Soft Tissue Mass
Christopher G. Anton, MD
DIFFERENTIAL DIAGNOSIS
Common
Ganglion Cyst
Lipoma
Hematoma
Vascular Malformation
Hemangioma
Fat Necrosis
Less Common
Rhabdomyosarcoma (RMS)
Myositis Ossificans
Neurofibroma (NF)
Synovial Sarcoma
Rare but Important
Extraosseous Ewing Sarcoma (EOES)
Fibromatosis
Fibrosarcoma (FS)
Malignant Peripheral Nerve Sheath Tumor
Lipoblastoma
Liposarcoma
Other Sarcomas
Congenital or Infantile
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Some soft tissue masses can be diagnosed by clinical exam
Lipoma: Superficial & doughy by palpation
Ganglion cyst: Transilluminates and near joint
Others need further evaluation by radiographs and then MR
MR will help differentiate determinate from indeterminate lesions
Determinant lesions: Neurofibroma, vascular malformations, hematoma, lipoma
Excision biopsy or monitoring
Indeterminate: Underlying pathology is uncertain
Needle biopsy to determine management
Helpful Clues for Common Diagnoses
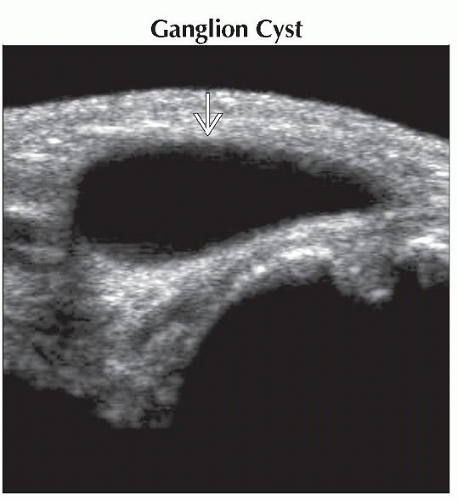
Ganglion Cyst
MR: Homogeneous hyperintense T2 signal cystic mass, peripheral enhancement
Communicates with joint space or tendon sheath
Lipoma
May represent up to 1/3 of all soft tissue masses
May appear lucent on radiographs
MR: Follows subcutaneous fat signal on all pulse sequences
Hint: Use fat-suppression sequences
May have thin septations
Intramuscular lipomas may appear more complex with infiltration and poor definition
Hematoma
MR: Hemorrhagic products
Hyperintense T1 and hypo- to hyperintense on T2 with “blooming” on gradient echo sequences
Must use caution; may be difficult to differentiate from soft tissue sarcoma with hemorrhage
Vascular Malformation
Present at birth
Venous: Low-flow lesion on gradient echo MR images with thrombi, phleboliths, and diffuse contrast enhancement
May see calcified phleboliths on radiographs
Lymphatic: Low-flow lesion on gradient echo MR images with septal enhancement and often fluid-fluid levels
Arteriovenous: High-flow lesion on gradient echo MR images; tangle of vessels without enhancing soft tissue mass
Hemangioma
True neoplasm
Small or absent at birth, rapid growth over 1st several months, involutes over months to years
MR: Hyperintense on T2, vascular flow voids (high flow on GE images), intense post-contrast enhancement
May have fatty component when involuting
Ultrasound: High vessel density (> 5 vessels/cm2)
Strawberry skin discoloration if superficial or bluish in deeper hemangiomas
Fat Necrosis
Helpful Clues for Less Common Diagnoses
Rhabdomyosarcoma (RMS)
Most common soft tissue sarcoma in children
Embryonal RMS: 60-70% of childhood RMS
Typically < 15 years old; more common in GU and head and neck
Alveolar RMS: Adolescents; most common in extremity, trunk, perianal/perirectal
Alveolar and extremity RMS tend to have worse prognosis
Myositis Ossificans
Ring-like peripheral calcifications
Neurofibroma (NF)
Frequently multiple and seen in neurofibromatosis type 1
May be sporadic and solitary
“Target” sign or “bag of worms”
Synovial Sarcoma
2nd most common sarcoma in childhood, 15-35 years old
Calcifications in 1/3 can appear nonaggressive on MR, near joint; when extensive, improved prognosis
Helpful Clues for Rare Diagnoses
Extraosseous Ewing Sarcoma (EOES)
May erode adjacent bone
Fibromatosis
MR: Typically hypointense to skeletal muscle on T1 and hyperintense with areas of hypointensity on T2, may enhance
Fibrosarcoma (FS)
Infantile FS < 5 years old; more common in lower extremities, heterogeneous enhancement, local recurrence
Rarely metastasizes, better prognosis than adult FS
Malignant Peripheral Nerve Sheath Tumor
Most commonly associated with NF1 (50%); more common in lower extremities
Must consider malignant degeneration of neurofibroma if erodes bone, painful, rapid growth, and loss of “target” sign
Lipoblastoma
Primarily < 3 years old, superficial arms and legs (deeper in lipoblastomatosis)
MR: Composed of fat and myxoid tissue, hyperintense on T1, heterogeneous on T2
Liposarcoma
Myxoid subtype more common, bright on T2 with heterogeneous enhancement
Well-differentiated subtype; looks like lipoblastoma (but > 3 years old)
Other Sarcomas
PPNET, epithelioid sarcoma, MFH, ASPS
Congenital or Infantile
Infantile myofibromatosis, fibrous hamartoma of infancy, congenital-infantile fibrosarcoma, etc.
Image Gallery
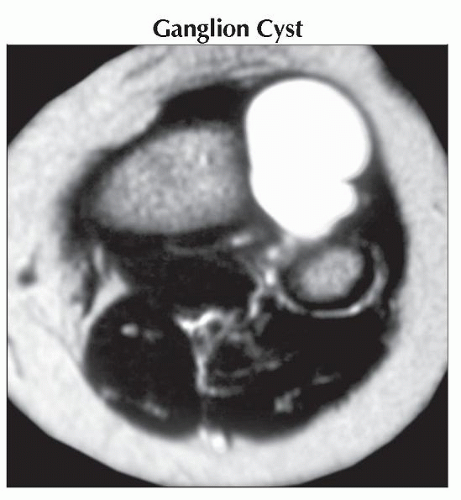 Axial T2WI MR shows a bright hyperintense signal mass extending from the proximal tibia-fibia joint. The mass demonstrated peripheral enhancement (not shown), typical of a ganglion cyst.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|