of skull fracture, or focal neurologic deficit or if he/she experienced a severe mechanism of injury.
Table 27–4. Concussion: symptom checklist.
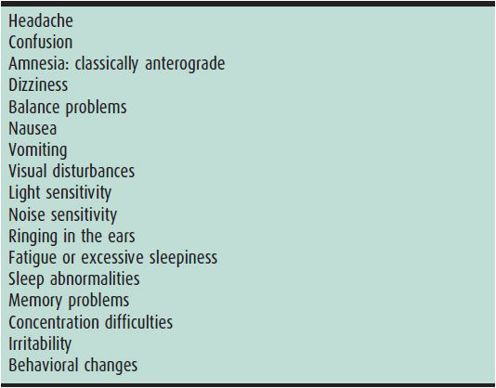
Symptoms associated with concussions usually follow a predictable pattern and most resolve in 7–10 days. Children and adolescents tend to have a longer recovery interval. Acute management of concussion includes an early period of physical and cognitive rest (1–2 days), the exact duration of which is currently unknown. Return to school and light noncontact physical activity may be reasonable early during the recovery period if symptoms are not exacerbated. In young athletes, interventions may include modified school attendance, decreased school work, reduction in technological stimulation (television, internet, computer games, cellular phone use), proper nutrition and hydration, and adequate rest and sleep. Before athletes are allowed to return to sports participation, symptoms should be resolved both at rest and during exercise without the aid of medication and a graduated return-to-play protocol should be completed. Return to play is a six-step progression with each step lasting 24 hours: (1) when asymptomatic at rest for 24 hours, progress to (2) light aerobic exercise, followed by (3) sport-specific exercise, then begin (4) noncontact drills, followed by (5) contact practice drills, and finally (6) release to game play. If any symptoms recur during any of the steps, the athlete should not move to the next stage and should rest for 24 hours, thereafter restarting at the previous step where the athlete was asymptomatic. Commonly, it is recommended that an athlete follow up with a medical provider for clearance for return to contact or collision sports, and many states have passed legislation requiring medical assessment of concussed youth and medical clearance for return to play. Current expectations are that children should return to school prior to return to sport. In general, conservative return to play guidelines should be used in children.
Among commonly used assessment tools are the SCAT3, Standardized Assessment of Concussion (SAC), Balance Error Scoring System (BESS), computerized testing, and symptoms checklist (see Table 27–4). Neuropsychological testing may be helpful in assessing the cognitive function of concussed athletes, but it should not be used as the only source of clinical decision making. It may assist in management decisions for athletes with complex cases or severe or prolonged symptoms and is best performed and interpreted by a qualified neuropsychologist. Preseason testing may provide a comparison to help practitioners assess acute concussive status, but there is no solid evidence currently to support the use of baseline neuropsychological testing.
The long-term effects of concussions or contact/collision sports have yet to be established; specifically, a cause-and-effect relationship has not been proven between concussions and chronic traumatic encephalopathy (CTE). Second impact syndrome is a controversial diagnosis primarily based on anecdotal reports. There is no universal agreement on the existence of this reported phenomenon. Advocates endorse a rare but potentially deadly complication of repeated head injury, causing loss of vascular autoregulation, catecholamine surge, increased cerebral blood pressure, and subsequent malignant cerebral edema without intracranial hematoma. Consequences include massive brain swelling and herniation leading to seizure, coma, and, possibly, death. Opponents suggest the phenomenon is actually the well-established condition of diffuse cerebral swelling, a known complication of head injury, particularly in younger individuals. The decision to retire an athlete from high risk or contact/collision sport is a sensitive and challenging one. There is currently little evidence to support a standardized approach to retirement decisions. However, considerations should include total number of concussions; increasing frequency; occurrence with serially less force; and prolonged, more severe, or permanent symptoms/signs.
Child-SCAT3. Br J Sports Med 2013;47:263 [PMID: 23479481]. http://bjsm.bmj.com/content/47/5/263.full.pdf.
