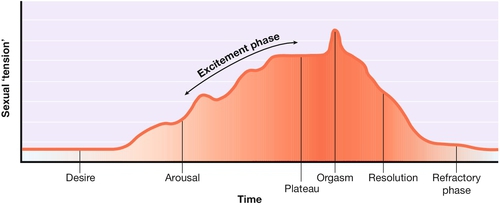
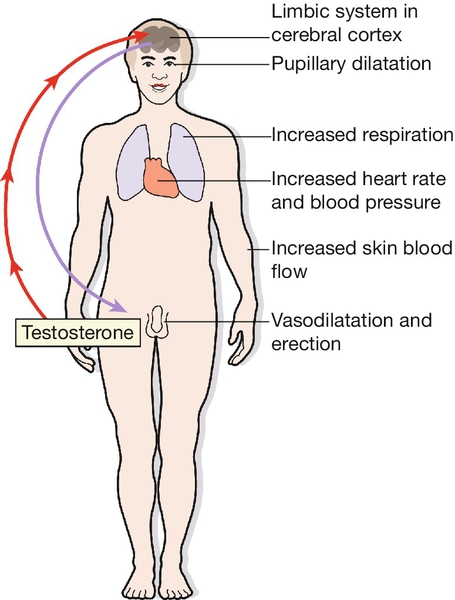
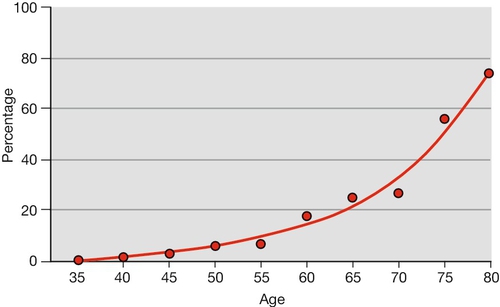
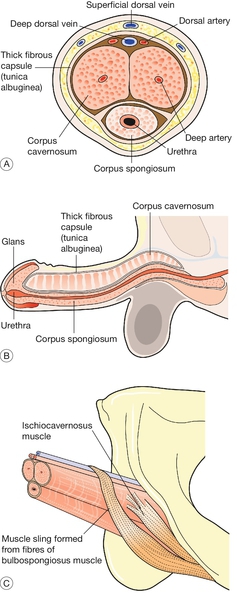
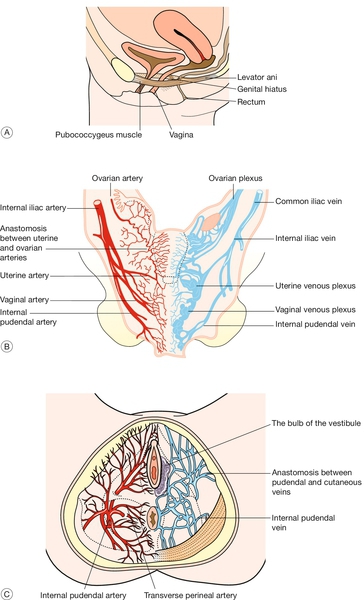
25 It is important for any doctor to be able to take a sexual history and to have some idea of how sexual problems are managed. Understanding the physiology of the normal sexual response will allow the doctor to better understand many of the uncomplicated sexual problems. Scientific investigation of the normal sexual response is necessary to our understanding, but, because of society’s disapproval, few scientists have chosen to work in this area until recently. Early workers were: The normal human sexual response can be regarded as having five phases: desire, arousal, orgasm, resolution and the refractory phase (Fig. 25.1). Sexual desire refers to the general level of interest in sexuality. It is modulated by hormones – hence the change in sexual interest at puberty. The main hormonal modulator in both sexes is testosterone. Desire is also dependant on contextual factors such as mood, environment and levels of sexual attraction. This phase has three components: central arousal, genital response and peripheral arousal. This refers to the response to sexual stimuli, which may be visual or tactile or may result from internal imagery or from a relationship. These stimuli act through the cerebral cortex (Fig. 25.2). The areas of the brain involved in sexual arousal are thought to be in the limbic system. There are thought to be excitatory centres with endorphins as the neurotransmitter, and inhibitory centres, linked to the centres for pain and fear. The spinal pathways leading to the genitalia are not precisely known but appear to be near the spinothalamic pathways for pain and temperature. Genital responses are due to vasocongestion and neuromuscular changes. Arteriolar dilatation is probably controlled by the parasympathetic sacral outflow at S2, 3 and 4 via the nervi erigentes. Thoracic sympathetic outflow also plays a part. The local neurotransmitters involved include vasoactive intestinal polypeptide (VIP), a potent vasodilator found in the penis and vagina. In the male, engorgement of the corpora cavernosa is due mainly to arteriolar dilatation and probably a reduction in the venous outflow which results in penile erection (Fig. 25.3). The scrotum tightens due to contraction of the dartos muscle and the testes are elevated due to contraction of the cremaster muscle. (A) Cross-section showing erectile spaces and principal blood vessels. (B) Erectile tissues. Each crus of the corpora cavernosa is inserted into the pubic bone. (C) Muscles. In the female, there is engorgement of the venous plexus surrounding the lower part of the vagina, and of the erectile bulbs of the vestibule on either side of the introitus (Fig. 25.4). There is reddening and pouting of the labia minora. The clitoris becomes erect and later is said to retract against the symphysis pubis. Fig. 25.4Female reproductive organs. (A) The muscular supports of the vagina. This shows the sling of muscle fibres that surround the urethra, vagina and rectum, running from the pubic bone to the coccyx. The levator plate formed by these fibres supports the rectum and vagina in its non-aroused horizontal position. (B) Arteries and veins supplying the female reproductive organs. (C) Blood vessels of the pelvic floor, showing the rich arterial and venous networks surrounding the vaginal opening. The vagina becomes lubricated by a transudate as the blood supply to the vaginal wall increases. This fluid is not the product of mucous glands: beads of fluid appear all over the vaginal wall. Mucus secretion from the cervix makes relatively little contribution to vaginal lubrication (which is therefore usually unaffected by hysterectomy). Secretion from Bartholin’s glands, formerly thought to be mainly responsible for lubrication, is only moderate in amount and occurs relatively late during arousal. Relaxation of the woman’s pelvic floor muscles occurs after vaginal lubrication has started. In the later stages of arousal, the uterus becomes engorged, increases in size and rises in the pelvis. The upper part of the vagina ‘balloons’ and there may be slow irregular contractions of the lower third of the vagina. In both sexes, but particularly in the male, the genital response interacts with the central response, so that arousal becomes self-amplifying. Sexual arousal causes: When arousal is complete, there may be a ‘plateau’ phase during which the couple prolong the pleasure of intercourse before orgasm. If this continues too long, however, coitus may become painful for one or both partners. Orgasm involves genital, muscular and sensory changes, as well as cardiovascular and respiratory responses. First, there is smooth muscle contraction of the epididymis, vas deferens, seminal vesicle, prostate and ampulla, propelling seminal and prostatic fluid into the urethral