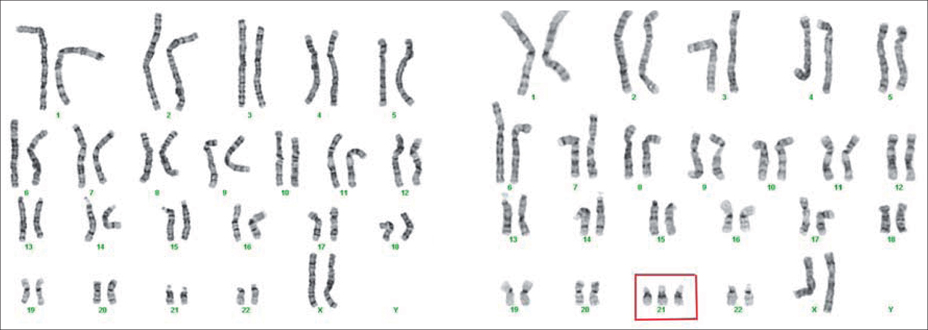
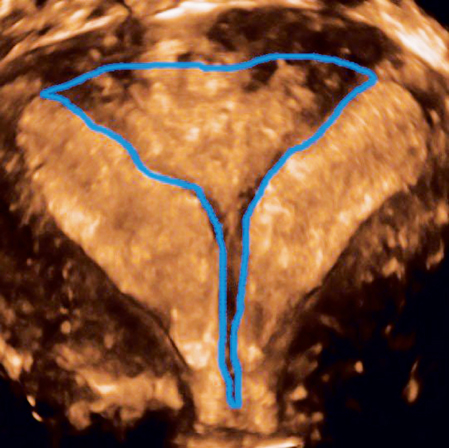
14 Spontaneous Abortion Daniela Carusi Many terms are used to describe spontaneous abortion, including miscarriage, chemical pregnancy, early pregnancy loss, embryonic or fetal demise, or blighted ovum. These refer to a pregnancy prior to 20 weeks of gestation that has ceased development, or has passed, or begun to pass, from the uterus. Though common, the event may be devastating to patients, and health care providers must be comfortable handling the woman’s medical and psychological needs through this process. Chemical pregnancy: This is a pregnancy that is identified by a positive human chorionic gonadotropin (HCG) level, which is lost prior to 5 weeks’ gestation. Clinical studies on miscarriage and recurrent pregnancy loss often do not include these common events. Blighted ovum: Development of trophoblast and a gestational sac, but no evidence of embryonic development. This may also be called an anembryonic gestation. A sac that measures 16 mm or greater in diameter with no embryo is abnormal. Missed abortion: A pregnancy is identified as “failed,” but no tissue has passed and the cervix is closed. Threatened abortion: The patient has vaginal bleeding, but the cervix is closed and the pregnancy otherwise appears viable. If a fetal heartbeat has been seen at 10 weeks’ gestation, then these patients have a 98% probability of continuing the pregnancy without a loss. Inevitable abortion: The patient has an open cervix, usually with bleeding and cramping, but the pregnancy has not passed and otherwise appears viable. Incomplete abortion: The cervix has opened and some, but not all, pregnancy tissue has passed. Completed abortion: A previously identified pregnancy has passed, the uterus has contracted down, bleeding has diminished, and the cervix has closed. HCG levels, if drawn, would fall to zero. If ultrasound scanning or pathological analyses were performed, there would be no evidence of pregnancy tissue. Septic abortion: Pregnancy loss accompanied by uterine infection or endometritis. If not promptly treated, this can develop into pelvic inflammatory disease, sepsis, and death. Molar pregnancy: This is a form of gestational trophoblastic disease marked by hydropic placental villi and abnormally high HCG levels. With a complete mole, there is no embryonic development and HCG levels may be dangerously high. With a partial mole, there may be development of a triploid fetus. Both types of molar pregnancy are nonviable. Recurrent abortion: Also called recurrent pregnancy loss (RPL) or habitual abortion, this refers to three, sequential, pregnancy losses, usually with no history of a term delivery. Such an outcome is unlikely to occur by chance, and therefore evaluation for a medical problem in the parents is indicated. Some clinicians initiate a work-up after two miscarriages. Spontaneous abortion is, unfortunately, a common event in early pregnancy: 15% of clinical pregnancies end in a spontaneous abortion, with an even higher proportion lost before 5 weeks’ gestation. The vast majority (80%) of miscarriages occur before 12 weeks’ gestation, while the risk of miscarriage after 16 weeks is less than 1%. There is a strong relationship between maternal age and risk of miscarriage. While the risk of miscarriage is 9% for a 20–24-year-old, that risk increases to 15% for a 30–34-year-old and 51% for a 40–44-year-old. Advancing age of the father may contribute as well, but to a much lesser extent. While most miscarriages are sporadic events, a history of miscarriages, particularly multiple miscarriages, increases the risk of having another. In one study, the miscarriage risk was 5% for women who had never had a prior miscarriage, 20% for those with one prior miscarriage, and 43% for those with three prior losses. Miscarriage risk has also been associated with cigarette smoking, cocaine use, high levels of cafeine intake, and extremes of body mass index. In most cases of first trimester miscarriage, no specific cause is identified. A formal evaluation is generally not performed after one or two first-trimester losses. However, a more thorough work-up is performed if a woman has had recurrent pregnancy