Spinal Dysraphic Lesion
Bernadette L. Koch, MD
DIFFERENTIAL DIAGNOSIS
Common
Incomplete Fusion, Posterior Element
Myelomeningocele
Lipomyelomeningocele (LMM)
Lipomyelocele (LM)
Less Common
Diastematomyelia
Dorsal Dermal Sinus
Rare but Important
Meningocele, Dorsal Spinal
Terminal Myelocystocele
Segmental Spinal Dysgenesis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Spina bifida: Incomplete closure of posterior bony elements
Spina bifida aperta = spina bifida cystica: Protrusion of spinal canal elements through posterior bony defect
Simple meningocele: Dura and arachnoid, no neural elements
Myelocele: Midline plaque of neural tissue exposed, flush with skin surface
Myelomeningocele: Myelocele protrudes above skin surface + expansion of subarachnoid space posterior to placode
Occult spinal dysraphisms develop beneath intact skin surface
Meningocele, diastematomyelia, split notochord syndrome, dorsal dermal sinus, fibrolipoma of filum terminale, spinal lipoma, lumbosacral hypogenesis, segmental spinal dysgenesis, myelocystocele
Helpful Clues for Common Diagnoses
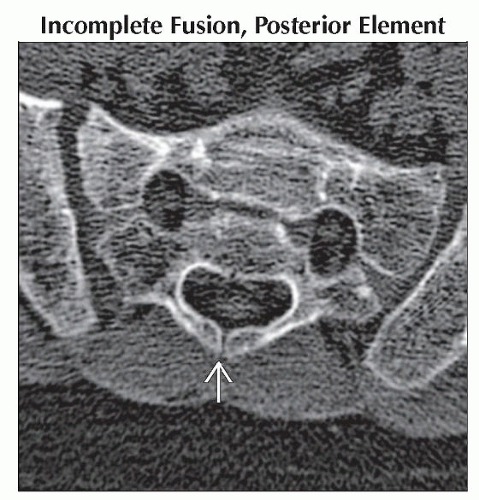
Incomplete Fusion, Posterior Element
Key facts: Spina bifida occulta
Imaging
Incomplete fusion of spinous process/lamina without underlying neural or dural abnormality
Lumbosacral > cervical > thoracic
Myelomeningocele
Key facts: Open neural tube defect, lacks skin coverage
Level of dysraphism determines neurological deficit
Rarely image spine preoperatively
Postoperative spinal imaging if neurological decline despite adequate treatment of hydrocephalus or if neurologic exam suggests additional underlying lesions
Imaging
CSF sac and neural elements protrude through wide osseous dysraphism
Fetal elongation of low-lying cord, usually in dorsal aspect of canal deep to skin-covered postoperative repair
Associated abnormalities
Chiari 2 malformation (≈ 100% )
Hydrocephalus, kyphoscoliosis, segmentation anomalies, diastematomyelia and dermal sinus, syrinx, intraspinal dermoid/epidermoid, orthopedic abnormalities
Lipomyelomeningocele (LMM)/Lipomyelocele (LM)
Key facts: Cutaneous stigmata in up to 50%; hemangioma, dimple, dermal sinus, skin tag, or hairy patch
Imaging
LMM = spinal subarachnoid space expanded ventrally → placode, tethered cord, subarachnoid space, and dura extend dorsally through spina bifida
LM = tethered cord and junction between placode and lipoma within spinal canal, lipoma through bony defect
Lipoma attached to dorsal aspect of neural placode and contiguous with SQ fat
Dorsal and ventral nerve roots exit from ventral surface of placode
± segmentation anomalies, sacral anomalies, syrinx, diastematomyelia, anorectal and GU abnormalities
Diastematomyelia
Key facts: Majority between T9 and S1
Imaging
Split cord malformation (SCM) = sagittal split into 2 hemicords ± fibrous, osteocartilaginous, or osseous spur
Pang type 1 SCM = separate dural sac, arachnoid space around each hemicord, separated by fibrous/osseous spur
Pang type 2 SCM = single dural sac and arachnoid space without spur ± adherent fibrous bands tethering cord
Nearly all reunite below split
± thick filum, tethered cord, syringohydromyelia in 1 or both hemicords, myelocele, or MM
± intersegmental laminar fusion ≈ pathognomonic for diastematomyelia
Helpful Clues for Less Common Diagnoses
Dorsal Dermal Sinus
Key facts
Midline or rarely paramedian dimple or pinpoint ostium ± pigmented patch, hairy nevus, or cutaneous hemangioma
Differentiate from simple sacral dimple (< 2.5 cm from anus, extends inferiorly toward coccyx) and pilonidal sinus (low ostium, does not enter spine)
High suspicion if dimple above intergluteal fold
Imaging
↓ curvilinear tract through ↑ SQ fat May end in SQ tissue or extend into canal, terminating in conus medullaris, subarachnoid space, filum terminale, nerve root, fibrous nodule on surface of cord, or dermoid/epidermoid cyst
Dural “tenting” at dural penetration
LS > occipital > T > C spine
± varying degrees of dysraphism; incomplete posterior element fusion → multilevel dysraphism
± dermoid/epidermoid, abscess, or arachnoiditis
± cord tethering in lumbosacral lesions
Helpful Clues for Rare Diagnoses
Meningocele, Dorsal Spinal
Key facts: Skin covered
Imaging
Meninges protrude through dysraphism into SQ fat
Cord tethering and syrinx rare
Terminal Myelocystocele
Key facts: Large skin-covered mass, usually sacral/coccygeal
Imaging
Hydromyelic tethered cord traverses dorsal meningocele, terminates in dilated terminal ventricle
Segmental Spinal Dysgenesis
Key facts: Focal dysmorphic/hypoplastic vertebrae, meninges, and spinal cord with normal spine above and below
Imaging
Dysplastic vertebrae → severe focal kyphosis
Thecal sac narrows and then terminates; spinal cord narrows and disappears rostral to thecal sac
Thecal sac reappears below dysplastic segments
Spinal cord reappears below reappearance of thecal sac
Image Gallery