McCrory P, Davis G, Makdissi M: Second impact syndrome or cerebral swelling after sporting head injury. Curr Sports Med Rep 2012;11:21–23 [PMID: 22236821].
McCrory P et al: Consensus statement on concussion in sport: the 4th international conference on concussion in sport held in Zurich, November 2012. Br J Sports Med 2013;47:250–258 [PMID: 23479479].
Randolph C: Baseline neuropsychological testing in managing sport-related concussion: does it modify risk? Curr Sports Med Rep 2011;10(1):21–26 [PMID: 21228656].
SCAT3. Br J Sports Med 2013;47:259 [PMID: 23479480]. http://bjsm.bmj.com/content/47/5/259.full.pdf.
Schatz P, Moser RS: Current issues in pediatric sports concussion. Clin Neuropsychol 2011:1–16 [PMID: 21391151].
Wetjen NM, Pichelmann MA, Atkinson JLD: Second impact syndrome: concussion and second injury brain complications. J Am Coll Surg 2010;211(4):553–557 [PMID: 20822744].
2. Atlantoaxial Instability
Atlantoaxial instability is common in children with Down syndrome because of hypotonia and ligamentous laxity, especially including the annular ligament of C1. Consequently, this condition causes increased mobility at C1 and C2. Most cases are asymptomatic. Lateral cervical neck films in flexion, extension, and neutral position evaluate the atlantodens interval (ADI). ADI is normally less than 2.5 mm, but up to 4.5 mm is acceptable in this population. Children with an ADI greater than 4.5 mm should be restricted from contact and collision activities, as well as any sport requiring excessive neck flexion or extension.
Dimberg EL: Management of common neurologic conditions in sports. Clin Sports Med 2005;24:637 [PMID: 16004923].
Klenck C, Gebke K: Practical management: common medical problems in disabled athletes. Clin J Sport Med 2007;17(1): 55–60 [PMID: 17304008].
Winell J: Sports participation of children with Down syndrome. Orthop Clin North Am 2003;34:439 [PMID: 12974493].
3. Burners or Stingers
Burners or stingers are common injuries in contact sports, especially football. The two terms are used interchangeably to describe transient unilateral pain and paresthesias in the upper extremity. These cervical radiculopathies or brachial plexopathies typically occur when the head is laterally bent and the shoulder depressed, causing exacerbation of a degenerative cervical disk or stenosis, a compressive injury to a cervical nerve root on the symptomatic upper extremity, or a traction injury to the brachial plexus of the ipsilateral shoulder. Symptoms include immediate burning pain and paresthesias down one arm generally lasting only minutes. Unilateral weakness in the muscles of the upper trunk—supraspinatus, deltoid, and biceps—also tends to resolve quickly, but can persist for weeks. The most important part of the workup is a thorough neurologic assessment to differentiate this injury from a more serious brain or cervical spine injury. The key distinguishing feature of the stinger is its unilateral nature. If symptoms persist or include bilateral complaints, headache, change in mental status, or severe neck pain, a diagnostic evaluation should include a careful neurological examination and possibly cervical spine radiographs including flexion/extension views, magnetic resonance imaging (MRI) scans, and electromyography (EMG).
Treatment consists of removal from play and observation. The athlete can return to play once symptoms have resolved, neck and shoulder range of motion is pain-free, reflexes and strength are normal, and the Spurling test is negative. The Spurling test is performed by having the head extended, rotated, and flexed to the ipsilateral shoulder while applying an axial load. Restriction of same day return to play should be considered in athletes with a history of multiple stingers, particularly if sustained in the same season. Preventative strategies include always wearing well-fitting protective gear, proper blocking and tackling techniques, and maintaining neck and shoulder strength. Long-term complications are possible, including permanent neurologic injury or repeated occurrence of stingers, which would necessitate further workup and possible lifetime exclusion from contact or collision sports.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