bulb. Then, the male becomes aware that orgasm is imminent and ejaculation usually follows within a few seconds. The internal bladder sphincter remains shut but the external sphincter relaxes and semen is propelled along the urethra by rhythmic contractions of the bulbospongiosus and ischiocavernosus muscles. A few seconds after the onset of the subjective experience of orgasm, there is a spasm of the muscles surrounding the lower third of the vagina (the ‘orgasmic platform’) followed by a series of rhythmic contractions, usually five to eight in number. These do not expel fluid from the vagina. Uterine contractions may also occur. There is contraction of rectus abdominis, pelvic thrusting, contraction of the anal sphincter and sometimes carpopedal spasm. Systolic and diastolic blood pressure rises by at least 25 mmHg, and hyperventilation occurs. There is a feeling of intense pleasure and an alteration of consciousness to a variable degree. The events of arousal are gradually reversed. In men, there is a moderate immediate loss of erection, followed by a slower complete reversal. In women, if no orgasm has occurred, pelvic congestion may take hours to resolve and may be uncomfortable. In both sexes, there is a subjective feeling of relaxation, though its duration may differ between the man and the woman. There follows an interval during which further stimulation does not produce a response. In men, this varies from minutes in young men to many hours in older men. Some women do not experience a refractory period, only a minority of women (14% according to Kinsey) can have multiple orgasms. Normal sexual behaviour differs from couple to couple. It also alters with age and with the evolution of a sexual relationship. Patients may present with problems due to difficulties in adjusting to the change from one phase to the next of a relationship. An adolescent usually has a higher capacity for sexual arousal and a need to discover their sexual attractiveness. However, coupled with the need to learn about sexual behaviour there is an emotional vulnerability. Unsatisfactory sexual experience at this time can result in continuing problems later as a result. Young women in their teens are at a higher risk of unwanted pregnancy due to uncertainty about contraceptive needs. The early months of a relationship may be characterized by frequent sex, but couples need to learn quickly how to establish good communication and to adjust their sexual behaviour to suit each other’s needs, as desire usually wanes as a relationship progresses. Should this communication not occur, dysfunctional patterns may develop potentially resulting in sexual problems and relationship difficulties. The time taken for sexual interest to return after childbirth is variable and in some women, can be a year or more. Problems can result from a difficult birthing experience or postnatal depression but more commonly are due to tiredness and the difficulties coping with the demands of the new baby. When the novelty of a sexual relationship has worn off, sexual activity usually becomes less frequent and this may cause anxieties. Couples may feel they ‘ought’ to be having sex more often. Stresses at work for both partners in combination with social commitments can make it difficult for them to find time to relax together. In the years before the menopause, women often have menstrual problems. After the menopause, there may be a reduction in sexual interest or a problem with vaginal dryness; these can usually be corrected by hormone replacement therapy. There is a decline in erectile function with age, which can be a manifestation of physical disease (Fig. 25.5). Postmenopausal women may experience low libido and vaginal dryness or atrophy. These factors can impact on the couple’s sexual relationship. It is important to remember how much people differ from one another and how wide the range of normality may be. Reproductive sex is often limited to a short interval in a couple’s relationship once conception has occurred. Couples who have fertility problems may find that it causes difficulty with their sex life, or conversely may find, that after they achieve pregnancy it is difficult to have sex for pleasure only. Sexual activity is a form of physical exercise, which improves self-esteem and feelings of well-being but is also something to bear in mind in people with physical problems, such as angina. Though sex is readily associated with pleasure, there are in some cultures taboos that prevent some people from enjoying sex. Enjoying sex means lowering one’s defences, and sharing this experience strengthens the bond between partners. People who have had to build particularly strong defences, for example, after emotional abuse in childhood, may have difficulty in relinquishing them. People may use sexual activity to reassure themselves about their sexuality. Satisfactory sex can improve one’s self-esteem however, for some, promiscuous behaviour to accomplish