Rubella
Maria Jevitz Patterson
Rubella (German measles) is no longer endemic in the United States. Because of its worldwide distribution, imported cases continue to occur, although these sporadic cases do not result in sustained transmission.1,2 Rubella is usually a minor illness in adults. Of major significance, however, is the high incidence of a constellation of congenital defects in children whose mothers are infected during early pregnancy. Typical anomalies, known collectively as the congenital rubella syndrome (CRS), include hearing impairment, cardiac defects, cataracts, and developmental delay.
 PATHOPHYSIOLOGY
PATHOPHYSIOLOGY
Rubella is a member of the Togaviridae family with an approximately 10-kb single-stranded, positive-sense polyadenylated RNA genome and a lipid envelope. Currently, standardized nomenclature for wild-type and vaccine rubella viruses describes 2 clades, 9 recognized genotypes, and 4 provisional genotypes.4 The virion is roughly spherical, 60 to 70 nm in diameter, with an icosahedral nucleocapsid composed of multiple copies of a single virus-specified structural capsid protein (C) that is covered by a lipid envelope in which 2 virus-specified structural glycoproteins (E1 and E2) are embedded. E1 appears to function in attachment, fusion, hemagglutination, and neutralization.
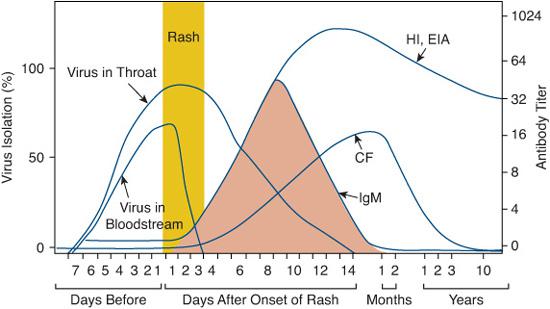
Humans are the only natural host. Direct person-to-person airborne spread by infected droplets appears to be the usual mode of transmission. The patient with subclinical infection is also a source of rubella virus. Patients are most contagious for a few days before and after the onset of rash, although virus may be present in pharyngeal secretions for as long as 1 week before and 2 weeks after the onset of rash (Fig. 320-1). Prolonged shedding occurs only in patients with congenital rubella syndrome, not when acquired postna-tally; infants may remain contagious for months after birth.
 EPIDEMIOLOGY
EPIDEMIOLOGY
Although rubella occurs in all areas of the world, epidemiologic patterns vary from country to country. Mathematic modeling predicts that elimination of transmission requires approximately 90% immunity among children.5,6 Prior to widespread use of rubella vaccines in the United States, when 85% of the population was immune, rubella occurred primarily in children during the elementary school years. A small minority did not become infected until early adulthood.

FIGURE 320-1. Rubella. The rash consists of erythematous macules and papules that appear initially on the face and spread inferiorly to the trunk and extremities, usually within the first 24 hours. (From Wolff K, Johnson RA. Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill; 2009.)
Following licensure of the first vaccine in 1969 until 1989, the reported incidence of rubella declined more than 99% in the United States (eFig. 320.1  ). Since 2001, annual reported rubella cases (< 25) and congenital rubella cases (< 4) declined further.7 Beginning with the 2005–2006 school year, all 50 states required and enforced the second dose of measles-mumps-rubella (MMR) vaccine for school entry.5,10
). Since 2001, annual reported rubella cases (< 25) and congenital rubella cases (< 4) declined further.7 Beginning with the 2005–2006 school year, all 50 states required and enforced the second dose of measles-mumps-rubella (MMR) vaccine for school entry.5,10
Outbreaks during the years of changing epidemiology were confined essentially to unimmunized populations, religious communities that traditionally decline vaccination, settings in which young adults congregate, and among specific racial/ethnic groups from countries where rubella vaccine is not routinely used. Many countries have yet to achieve good rubella vaccination rates. By 2006, 75% of children globally still lived in countries without national policies for rubella vaccination,11 with an estimate of more than 100,000 infants born with congenital rubella syndrome annually.12
POSTNATAL RUBELLA
 CLINICAL MANIFESTATIONS
CLINICAL MANIFESTATIONS
The clinical manifestations of postnatal rubella range from inapparent infection to a characteristic pattern of adenopathy, rash, and low-grade fever. The incubation period is from 14 to 21 days. Primary replication occurs in the nasopharynx, followed by viremia at approximately days 5–7 and rash at days 14–17 (Fig. 320-1). A typical clinical course begins with adenopathy involving primarily the postauricular, occipital, and posterior cervical nodes, which may be slightly painful and tender. Although symptoms usually clear promptly as the rash fades, nodes may remain palpable for several weeks. Adolescents and adults may complain of malaise, headache, a low-grade fever, sore throat, and mild coryza during a 1-day to 5-day prodromal period that frequently accompanies the onset of adenopathy.
The rubella rash is variable but usually brief. It may be no more than a transient blush, but classically it persists for 2 to 3 days in a pattern that has been called kaleidoscopic because of its changing appearance. Initially, small, irregular pink macules begin on the face and spread rapidly (usually within 24 hours) to the neck, trunk, arms, and ultimately legs. By the next day, these lesions may have coalesced, developed a maculopapular component, and become scarlatiniform.
An exanthema consisting of punctate or slightly larger red spots on the soft palate may be present during the late prodrome and early rash phase.
Fever is uncommonly as high as 39°C (102.2°F) to 39.5°C (103.1°F), but may be absent in children. Polyarthralgia and polyarthritis are common manifestations of rubella among women, less common in men, and uncommon in children.  Joint symptoms are also associated with rubella vaccine, particularly in postpubertal females of HLA-DR2 and HLA-DR5 type.15 However, no causal relationship between vaccine and persistent joint symptoms has been validated.16
Joint symptoms are also associated with rubella vaccine, particularly in postpubertal females of HLA-DR2 and HLA-DR5 type.15 However, no causal relationship between vaccine and persistent joint symptoms has been validated.16
Postinfectious encephalitis, clinically indistinguishable from that following measles or varicella, is a rare complication of rubella that occurs less frequently than postmeasles encephalitis. Symptoms and signs of central nervous system involvement usually develop 2 to 4 days after onset of rash.
Many patients have slight transient decrease in platelet count during the course of uncomplicated rubella. Prognosis is generally excellent. Thrombocytopenia may sometimes be prolonged for 1 to 2 weeks.
 DIAGNOSIS
DIAGNOSIS
Diagnosis of rubelliform rashes in acutely ill, febrile children and in young adults requires accurate historical information from parents: vaccine history, source of exposure, prodrome, and progression of rash. Other childhood exanthems, as well as the possibility of primary vaccine failure should be considered.18 Clinical diagnosis is unreliable. Laboratory testing is required. Rubella can be diagnosed by isolating the virus, detecting viral nucleic acid by polymerase chain reaction or demonstrating rising titers of rubella antibody in serum (Fig. 320-2).19
Rubella serum antibody is measured in a variety of test systems based on neutralization, hemagglutination inhibition, complement fixation, latex agglutination, radial hemolysis, immunoblot, enzyme immunoassay (EIA), and IgG avidity. Interpretation of antibody testing should always be guided by clinical, epidemiological, and immunization status data.
Hemagglutination inhibition (HI), previously the serologic standard, has been replaced by EIA that detects antibody to viral proteins E1, E2, and C, while HI detects antibody only to E1. In patients with clinical rubella, rubella-specific IgM HI and EIA antibodies are detectable within 24 to 48 hours after onset of the rash. The patterns of rubella-specific IgM HI, CF, and EIA responses during rubella are also illustrated in Figure 320-2.
The presence of antibody at exposure confirms past rubella infection (or rubella vaccination), indicates protection from another episode of the disease, and in the pregnant woman obviates rubella-induced congenital malformation. Although no antibody titer is absolutely correlated with protection,22 absence of rubella hemagglutination inhibition or enzyme immunoassay (EIA) antibodies (<10 IU) at the time of exposure indicates susceptibility to rubella. National seropositive rates (1999–2004) showed immunity sufficient to interrupt transmission (children, 96.2%; adolescents, 93.7%; adult women, 91.5%; adult men, 88%).11 However, nearly 10% of women lacked protective antibody to prevent congenital rubella syndrome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


