Background
Women with a twin gestation are at increased risk for preterm birth (PTB), and sonographic cervical length (CL) is a powerful predictor for spontaneous PTB. Obstetricians frequently monitor CL in multiple gestations; yet, the optimal method to integrate and interpret the results of serial sonographic CL has not been determined.
Objective
We sought to determine whether there are different patterns of cervical shortening in twin gestations, and whether such patterns are related to the risk of PTB.
Study Design
We conducted a retrospective study of all women with twins followed up in a single tertiary referral center during 2012 through 2014. All women underwent serial measurements of CL every 2–3 weeks starting from 14–18 weeks and until 28–32 weeks of gestation. Changes in CL were analyzed and classified into distinct patterns that were initially identified by visual inspection of all individual cases. Each pattern was then characterized by several parameters including information about when cervical shortening began, the rate of shortening, and whether a plateau was observed. Locally weighted regression mean profiles were generated to describe each pattern of CL over time. The association of these patterns with spontaneous PTB was determined. The specific characteristics of each pattern that further determined the risk of PTB were identified using multivariable logistic regression analysis.
Results
We studied 441 women who had a total of 2826 measurements of CL done. Overall, 4 main patterns of change in CL were identified: pattern I, stable cervix (n = 196); pattern II, early and rapid shortening (n = 18); pattern III, late shortening (n = 109); and pattern IV, early shortening with a plateau (n = 118). The rate of PTB at <34 weeks was lowest in cases of pattern I (11.7%), followed by pattern IV (14.4%) and pattern III (20.2%), and was highest for women with pattern II (44.4%) ( P < .001). In cases with pattern III (late shortening), the most important factors affecting the risk of PTB were the shortening rate, the gestational age at the onset of cervical shortening, and the initial plateau of CL. In the case of pattern IV (early shortening with a plateau), it was only the new plateau at which cervical shortening stopped that was associated with the risk of PTB.
Conclusion
Changes in sonographic CL over time in twin gestations can be classified into 4 patterns, each associated with a different risk of PTB.
Introduction
Preterm birth (PTB) remains the main cause of neonatal mortality and morbidity in twin pregnancies. The rate of PTB <34 weeks of gestation is as high as 13% in twin pregnancies, compared with only 1% in singletons. The early prediction of PTB in twin pregnancies is of major importance as it may assist clinicians in identifying women with twin gestations who are at high risk of PTB and who may benefit from closer monitoring, administration of corticosteroids for fetal lung maturation, and other potential preventive interventions such as progesterone and cervical pessary.
Sonographic measurement of cervical length (CL) at midgestation has been shown to be predictive of PTB in singleton and twin gestations. This, in turn, has led to the relatively common practice of serial monitoring of CL during the second trimester in women at risk of PTB, including women with twin gestations. However, one question that needs to be answered before such practice becomes accepted into routine care relates to the optimal strategy for the integration and interpretation of the additional information derived from serial measurements of CL. One possible strategy for integrating and interpreting a series of measurements, which is used in the current study, is by classifying them into one of several recognized patterns.
The potential benefits of serial measurements of CL in twins has been addressed only by a few studies. Overall, most investigators have reported that serial measurements of CL do not improve the prediction of PTB. However, available studies have several limitations, including a small sample size and variability in the timing of CL measurement as well as the definition of cervical shortening. Furthermore, in most of these studies, the analysis of change in CL was restricted to only 2 sequential measurements of CL, so that data regarding the benefit and the interpretation and integration of multiple (>2) serial measurements of CL are lacking. Indeed, in a recent systematic review and metaanalysis on the predictive accuracy of changes in sonographic CL over time, Conde-Agudelo and Romero concluded that “the identification of distinct patterns of change in CL as a function of gestational age and the assessment of their predictive ability for PTB in women with singleton and twin gestations calls for further research.”
Thus, the aims of this study were to: (1) determine if there are distinct patterns of change in sonographic CL serially measured over time in twin gestations; and (2) examine the association between each pattern and PTB.
Materials and Methods
This was a retrospective study of all women with twin pregnancies followed up in the twins clinic in a single tertiary referral medical center from January 2012 through December 2014. Pregnancies complicated by any of the following conditions were excluded: <3 measurements of CL during gestation, cervical cerclage, uncertain pregnancy dating, indicated preterm delivery at <34 weeks for maternal or fetal indications, birthweight of either twin <500 g, gestational age at delivery <24 weeks, stillbirth of one or both fetuses, monoamniotic twins, monochorionic twins with twin-to-twin transfusion syndrome, or genetic or structural anomalies. The study was approved by the Sunnybrook Health Sciences Center Research Ethics Board.
All women were followed up by a single physician (J.B., a specialist in maternal-fetal medicine) during the study period. All women with twin pregnancies who were followed up in the twins clinic during the study period underwent routine transvaginal measurement of CL every 2–3 weeks starting from 14–18 weeks and until 28–32 weeks of gestation. In cases where there was evidence of cervical shortening, CL was monitored on a weekly basis. The decision regarding recommendation for bed rest, admission, or administration of antenatal corticosteroids for fetal lung maturation was made on an individual basis. Progesterone was not used in the management of women with twins and a short cervix given the lack of a primary randomized clinical trial of vaginal progesterone in women with a twin gestation and a short cervix. Cervical cerclage was considered and offered in selected cases of women with marked cervical shortening or cervical dilatation when it was thought that cervical insufficiency may have played a role. Since our hospital is a referral center for women with twin pregnancies, several women who lived relatively far from our center had some of their ultrasound scans done locally (ie, closer to their home), and in some cases the results of these scans were not always available to us.
All sonographic examinations were performed by experienced sonographers using a transvaginal approach. The measurement of CL was performed transvaginally after each patient had emptied her bladder and according to the standard technique. Briefly, the measurement of CL was performed in the sagittal plane, visualizing the full length of the endocervical canal from the internal to the external cervical os while exerting as little pressure with the transducer as possible. At least 3 measurements were obtained and the shortest measurement was recorded. The presence of cervical funneling or change in CL, either spontaneously or in response to fundal pressure, was routinely documented as well.
Data were extracted from the medical records and included demographic and obstetrical characteristics, chorionicity, validation of gestational age by first-trimester ultrasound, complications during pregnancy, use of cervical cerclage, gestational age at delivery, and neonatal characteristics. All the ultrasound reports throughout gestation were reviewed in detail for information on CL including the presence, shape, and length of cervical funneling, length of the closed part of the cervix, and change in CL in response to fundal pressure.
Changes in CL over time for each patient were plotted and, based on visual inspection (by the primary author, N.M.), 4 patterns were identified. It should be emphasized that we had no a priori hypothesis regarding the type of patterns. Each pattern was then characterized by several parameters including information about when cervical shortening began, the rate of shortening, and whether a plateau was observed. A computerized algorithm was developed (using Excel Visual Basic; Microsoft, Redmond, WA) that classified each individual trajectory of CL into 1 of the 4 patterns and calculated the characteristics of the pattern for each patient (more details regarding the algorithm are provided in Supplemental Figure 1 ). The classification accuracy of the trajectories derived from the application of the computerized algorithm (modeling) was confirmed by visual inspection of the CL trajectory over time for each patient, with the inspector being blinded to the pregnancy outcome. Locally weighted regression mean profiles were generated to describe each pattern of CL over time. The quantreg package under the R statistical environment ( https://www.r-project.org ) was used to fit locally weighted linear quantile regression models to estimate reference biomarker quantiles (ie, centiles) as a function of gestational age at measurement of CL.
Hypothesis testing was performed using software (SPSS, v21.0; IBM Corp, Armonk, NY). The χ 2 tests were used to compare proportions of PTB associated with each of the 4 patterns. Kaplan-Meier analysis was used to compare the survival distribution associated with each of the patterns. Cox proportional hazards regression models were used to examine magnitudes of association (hazard ratios with 95% confidence intervals) between CL patterns and PTB, with and without adjustment for the index CL measurement. Multivariable logistic regression analysis was used to determine which of the characteristics of each CL pattern are associated with the risk of PTB. Analysis of covariance was used to compare the slope of the regression lines representing the rate of cervical shortening in women who did or did not deliver prematurely. Results were considered significant when the P value was < .05.
Materials and Methods
This was a retrospective study of all women with twin pregnancies followed up in the twins clinic in a single tertiary referral medical center from January 2012 through December 2014. Pregnancies complicated by any of the following conditions were excluded: <3 measurements of CL during gestation, cervical cerclage, uncertain pregnancy dating, indicated preterm delivery at <34 weeks for maternal or fetal indications, birthweight of either twin <500 g, gestational age at delivery <24 weeks, stillbirth of one or both fetuses, monoamniotic twins, monochorionic twins with twin-to-twin transfusion syndrome, or genetic or structural anomalies. The study was approved by the Sunnybrook Health Sciences Center Research Ethics Board.
All women were followed up by a single physician (J.B., a specialist in maternal-fetal medicine) during the study period. All women with twin pregnancies who were followed up in the twins clinic during the study period underwent routine transvaginal measurement of CL every 2–3 weeks starting from 14–18 weeks and until 28–32 weeks of gestation. In cases where there was evidence of cervical shortening, CL was monitored on a weekly basis. The decision regarding recommendation for bed rest, admission, or administration of antenatal corticosteroids for fetal lung maturation was made on an individual basis. Progesterone was not used in the management of women with twins and a short cervix given the lack of a primary randomized clinical trial of vaginal progesterone in women with a twin gestation and a short cervix. Cervical cerclage was considered and offered in selected cases of women with marked cervical shortening or cervical dilatation when it was thought that cervical insufficiency may have played a role. Since our hospital is a referral center for women with twin pregnancies, several women who lived relatively far from our center had some of their ultrasound scans done locally (ie, closer to their home), and in some cases the results of these scans were not always available to us.
All sonographic examinations were performed by experienced sonographers using a transvaginal approach. The measurement of CL was performed transvaginally after each patient had emptied her bladder and according to the standard technique. Briefly, the measurement of CL was performed in the sagittal plane, visualizing the full length of the endocervical canal from the internal to the external cervical os while exerting as little pressure with the transducer as possible. At least 3 measurements were obtained and the shortest measurement was recorded. The presence of cervical funneling or change in CL, either spontaneously or in response to fundal pressure, was routinely documented as well.
Data were extracted from the medical records and included demographic and obstetrical characteristics, chorionicity, validation of gestational age by first-trimester ultrasound, complications during pregnancy, use of cervical cerclage, gestational age at delivery, and neonatal characteristics. All the ultrasound reports throughout gestation were reviewed in detail for information on CL including the presence, shape, and length of cervical funneling, length of the closed part of the cervix, and change in CL in response to fundal pressure.
Changes in CL over time for each patient were plotted and, based on visual inspection (by the primary author, N.M.), 4 patterns were identified. It should be emphasized that we had no a priori hypothesis regarding the type of patterns. Each pattern was then characterized by several parameters including information about when cervical shortening began, the rate of shortening, and whether a plateau was observed. A computerized algorithm was developed (using Excel Visual Basic; Microsoft, Redmond, WA) that classified each individual trajectory of CL into 1 of the 4 patterns and calculated the characteristics of the pattern for each patient (more details regarding the algorithm are provided in Supplemental Figure 1 ). The classification accuracy of the trajectories derived from the application of the computerized algorithm (modeling) was confirmed by visual inspection of the CL trajectory over time for each patient, with the inspector being blinded to the pregnancy outcome. Locally weighted regression mean profiles were generated to describe each pattern of CL over time. The quantreg package under the R statistical environment ( https://www.r-project.org ) was used to fit locally weighted linear quantile regression models to estimate reference biomarker quantiles (ie, centiles) as a function of gestational age at measurement of CL.
Hypothesis testing was performed using software (SPSS, v21.0; IBM Corp, Armonk, NY). The χ 2 tests were used to compare proportions of PTB associated with each of the 4 patterns. Kaplan-Meier analysis was used to compare the survival distribution associated with each of the patterns. Cox proportional hazards regression models were used to examine magnitudes of association (hazard ratios with 95% confidence intervals) between CL patterns and PTB, with and without adjustment for the index CL measurement. Multivariable logistic regression analysis was used to determine which of the characteristics of each CL pattern are associated with the risk of PTB. Analysis of covariance was used to compare the slope of the regression lines representing the rate of cervical shortening in women who did or did not deliver prematurely. Results were considered significant when the P value was < .05.
Results
Characteristics of study population
We studied 441 women with twin pregnancies who were eligible for the study and had 2826 measurements of CL done ( Table 1 ). Eighteen women who had a cervical cerclage were excluded from the analysis. Women in the study group had a median number of 6 CL measurements along gestation. The rates of PTB at <36 weeks, <34 weeks, <32 weeks, and <30 weeks were 41.7%, 15.9%, 7.9%, and 3.6%, respectively.
| Characteristic, N = 441 | Value |
|---|---|
| Maternal age, y | 32.9 ± 4.1 |
| Nulliparity | 270 (61.2) |
| History of preterm birth | 6 (1.4) |
| Chorionicity | |
| Dichorionic/diamniotic | 358 (81.2) |
| Monochorionic/diamniotic | 83 (18.8) |
| No. of cervical length measurements | 6 (5–8) |
| Gestational age at delivery, wk | 35.4 ± 2.4 |
| <36 a | 184 (41.7) |
| <34 a | 70 (15.9) |
| <32 a | 35 (7.9) |
| <30 a | 16 (3.6) |
| Birthweight, g | |
| Twin A | 2389 ± 552 |
| Twin B | 2335 ± 563 |
| Male sex | |
| Twin A | 192 (43.5) |
| Twin B | 220 (49.9) |
a Refers to preterm births at all gestational ages below this threshold.
Change in CL along gestation
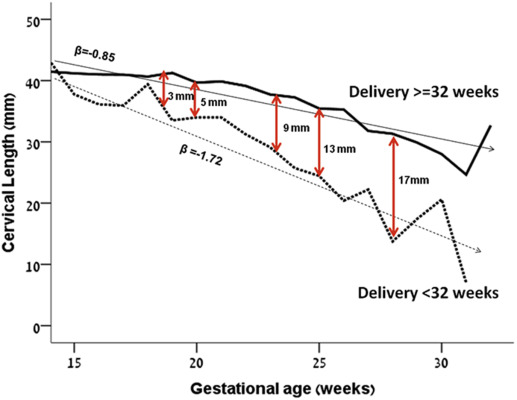
As the first step in determining whether the information obtained from serial CL measurements could identify women at risk for PTB, the mean CL as a function of gestational age was compared between women who did or did not deliver <32 weeks of gestation ( Figure 1 ; similar analysis was performed for PTB <30 weeks and <34 weeks, data not shown). While the differences in CL between the 2 groups were relatively small at ≤20 weeks of gestation (5 mm), these differences became larger at more advanced gestational ages ( Figure 1 ). In addition, the slope of the regression line representing the change in CL with gestational age in women who gave birth <32 weeks was significantly larger than that of women who did not ( P < .001) ( Figure 1 ). These findings imply that the information obtained from serial measurements of CL in twins can identify women who are more likely to deliver prematurely.
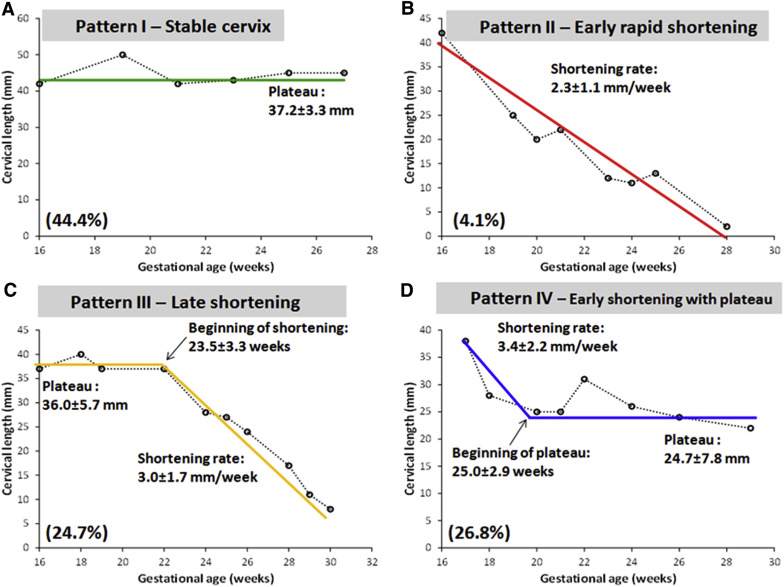
Patterns of change in sonographic CL as a function of time
Overall, 4 distinct patterns of change in CL along gestation were identified and are presented in a schematic manner in Figure 2 : (1) pattern I (stable cervix, n = 196 [44.4% of women]) ( Figure 2 , A), where the cervix remained long and stable until at least mid-third trimester; (2) pattern II (early and rapid shortening, n = 18 [4.1% of women]) ( Figure 2 , B), where there was a persistent shortening of CL starting from early second trimester at an average rate of 2.3 ± 1.1 mm/wk; (3) pattern III (late shortening, n = 109 [24.7% of women]) ( Figure 2 , C), where the onset of cervical shortening was noted toward late second trimester (mean gestational age of 23.5 ± 3.3 weeks); and (4) pattern IV (early shortening with a plateau, n = 118 [26.8% of women]) ( Figure 2 , D), where there was an early onset of shortening of CL (mean rate of 3.4 ± 2.2 mm/wk) until reaching a new plateau (of 24.7 ± 7.8 mm at a mean gestational age of 25.0 ± 2.9 weeks). In most cases, the pattern could be determined for each patient by 26–28 weeks of gestation.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


