(1)
Division of Urology, Department of Surgery, University of Chicago Medicine and Biological Sciences Division, Chicago, IL, USA
(2)
Comer Children’s Hospital, University of Chicago, Chicago, IL, USA
Abstract
The robotic platform has helped to bridge the gap between open and conventional laparoscopic surgery and has allowed the surgeons to overcome the difficulties of intricate suturing, tissue handling, and learning curve. Robotic pyeloplasty is the commonest procedure performed in the realm of robotic pediatric urology among the others like ureteric reimplantation, heminephrectomy, appendicovesicostomy, and cystoplasty. The key steps for successful completion are case selection, positioning, and port placement. Use of the UPJ as handle facilitates the anastomosis without much handling of the ureter during the anastomosis. The placement of cutaneous pyeloureteral (C-PU) stent avoids the second anesthesia for removal and does not have associated bleeding during placement, as experienced with nephroureteral stent. The outcomes are equivalent compared to open approach and have reduced morbidity. The system in its current stage is not tailored to meet the demands and requirements of pediatric application and requires further refinements and miniaturization.
The online version of this chapter (doi:10.1007/978-1-4471-5394-8_8) contains supplementary material, which is available to authorized users.
Keywords
PyeloplastyRoboticPediatricStentUPJIntroduction
Since the first description of laparoscopic pyeloplasty about two decades ago, only select surgeons were able to perform this procedure, due to complexity of suturing and time invested to master these skills [1]. The robotic platform with its inherent 7-degree freedom of movement and three-dimensional vision had bridged the gap between laparoscopic and open surgery for reconstructive procedures like pyeloplasty, with similar success. Robotic pyeloplasty is the commonest procedure performed in the realm of robotic pediatric urology among the others like ureteric reimplantation, heminephrectomy, appendicovesicostomy, and cystoplasty [2].
Preoperative Workup
The preoperative imaging is similar to open surgical approach in the form of USS scan and MAG-3 radioisotope diuretic renal scan. In the author’s experience, there is no need for a retrograde pyelogram at the time of surgery except in horseshoe kidney, ectopic kidney, and redopyeloplasty. Bowel preparation is unnecessary, often a dilated colon is encountered during procedure in infants, and intraoperative insertion of a flatus tube will help to deflate the colon. MR angiogram is often useful for horseshoe kidney pyeloplasty for delineation of the aberrant renal vessels [3]. A thorough preoperative counseling with families about the procedure outcome, complications, and explaining pros and cons of the approach is mandatory.
Case Selection
In the author’s experience, it is ideal to begin initially with patients older than 5 years, and as the experience builds on, then the age could be lowered (infants) and even extended to anomalous kidneys (e.g., horseshoe and ectopic) and reoperative cases. Currently the author offers this approach to all patients requiring pyeloplasty above the age of 2 months. Most important is that the operative indication should not change from an open procedure.
Approaches
Retroperitoneal approach is standard for open surgical reconstruction of renal anomalies including dismembered Anderson-Hynes pyeloplasty for UPJ. The inherent advantage of this confined space is if there is a urine leak, it will be contained and avoids the paralytic ileus. Unfortunately due to restriction of the endoscopic movements in this confined space, it has been never popular and transperitoneal approach remains standard. To date, there is only one report of robotic pediatric pyeloplasty with retroperitoneal approach [4]. Transmesocolic approach may be feasible for a left side, while liver retraction is required for a right side pyeloplasty.
Patient Positioning
This is a key step for successful completion and preventing external pressure injuries during the surgical procedure. Diligent attention is required, especially in infants. Intraoperative orogastric tube and Foley catheter are placed to keep the stomach and bladder decompressed, facilitating the port placement.
All pressure points are well padded, and the patient is brought to the edge of the bed and positioned 30–45-° lateral decubitus position with ipsilateral side raised. The table is flexed approximately 15°, and a bean bag is placed underneath and well secured at the level of the nipple and iliac crest with silk tape. The ipsilateral arm rests comfortably on the patient’s side in the natural anatomical position, whereas the contralateral arm rests outstretched supported by a bedside attachment limb support. Large foam padding is placed on the head protecting the airway and face in the case of camera approximation during operation (Fig. 8.1).
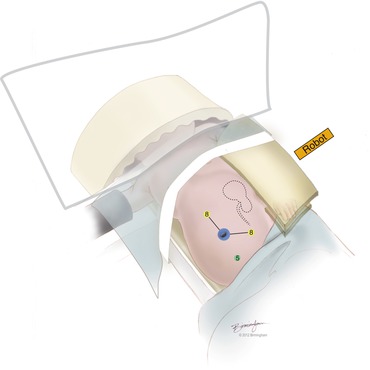
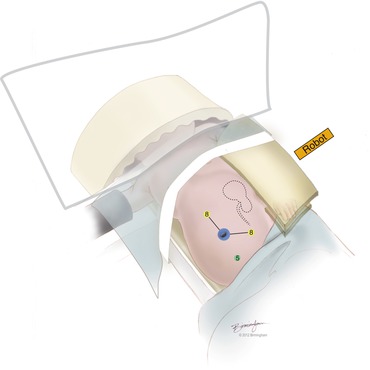
Fig. 8.1
Positioning and port placement for left robotic pyeloplasty
Port Placement
This is the next key step in proceeding with successful completion of the procedure. The preferred approach for initial insufflation is with the open Hasson’s technique. The camera port (12 mm/8.5 mm) is first placed at umbilicus with this approach. Initial insufflation is set to 12–15 mmHg of carbon dioxide; however, this may be variable based on the age of the patient, with lower pressures (10–12) for younger patients.
Two 8 mm working ports are generally used during operation. These ports are placed after pneumoperitoneum is achieved, and under direct vision with a 30° upward-facing camera or 0° degree lens is used. The left port is placed in midline 6–8 cm superior to the umbilicus, while right port is placed about 6–8 cm away from the umbilicus in ipsilateral midclavicular line. In the author’s experience, an additional 5 mm assistant port facilitates the procedure and is placed in the midline at suprapubic level (Fig. 8.1). Adequate spacing (6–8 cm) between ports and the camera is critical to prevent collision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