this can have negative consequences. Some people see the sexual relationship in terms of dominance and submission. This can apply to coitus itself, or to the power to allow or deny access to sex. Rape can be seen as an example of this. This can be helpful for most people but in some cases, can cause relationship or personal problems through risk taking, for example, promiscuity or use of internet pornography. Prostitution is the most obvious form of sex for gain, and is often the result of poverty. Marriage, even nowadays, may also be a way of using sex to buy security. Some sexual problems may present as another symptom such as pelvic pain, or are discovered fortuitously, for example, when a routine enquiry is made about contraception. It is not possible to take a detailed sexual history from every patient whatever their complaint, but it is reasonable, particularly in a gynaecological clinic, to ask one or two questions about sex as a routine; for example, ‘Do you have any trouble with intercourse?’ or, if appropriate, ‘Is this symptom worse after intercourse?’ An evasive reply may suggest that all is not well which may require some further sensitive questioning.
Sexual problems
Introduction
![]() Sigmund Freud (1856–1939), an Austrian doctor, was the founder of psychoanalysis and the first to recognize the importance of childhood influences on sexuality. His studies were on patients rather than normal subjects.
Sigmund Freud (1856–1939), an Austrian doctor, was the founder of psychoanalysis and the first to recognize the importance of childhood influences on sexuality. His studies were on patients rather than normal subjects.
![]() Havelock Ellis (1859–1939) studied medicine at St Thomas’s Hospital, London. His seven-volume Studies in the Psychology of Sex (1897–1928) caused controversy but was the first detached treatment of the subject.
Havelock Ellis (1859–1939) studied medicine at St Thomas’s Hospital, London. His seven-volume Studies in the Psychology of Sex (1897–1928) caused controversy but was the first detached treatment of the subject.
![]() Alfred Kinsey (1894–1956), an American zoologist, became director of Indiana University’s Institute for Sex Research in 1942. To investigate ‘normal’ sexual experience, 18 500 Americans were interviewed. Sexual Behaviour in the Human Male was published in 1948, and Sexual Behaviour in the Human Female in 1953.
Alfred Kinsey (1894–1956), an American zoologist, became director of Indiana University’s Institute for Sex Research in 1942. To investigate ‘normal’ sexual experience, 18 500 Americans were interviewed. Sexual Behaviour in the Human Male was published in 1948, and Sexual Behaviour in the Human Female in 1953.
![]() Masters and Johnson: William Masters (1915–2001), a doctor, and Virginia Johnson (1925–2013), a psychologist, working at Washington University, St Louis, carried out the first direct observations on sexual activity under laboratory conditions. Human Sexual Response appeared in 1966, and Human Sexual Inadequacy in 1970.
Masters and Johnson: William Masters (1915–2001), a doctor, and Virginia Johnson (1925–2013), a psychologist, working at Washington University, St Louis, carried out the first direct observations on sexual activity under laboratory conditions. Human Sexual Response appeared in 1966, and Human Sexual Inadequacy in 1970.
![]() The field of sexual medicine or sexology has developed significantly since the early work of these pioneers and is now a flourishing specialty in itself. There are numerous societies, conferences and journals devoted to the field. Despite this, it is still a super specialism and not everyone has access to services for sexual problems.
The field of sexual medicine or sexology has developed significantly since the early work of these pioneers and is now a flourishing specialty in itself. There are numerous societies, conferences and journals devoted to the field. Despite this, it is still a super specialism and not everyone has access to services for sexual problems.
Normal sexual response
Desire
Arousal
Central arousal
Genital response
Peripheral arousal
![]() a rise in systolic and diastolic blood pressure (which may only be transient)
a rise in systolic and diastolic blood pressure (which may only be transient)
![]() general flushing of the skin
general flushing of the skin
![]() change in heart rate (either an increase or a decrease)
change in heart rate (either an increase or a decrease)
![]() respiratory changes
respiratory changes
![]() pupillary dilatation.
pupillary dilatation.
Plateau phase
Orgasm
In the male
In the female
In both sexes
Resolution
Refractory phase
The effect of age
Adolescence
The couple
Early parenthood
Middle age
Old age
The functions of sex
Reproduction
Physical Exercise
Pleasure
Pair-bonding
Asserting masculinity or femininity
Bolstering self-esteem
Achieving power
Reducing anxiety or tension
Material gain
History-taking
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree