Sensorineural Hearing Loss in A Child
Bernadette L. Koch, MD
DIFFERENTIAL DIAGNOSIS
Common
Large Endolymphatic Sac Anomaly (IP-2)
Fractures, Temporal Bone
Semicircular Canal Dysplasia
Labyrinthine Ossificans
Less Common
Labyrinthitis
Cochlear Nerve Deficiency
Cystic Cochleovestibular Anomaly (IP-1)
Lipoma, CPA-IAC
Rare but Important
Common Cavity, Inner Ear
Cochlear Aplasia, Inner Ear
Labyrinthine Aplasia
Vestibular Schwannoma
Schwannoma, Facial Nerve, CPA-IAC
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
History is important
In setting of fluctuating or “cascading” sensorineural hearing loss (SNHL) in child who could hear at birth (without history of meningitis)
Look for large vestibular aqueduct ± cochlear dysplasia and modiolar deficiency on CT
Look for enlarged endolymphatic sac and duct with cochlear dysplasia and modiolar deficiency on MR
Trauma: Look for fracture involving inner ear structures ± pneumolabyrinth on CT
Genetic disorders: In CHARGE, Alagille, Waardenburg, Crouzon or Apert syndrome, look for semicircular canal (SCC) dysplasia
Prior meningitis
Look for labyrinthine ossificans on CT
Look for enhancement or replacement of high T2 intensity with low T2 intensity within structures of membranous labyrinth on MR (depends on timing of imaging)
Best imaging tool
Thin-section T-bone CT identifies many congenital inner ear anomalies
High-resolution T2 MR imaging identifies large endolymphatic sac, cochlear dysplasia; best to show cochlear nerve aplasia/hypoplasia
Contrast MR best evaluates schwannoma, acute labyrinthitis, and lipoma
Helpful Clues for Common Diagnoses
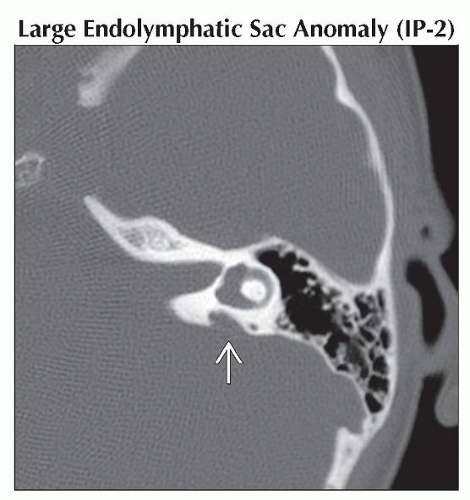
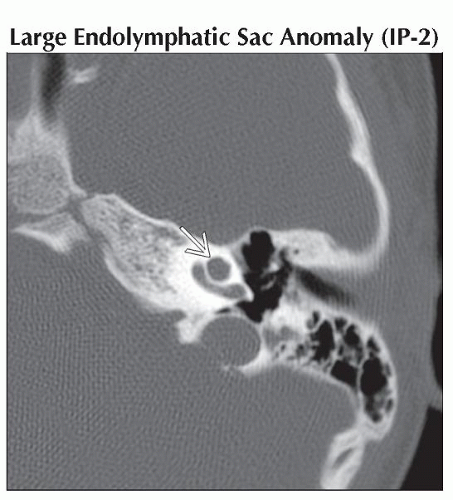
Large Endolymphatic Sac Anomaly (IP-2)
Most common congenital anomaly of inner ear found by imaging
Vestibular aqueduct on CT ≥ 1.5 mm bony transverse dimension
Newer literature suggests ≥ 2 mm at operculum or ≥ 1 mm at midpoint
Look for associated cochlear dysplasia, modiolar deficiency, vestibule &/or SCC dysplasia
Additional diagnosis information
Avoidance of contact sports or other activities that may lead to head trauma is recommended in children with IP-2 anomaly
Genetic testing for Pendred syndrome is becoming increasingly recommended in children with IP-2 anomaly
Up to 15% of all patients with IP-2 will have Pendrin gene = Pendred syndrome, with severe profound bilateral SNHL; 50% with goiter and 50% of those with goiter, will be hypothyroid
Fractures, Temporal Bone
Thin-section T-bone CT (0.625-1 mm)
Transverse or longitudinal fracture may cross inner ear structures, ± pneumolabyrinth
Semicircular Canal Dysplasia
Spectrum of abnormalities: 1 or more of SCC dysmorphic, hypoplastic, or aplastic
Unilateral or bilateral: Bilateral more common in syndromic form
Most common is short, dilated lateral SCC and vestibule forming single cavity
Look for associated cochlear dysplasia, oval window atresia, and ossicular anomalies
CHARGE syndrome
Bilateral absence of all SCCs
Associated anomalies: Small vestibule, absent cochlear nerve aperture (“isolated cochlea”), oval window atresia (± overlying tympanic segment of CN7), choanal atresia, coloboma
Lateral SCC last to form embryologically, therefore if lateral SSC is normal, posterior superior should be normal
Except if obliterated by labyrinthine ossificans or hypoplastic in Waardenburg and Alagille syndrome
Labyrinthine Ossificans
Synonyms: Labyrinthitis ossificans, labyrinthine ossification, chronic labyrinthitis, ossifying labyrinthitis
Acute inflammatory response results in fibrous and then osseous replacement of membranous labyrinth
May involve cochlea ± vestibule ± semicircular canals
Bilateral in meningogenic form (meningitis) and in hematogenic form (blood-borne infections)
Unilateral in tympanogenic form (middle ear infection)
T-bone CT: High-attenuation bone deposition in formerly fluid-filled membranous labyrinth
T2 MR: Focal or diffuse low intensity replaces high intensity fluid, with apparent “enlargement” of modiolus if cochlea is involved
T1 C+: Enhancement of involved membranous labyrinth structures in early stage, may persist into ossifying stages
Helpful Clues for Less Common Diagnoses
Labyrinthitis
Subacute inflammation of fluid-filled inner ear structures
T-bone CT: Normal in early phases, may progress to labyrinthine ossificans
T2 MR: Low intensity replaces normal fluid signal within membranous labyrinth structures
T1 C+: Mild to moderate enhancement
Cochlear Nerve Deficiency
Very small or absent cochlear nerve with small IAC
Cystic Cochleovestibular Anomaly (IP-1)
Cochlea and vestibule form bilobed cyst
Lipoma, CPA-IAC
Fatty lesion of CPA, IAC ± inner ear
Helpful Clues for Rare Diagnoses
Common Cavity, Inner Ear
Cystic cochlea and vestibule form a common cavity ± SCC absence or dysplasia
Cochlear Aplasia, Inner Ear
Absent cochlea
Labyrinthine Aplasia
Absent membranous labyrinth
Vestibular Schwannoma
Enhancing lesion ± cysts in CPA-IAC
Rare in children
Schwannoma, Facial Nerve, CPA-IAC
Enlarged labyrinthine segment CN7 canal with enhancing tubular mass in CPA-IAC and labyrinthine segment of CN7
Rare in children
Image Gallery
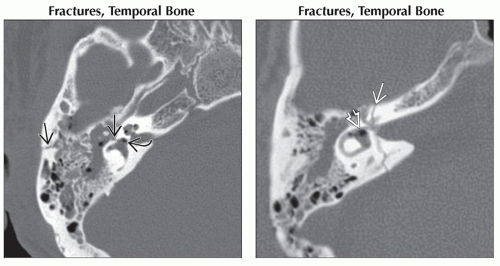 (Left) Axial bone CT shows a longitudinal temporal bone fracture
 with associated pneumolabyrinth with associated pneumolabyrinth  . (Right) Coronal oblique bone CT shows a transverse temporal bone fracture . (Right) Coronal oblique bone CT shows a transverse temporal bone fracture  with associated pneumolabyrinth and gas in the vestibule with associated pneumolabyrinth and gas in the vestibule  and lateral semicircular canal. and lateral semicircular canal.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|