Special Intensive Care
Thomas A. Parker
MECHANICAL VENTILATION
Respiratory failure is one of the most common problems requiring admission to the neonatal intensive care unit. Respiratory failure is often the final result of restrictive lung disease with regional or global alveolar collapse or consolidation. In order to achieve optimal alveolar gas exchange, the lung needs to be inflated at end expiration (at functional residual capacity) and have sufficient tidal and minute ventilation to eliminate carbon dioxide.1 Under optimal conditions, several factors help prevent the collapse of alveoli at the end of expiration and thereby maintain an adequate functional residual capacity. Surfactant, which is produced in the type II cells of the lung, dramatically reduces surface tension and opposes the tendency of alveoli to collapse when lung volume is at its lowest. In addition, the rigidity of the chest wall opposes lung collapse. In comparison to the adult, several factors present disadvantages for the neonate’s capacity to maintain optimal lung volumes. The neonatal chest is highly compliant, which limits its ability to oppose elastic recoil and collapse during expiration and increases the potential for the development of collapse. This problem is greatly exacerbated in the setting of surfactant deficiency or inactivation, in which unopposed surface tension dramatically increases the chance of alveolar collapse during expiration. Lastly, although the small diameter of the neonatal tracheobronchial tree generally is sufficient to provide unimpeded airflow, further small reductions in its diameter can dramatically increase resistance and adversely affect gas entry and egress.
A hallmark of treatment for most causes of neonatal respiratory failure is the provision of positive airway pressure.2 (See also Chapter 102.) Application of pressure to the proximal airway may result in several beneficial effects. Most importantly, positive pressure opposes the tendency of end-expiratory alveolar collapse caused by elastic recoil and high surface tension. Moreover, positive proximal airway pressure increases the pressure differential between the upper airway and the distal airspace during spontaneous respiratory effort, facilitating increased bulk flow of gas down the tracheobronchial tree. In addition, positive pressure may help to maintain adequate patency of the airway in disease states characterized by inflammation, plugging, or anatomic (either fixed or dynamic) narrowing of the airway.
 CONTINUOUS POSITIVE AIRWAY PRESSURE (CPAP)
CONTINUOUS POSITIVE AIRWAY PRESSURE (CPAP)
The least invasive means for consistently delivering proximal distending airway pressure is via CPAP.3 CPAP may be delivered via prongs, which are placed in the nose, or by a mask affixed over the mouth and nose. Generally, CPAP is provided at a pressure range of 4 to 8 cm H2O, with the specific level based on the type and severity of the underlying lung disease, the degree of inflation achieved, and the baby’s tolerance of the therapy. Common indications for use of CPAP in the neonatal intensive care unit include mild hyaline membrane disease, disease or narrowing of the airways, and as a bridge to extubation in preterm infants recovering from hyaline membrane disease.4 CPAP may also decrease the incidence or severity of apnea and bradycardia in some preterm infants, likely by improving chest wall stability and helping to maintain airway patency. In recent years, some investigators have advocated early use of CPAP, either in place of or after surfactant replacement, as a means for providing respiratory support for infants with hyaline membrane disease while avoiding the potentially injurious use of more invasive ventilatory support.5 Although most babies treated with CPAP can be concurrently fed successfully via a nasogastric tube, some may develop intolerable gastric and intestinal distension. Vigilant observation and care of the nasal septum and columnella is necessary because both CPAP prongs and ventilation masks can cause pressure necrosis of these structures.
 CONVENTIONAL POSITIVE PRESSURE VENTILATION
CONVENTIONAL POSITIVE PRESSURE VENTILATION
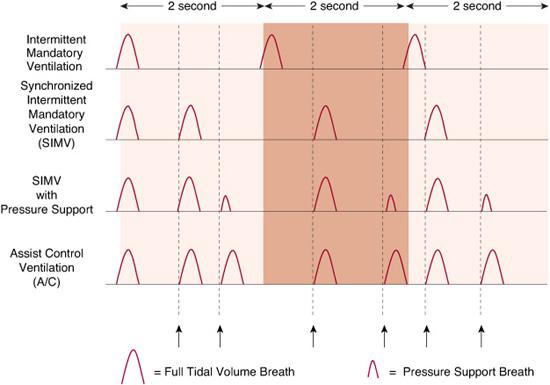
In many cases of respiratory compromise in the neonate, CPAP alone does not provide adequate support, and more invasive therapy, including intubation and formal mechanical ventilation, is required.6Conventional ventilation of the newborn generally refers to the use of intermittent positive pressure ventilation, or IPPV, whereby a ventilator provides alternating cycles of positive end-expiratory pressure (PEEP) and discrete inflating “breaths.” A common feature of these ventilators is the use of a continuous flow of oxygen-enriched gas through the ventilator circuit, providing an ongoing source of fresh gas during spontaneously breathing. Partial closure of a valve in the expiratory portion of the circuit during the inspiratory cycle diverts gas down the endotracheal tube, delivering a breath to the patient. The size of each full inflating breath is determined by the specific ventilator mode employed. Typically, such ventilators are time-cycled, meaning that they provide a breath at discrete intervals, based on the set rate, and for a defined period (the inspiratory time). Should the patient be breathing spontaneously, most modern ventilators now have the capacity to detect the patient’s spontaneous effort and to synchronize each delivered breath to a spontaneous inspiratory effort during each respiratory cycle (a technology called SIMV, or synchronized intermittent mandatory ventilation). In addition, some neonatal ventilators now offer a pressure support option whereby all intervening spontaneous breaths that do not qualify for a full ventilator breath are provided with a modest increase in inspiratory pressure (generally 4–8 mm Hg) intended to help overcome the resistance to airflow in the endotracheal tube and decrease the work of breathing. An alternative mode now available on some ventilators is “assist-control” in which each spontaneously initiated respiratory effort detected by the ventilator is supported with a full tidal volume breath as shown in Figure 61-1.
In pressure-limited ventilation, gas is diverted into the endotracheal tube at a preset pressure, the peak inspiratory pressure (PIP). The volume of gas delivered in this mode depends on the underlying lung compliance; highly compliant lungs receive a greater volume of gas than those that are poorly compliant. Optimal inflating pressures cannot be generalized because of the wide variability in the type and severity of underlying lung disease among infants. With some newer generation neonatal ventilators, volume-targeted ventilation is now possible.7 In this mode, a specified volume of gas is diverted down the endotracheal tube. The pressure required to deliver this volume depends on the compliance and resistance in the lung. Volume-targeted ventilation offers the theoretic advantage of providing consistent gas volumes in the setting of rapidly changing lung compliance, a situation common to many forms of neonatal lung disease, such as hyaline membrane disease. It should be noted that most ventilators, when in a volume mode, require that the operator set a pressure limit that will not be exceeded during the inspiratory phase even if the desired volume is not delivered. This can lead to inconsistent tidal volumes and inadequate ventilation. Target settings for tidal volume (VT) generally are 4 to 8 ml/kg. Regardless of the inspiratory mode used with conventional ventilation, positive end-expiratory pressure should be provided to minimize end-expiratory alveolar collapse. Generally, a positive end-expiratory pressure of 4 to 8 mm Hg is used for most neonates, though higher levels may be optimal in the setting of significant disease of the airways. Most practitioners recommend assessing multiple parameters to guide the pressure or volume used to ventilate a newborn, including gas exchange, clinical assessment of air entry (both visual and auscultatory), and radiographic assessment of lung inflation.
Currently, there is no consensus on the most efficacious and least injurious conventional mode of ventilation for neonates. Many of the newer neonatal ventilators can employ either a pressure-limited or volume-targeted strategy and allow the practitioner to monitor a number of sensitive and sophisticated ventilatory measurements regardless of the mode employed. In addition, many of these newer ventilators offer modes that are beyond the scope of this discussion, each of which may theoretically improve gas exchange or reduce ventilator-induced lung injury. None of these newer modes have been widely embraced, but ongoing studies may ultimately provide compelling evidence of benefit over the more basic strategies just discussed.
 HIGH-FREQUENCY VENTILATION (HFV)
HIGH-FREQUENCY VENTILATION (HFV)
HFV offers an alternative to the conventional ventilation approaches described previously. As the name implies, HFV employs supraphysio-logic rates, generally in the range of 300 to 700 breaths per minute, and very small tidal volumes, sometimes less than the anatomic dead space. The physiologic mechanisms by which HFV achieves ventilation are very complex, and this mode of ventilation can be extremely efficient, including in babies who are not effectively ventilated using a conventional strategy. In the United States, 3 different high-frequency modes are employed clinically. In high-frequency oscillation, gas is delivered by the forward and aft movement of a diaphragm, which “oscillates” about a set mean airway pressure. This mode of HFV is distinguished from others because of its active expiratory phase. In high-frequency jet ventilation, brief pulses of gas are delivered directly into a port on a specially designed endotracheal tube, while a conventional ventilator simultaneously provides a set positive end-expiratory pressure or mean airway pressure. In high-frequency flow interruption, a central stream of gas is interrupted at a rapid rate. Unlike high-frequency oscillation, both high-frequency jet ventilation and high-frequency flow interruption allow for the use of regular “background” breaths, which are conventional tidal breaths typically provided several times per minute.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