losses or one second-trimester spontaneous abortion. Aneuploidy (an abnormal number of chromosomes) is the most common cause of first trimester miscarriage. This is usually due to random nondisjunction during egg development, and the risk increases with maternal age. Genetic or chromosomal abnormalities can also develop as the embryo develops and cells rapidly divide. Trisomy 16 is the most common aneuploidy found in early pregnancy losses. Sex chromosome abnormalities and the trisomies 21, 13, and 18 are less common, but more likely to survive beyond the first trimester (Fig. 14.1). A physical defect in the cavity of the uterus may contribute to miscarriage. These include uterine fibroids, a septum (Fig. 14.2), scar tissue, or possibly a large polyp. While this could contribute to any pregnancy loss, it should be particularly considered with second trimester or recurrent losses. Cervical insufficiency or incompetence refers to a second trimester condition in which the cervix inappropriately opens without labor. The cause of this condition is poorly understood. Blood clots forming in the placenta or uterus may lead to loss of the fetus. This is an unusual circumstance, but may occur in patients who carry a thrombophilia. This may be inherited (e. g., factor V Leiden mutation or prothrombin gene mutation) or acquired (e. g., antiphospholipid antibodies). Fig. 14.1 Normal female karyotype (left), and karyotype of a female fetus with trisomy 21 (three copies of chromosome 21, boxed in red). Placental bleeding increases the risk of miscarriage. In the first trimester this is usually identified as a subchorionic hematoma, while in the second trimester the placenta may abrupt (prematurely separate). However, hematomas are frequently seen on early ultrasound scans, and do not imply that the pregnancy will be lost. In rare cases, placental insufficiency in the second trimester may lead to oligohydramnios, growth restriction, and fetal demise. Certain viruses and bacteria may infect the placenta and fetus, leading to fetal demise in the second trimester. The infection may pass from the mother’s blood stream or it may cross directly from the vagina. Rarely, the patient may develop a severe uterine infection, also called a septic abortion, which can be fatal if not promptly treated. Miscarriage has been linked to uncorrected thyroid disease, diabetes, and hyperprolactinemia. Patients with the polycystic ovarian syndrome also have a higher rate of miscarriage than the general population. In a few women the corpus luteum produces insufficient progesterone, a condition known as luteal phase insufficiency. This is marked by a short luteal phase and recurrent chemical pregnancies, and usually requires an endometrial biopsy for diagnosis. Fig. 14.2 Three-dimensional pelvic ultrasound scan demonstrating a complete uterine septum. The fibrous septum is outlined in blue. Severe congenital abnormalities may lead to fetal demise in the second trimester. Medications, environmental exposures, and basic radiologic studies are highly unlikely to produce miscarriage. More extreme exposures, such as treatment with chemotherapeutic agents, high-dose radiation (such as for cancer treatment or thyroid irradiation), or prostaglandins can result in pregnancy loss. The risk of spontaneous loss is increased following chorionic villus sampling or amniocentesis. The risk of loss is slightly increased after nonuterine surgery performed under general anesthesia. Patients who undergo removal of the corpus luteum (owing to rupture, torsion, or hemorrhage) must have progesterone replacement prior to 9–10 weeks’ gestation in order to avoid spontaneous loss. Diagnosis of a spontaneous abortion usually involves a combination of history, physical examination, ultrasonography, and laboratory tests, though not all of these may be required. While a history and physical examination are always used, the choice of other studies depends on the gestational age of the pregnancy.
Definitions
Incidence and Risk Factors
Etiology
Chromosomal Abnormalities
Structural Problems
Thrombosis
Placental Complications
Infection
Endocrine Disorders
Fetal Abnormalities
Exposures
Procedures
Diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


