Essential Features
- • The biology of the developing cervix may increase the risk for STDs in young women.
- • Adolescents have delayed health care–seeking behavior and may not be forthcoming in reporting sexual risk behavior.
- • In most states, patients 12 years and older can give consent for confidential reproductive health care services.
General Considerations
Nearly one quarter of all sexually transmitted diseases (STDs) occur in sexually active adolescents. A variety of biologic, cognitive, psychological, behavioral, and social factors contribute to the high rates of STDs observed in this population. To provide effective care for these patients, it is important that clinicians understand the issues that contribute to adolescents’ increased STD risk.
Not all adolescents are sexually active. According to the 2003 Youth Risk Behavior Surveillance System (YRBS), 46.7% of high school students reported having had sexual intercourse during their lifetime. Only 28–63% of those who were sexually active reported having used a condom during their last intercourse. STDs commonly go undiagnosed in adolescents because (1) infections are often asymptomatic, (2) routine screening relies on appropriate health care–seeking behavior, and (3) adolescents must identify themselves as sexually active. STDs in adolescents result in complications such as infertility, ectopic pregnancy, HIV infection, and cervical cancer.
Epidemiology
Adolescents have the highest age-specific rates for chlamydia and gonorrhea. In 2003, the highest age-specific chlamydial rates were among female adolescents aged 15–19 years (2687.3 per 100,000 females vs 9.8 per 100,000 males, Figure 23–1). As with chlamydia, gonorrhea rates are highest in female adolescents aged 15–19 years, and in men aged 20–24 years (see Figure 23–2).
Age-specific national prevalence estimates and case reporting data for genital herpesvirus infection, genital warts or other human papillomavirus (HPV) infections, and trichomoniasis are not available. The most common ulcerative disease among adolescents is herpes simplex virus type 2 (HSV-2). According to the National Health and Examination (NHANES) III data (1988–1994), seroprevalence rates among adolescents aged 12–19 years range from less than 10% to 17% in some reports. HPV is one of the most common STDs in adolescent and young adult women, with a prevalence of 30–50% in this population. Various studies report that trichomoniasis is found in 5–10% of the general population and in 18–50% of women with vaginal complaints.
Syphilis is typically not considered an adolescent disease. The incidence was highest among women aged 20–24 years (2.4 cases per 100,000 population) and among men aged 35–39 years (11.8 cases per 100,000 population) in 2003.
Nearly half of all new HIV infections in the United States occur in adolescents and young adults aged 13–24 years. It is estimated that as many as 100,000 adolescents are infected with HIV, of whom 25% are unaware of their status.
STD rates have been disproportionately higher among African-American adolescents relative to same-age Caucasian counterparts. There does not appear to be a biologic basis for such differences, and the cause of this health disparity is unclear but may be attributable, in some degree, to higher rates of poverty, lack of access to quality health care, and living in high-prevalence communities. Reporting bias may also contribute to the high rates of STDs in minority communities, because minority populations are more likely to seek care at clinics that receive public funding, which may be in better compliance with reporting regulations than private providers. Additionally, sexual networks may explain why African-American adolescents who reside in a high-prevalence community are at increased risk of having sexual activity with a concurrent partner exposed to an STD.
Factors that Increase the Risk of STDs in Adolescents
Overall, female adolescents appear to be more susceptible to STDs than male adolescents. Different pathogens preferentially infect different tissues: Neisseria gonorrhoeae and Chlamydia trachomatis preferentially attach to columnar cells, Trichomonas vaginalis and HPV attach to squamous epithelium, and Treponema pallidum infects squamous and columnar epithelial cells.
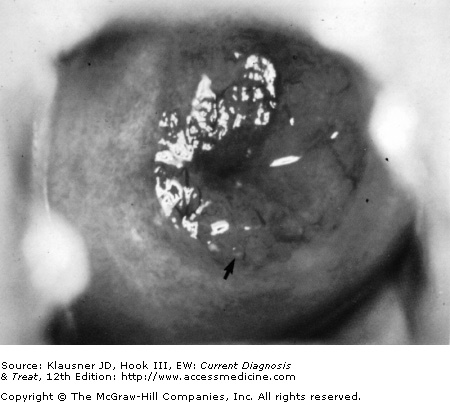
Many biologically plausible factors may contribute to increased adolescent susceptibility to infection. For instance, the cervix is physiologically immature in adolescent and young adult women, making it particularly vulnerable to STDs. During puberty, the epithelium lining the lower genital tract begins to thicken and undergo squamous metaplasia, the process during which readily infected, undifferentiated columnar (immature) epithelial cells transform into less susceptible squamous (adult) epithelium (see Figure 23–3). The junction of columnar and squamous epithelium is separated by squamous metaplastic epithelium referred to as the transition zone. In adolescents, this area on the exocervix is referred to as the zone of ectropion. The zone of ectropion is the preferential site of C trachomatis and N gonorrhoeae infections and thus biologically places female adolescents at risk for acquisition of multiple STDs, including HIV and pelvic inflammatory disease (PID), as well as abnormal Papanicolaou (Pap) smears.
Figure 23–3.
Presence of cervical ectopy. Endocervical columnar epithelium is present in an ectopic position on the exocervix, giving a bright-red circumoral appearance. Cervical mucus is clear, not purulent. (Reproduced, with permission, from Holmes KH et al. Sexually Transmitted Diseases, 3rd edition. McGraw-Hill, 1999.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree