Background
Previous studies have demonstrated an association between mental illness and preterm birth (before 37 weeks). However, these investigations have not simultaneously considered gestation of preterm birth, the indication (eg, spontaneous or medically indicated), and specific mental illness classifications.
Objective
The objective of the study was to examine the likelihood of preterm birth across gestational lengths and indications among Medi-Cal (California’s Medicaid program) participants with a diagnostic code for mental illness. Mental illnesses were studied by specific illness classification.
Study Design
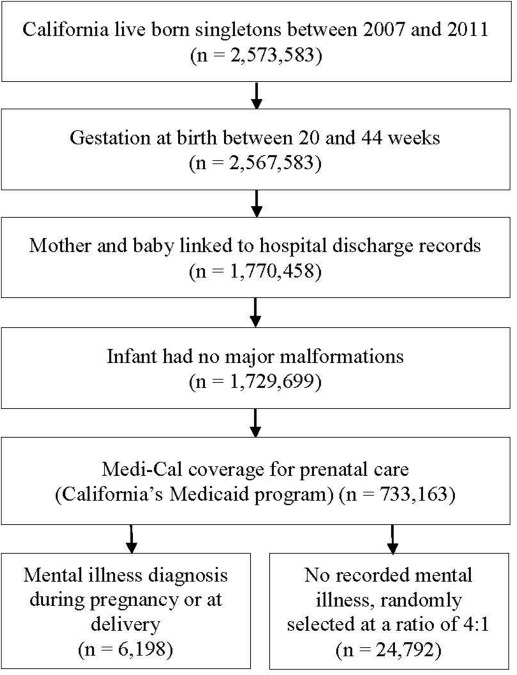
The study population was drawn from singleton live births in California from 2007 through 2011 in the birth cohort file maintained by the California Office of Statewide Health Planning and Development, which includes birth certificate and hospital discharge records. The sample was restricted to women with Medi-Cal coverage for prenatal care. Women with mental illness were identified using International Classification of Diseases , ninth revision, codes from their hospital discharge record. Women without a mental illness International Classification of Diseases , ninth revision, code were randomly selected at a 4:1 ratio. Adjusting for maternal characteristics and obstetric complications, relative risks and 95% confidence intervals were calculated for preterm birth comparing women with a mental illness diagnostic code with women without such a code.
Results
We identified 6198 women with a mental illness diagnostic code and selected 24,792 women with no such code. The risk of preterm birth in women with a mental illness were 1.2 times higher than women without a mental illness (adjusted relative risk, 1.2, 95% confidence interval, 1.1–1.3). Among the specific mental illnesses, schizophrenia, major depression, and personality disorders had the strongest associations with preterm birth (adjusted relative risks, 2.0, 2.0 and 3.3, respectively).
Conclusion
Women receiving prenatal care through California’s low-income health insurance who had at least 1 mental illness diagnostic code were 1.2–3.3-times more likely to have a preterm birth than women without a mental illness, and these risks persisted across most illness classifications. Although it cannot be determined from these data whether specific treatments for mental illness contribute to the observed associations, elevated risk across different diagnoses suggests that some aspects of mental illness itself may confer risk.
Mental illness is common during pregnancy: an estimated 14–23% of pregnant women suffer from a depressive disorder, and 3–5% of have major depressive disorder. Approximately 13% of pregnant women in the United States suffer from an anxiety disorder. Studying birth outcomes of women with a mental illness remains challenging because of the range of primary and comorbid mental disorders, different types of medication used as treatments, the duration of medication use during pregnancy, and associated confounding factors such as smoking and substance abuse.
Previous studies have demonstrated an association between mental illness and preterm birth (before 37 weeks’ gestation); however, few have examined more than 1 psychiatric diagnosis in a cohort. Recent large studies have demonstrated that women with depression are at a slightly increased risk of premature delivery, and small studies have suggested an association between bipolar and schizophrenic disorders and preterm birth.
A large Canadian study demonstrated that women with major depression or bipolar disorder were not only at increased risk of birth before 37 weeks but also birth before 32 weeks’ gestation. Mannisto et al examined both mental illness subtype and timing of delivery and demonstrated that women with depression, anxiety, or bipolar disorder were more likely to delivery before 37 weeks. No previous investigations, to our knowledge, have considered in totality gestation of preterm birth, the indication for preterm birth (eg, spontaneous or medically indicated), and mental illness classifications.
In this study, we estimated the risk of preterm birth across gestational lengths and indications for women with a diagnostic code for mental illness. Mental illnesses were studied by specific illness classification. We hypothesized that women with mental illness would be at increased risk of preterm birth and that risk would differ by gestation at delivery and mental illness classifications. In an attempt to assure equal access to medical care, we restricted our sample to women covered by Medi-Cal (California’s Medicaid program) for prenatal care.
Materials and Methods
In this retrospective cohort study, our sample was drawn from all California live-born singletons between Jan. 1, 2007, and Dec. 31, 2011 (n = 2,573,583). The sample was restricted to singleton births with gestations between 20 and 44 weeks linked to a hospital discharge database maintained by the California Office of Statewide Health Planning and Development (n = 1,770,458). This database contains linked birth and death certificates as well as detailed information on maternal and infant characteristics, hospital discharge diagnoses, and procedures recorded as early as 1 year prior to delivery and as late as 1 year after delivery.
Data files provided diagnoses and procedure codes based on the International Classification of Diseases , ninth revision, Clinical Modification. The study sample was further restricted to infants without chromosomal abnormalities or major structural birth defects (n = 1,729,699) because congenital abnormalities have been associated with both mental illness and indication of preterm birth. Structural birth defects for the study were considered major if determined by clinical review as causing major morbidity and mortality that would likely be identified in the hospital at birth or lead to hospitalization during the first year of life.
Our study protocols required that major structural birth defects be identified by their 4 digit International Classification of Diseases , ninth revision, codes because all hospitals in the state reported 4 digit International Classification of Diseases , ninth revision, diagnostic codes, but not all reported to 5 or 6 digit International Classification of Diseases , ninth revision, diagnostic codes.
In an effort to ensure equal access to medical care, we restricted our sample to women covered by Medi-Cal, California’s Medicaid program (n = 733,163). Exposed women were defined as women with an International Classification of Diseases , ninth revision, code for mental illness in their hospital admission for delivery. Mental illnesses were subgrouped into the following categories:
- •
Schizophrenic disorders: International Classification of Diseases , ninth revision, 295 schizophrenic disorders.
- •
Bipolar disorder: International Classification of Diseases , ninth revision, codes 296.0, bipolar I disorder, single manic episode; 296.1, manic disorder, recurrent episode; 296.4, bipolar I disorder, most recent episode (or current) manic; 296.5, bipolar I disorder, most recent episode (or current) depressed; 296.6, bipolar I disorder, most recent episode (or current) mixed; 296.7, bipolar I disorder, most recent episode (or current) unspecified; 296.8, other and unspecified bipolar disorders; 296.9, other and unspecified episodic mood disorder.
- •
Major depression: International Classification of Diseases , ninth revision, codes 296.2, major depressive disorder, single episode; 296.3, major depressive disorder, recurrent episode.
- •
Depressive disorder, not otherwise specified: International Classification of Diseases , ninth revision, code 311, depressive disorder not otherwise specified.
- •
Anxiety disorders: International Classification of Diseases , ninth revision, code 300, anxiety, dissociative, and somatoform disorders.
- •
Personality disorders: International Classification of Diseases , ninth revision, code 301, personality disorders.
- •
Any of the previously mentioned categories.
- •
More than 1 of the previously mentioned categories.
Women without a recorded mental illness were randomly selected at a ratio of 4:1 ( Figure 1 ). This ratio was selected to maximize the precision of our findings. No recorded mental illness included none of the previously mentioned categories of diagnoses in addition to no record of the following:
- •
Other mental illnesses: International Classification of Diseases , ninth revision, codes 290, dementias; 291, alcohol-induced mental disorders; 292, drug-induced mental disorders; 293, transient mental disorders caused by conditions classified elsewhere; 294, persistent mental disorders caused by conditions classified elsewhere; 297, delusional disorders; 298, other nonorganic psychoses; 299, pervasive developmental disorders; 302, sexual and gender identity disorders; 306, physiological malfunction arising from mental factors; 307, special symptoms or syndromes, not elsewhere classified; 308, acute reaction to stress; 309, adjustment reaction; 310, specific nonpsychotic mental disorders caused by brain damage; 312, disturbance of conduct, not elsewhere classified; 313, disturbance of emotions specific to childhood and adolescence; 314, hyperkinetic syndrome of childhood; 315, specific delays in development; 316, psychic factors associated with diseases classified elsewhere.
- •
International Classification of Diseases , ninth revision, code 648.4, mental disorders complicating pregnancy, childbirth, or the puerperium.
Because of the lack of specificity, we did not include these diagnoses in our population with mental illnesses.
Maternal characteristics for women with mental illness were compared with women without recorded mental illness using crude Poisson logistic regression to calculate relative risks and 95% confidence intervals. Potential confounders were selected from birth certificate records and included the following information: year of birth, race or ethnicity, maternal age at term, parity, prepregnancy body mass index (calculated from prepregnancy weight and height), maternal education, participation in the Women, Infants, and Children program, status of smoking during pregnancy, and previous preterm birth.
Additional factors selected from hospital discharge International Classification of Diseases , ninth revision, diagnoses noted by the coding hospital as complicating pregnancy included the following: hypertensive disorder ( International Classification of Diseases , ninth revision, code 642, hypertension complicating pregnancy, childbirth, and the puerperium); infection ( International Classification of Diseases , ninth revision, code 646.6, infections of genitourinary tract in pregnancy; code 647, infectious and parasitic conditions in the mother classifiable elsewhere but complicating pregnancy, childbirth, or the puerperium); and drug or alcohol dependence ( International Classification of Diseases , ninth revision, codes 648.3, drug dependence; 303, alcohol dependence syndrome; 304, drug dependence; and 305, nondependent abuse of drugs).
The best obstetric estimate of gestation at birth was obtained from birth certificate records. Preterm birth (before 37 weeks’ gestation) was grouped into premature rupture of the membranes, spontaneous labor with intact membranes, and medically indicated. As previously described, all pregnancies with an indication of premature rupture of the membranes in the infant’s birth certificate or mother’s hospital discharge records were included in the premature rupture of the membranes group.
Women with no indication of premature rupture of the membranes but had birth certificate or hospital discharge records indication of premature labor or tocolytic medication were included in the spontaneous labor with intact membrane group. Pregnancies resulting in medically indicated birth were considered to be those without premature rupture of the membranes, premature labor, or tocolytic administration for which there was a code for medical induction or artificial rupture of membranes, or for which there was a cesarean delivery without any of the aforementioned codes.
Risk of preterm birth (crude and adjusted), overall and by illness classification, for women with mental illness were compared with women without mental illness using Poisson logistic regression to calculate relative risks and 95% confidence intervals (because of the rare occurrence of preterm birth and the subtypes).
All analyses were performed using Statistical Analysis Software version 9.3 (SAS Inc, Cary, NC). Methods and protocols for the study were approved by the Committee for the Protection of Human Subjects within the Health and Human Services Agency of the State of California.
Results
We identified 6198 women with a mental illness diagnostic code during pregnancy and randomly selected 24,792 women without a documented mental illness. Approximately half of the women with a mental illness had a depressive disorder, whereas 24.5% had an anxiety disorder and 6.6% had more than 1 documented illness ( Supplemental Table ). Only 56 (0.9%) had a personality disorder.
Women with and without mental illness differed statistically on all maternal characteristics and obstetric complications we investigated except overweight body mass index. Women with a mental illness were more likely to be white, obese, and older than women without mental illness. Additionally, they were more educated and more likely to have had a previous preterm birth than women without mental illness. Women with a mental illness were also 2.8 times as likely to have smoked and 4.5 times as likely to have abused drugs or alcohol during pregnancy ( Table 1 ).
| Characteristic | No mental illness n, % | Any mental illness n, % | RR (95% CI) |
|---|---|---|---|
| Sample year of birth | 24,792 | 6198 | |
| 2007 | 5440 (21.9) | 1030 (16.6) | 0.6 (0.6–0.7) a |
| 2008 | 5235 (21.1) | 1104 (17.8) | 0.7 (0.6–0.7) a |
| 2009 | 5002 (20.2) | 1215 (19.6) | 0.8 (0.7–0.8) a |
| 2010 | 4662 (18.8) | 1348 (21.8) | 0.9 (0.8–1.0) b |
| 2011 | 4453 (18.0) | 1501 (24.2) | Reference |
| Race/ethnicity | |||
| White non-Hispanic | 2310 (9.3) | 1971 (31.8) | Reference |
| Hispanic | 18,237 (73.6) | 3030 (48.9) | 0.3 (0.3–0.3) a |
| Black | 880 (3.6) | 371 (6.0) | 0.6 (0.6–0.7) a |
| Asian | 1669 (6.7) | 176 (2.8) | 0.2 (0.2–0.2) a |
| American Indian/Alaska Native | 144 (0.6) | 67 (1.1) | 0.7 (0.5–0.9) b |
| Hawaiian/Pacific Islander | 104 (0.4) | 19 (0.3) | 0.3 (0.2–0.5) a |
| Other race | 752 (3.0) | 123 (2.0) | 0.3 (0.3–0.4) a |
| Two or more races | 437 (1.8) | 281 (4.5) | 0.9 (0.8–1.0) c |
| Unknown | 259 (1.0) | 160 (2.6) | 0.8 (0.7–1.0) c |
| Maternal age at term, y | |||
| <18 | 1167 (4.7) | 182 (2.9) | 0.7 (0.6–0.8) a |
| 18–34 | 20,640 (83.3) | 4967 (80.1) | Reference |
| >34 | 2985 (12.0) | 1049 (16.9) | 1.3 (1.3–1.4) a |
| Body mass index | |||
| Underweight | 2290 (9.2) | 432 (7.0) | 0.8 (0.7–0.9) a |
| Normal | 10,038 (40.5) | 2391 (38.6) | Reference |
| Overweight | 6503 (26.2) | 1570 (25.3) | 1.0 (0.9–1.1) |
| Obese | 5961 (24.0) | 1805 (29.1) | 1.2 (1.1–1.3) a |
| Parity d | |||
| Nulliparous | 8689 (35.1) | 2073 (33.6) | 0.9 (0.9–1.0) c |
| Multiparous | 16,094 (64.9) | 4119 (66.5) | Reference |
| Maternal education, y e | |||
| <12 | 11,727 (47.3) | 2186 (35.3) | 0.8 (0.7–0.8) a |
| 12 | 7217 (29.1) | 1895 (30.6) | Reference |
| >12 | 4902 (19.8) | 1757 (28.4) | 1.3 (1.2–1.4) a |
| Mother enrolled in WIC f | 21,301 (85.9) | 4950 (79.9) | 0.7 (0.7–0.8) a |
| Smoked during pregnancy | 1058 (4.3) | 1056 (17.0) | 2.8 (2.6–3.0) a |
| Previous preterm birth | 90 (0.4) | 87 (1.4) | 2.4 (2.0–3.0) a |
| Hypertension during pregnancy | 1445 (5.8) | 660 (10.7) | 1.6 (1.5–1.8) a |
| Diabetes | 2022 (8.2) | 769 (12.4) | 1.4 (1.3–1.5) a |
| Infection during pregnancy | 665 (2.7) | 523 (8.4) | 2.3 (2.1–2.5) a |
| Drug or alcohol abuse | 23 (0.1) | 172 (2.8) | 4.5 (3.9–5.2) a |
d Parity missing for 15 women (6 with mental illness, 9 without)
e Education missing for 1306 women (360 with mental illness, 946 without)
f Women, Infants, and Children participation missing for 515 women (118 with mental illness, 397 without).
Women with a mental illness were at increased risk of preterm birth. When adjusting for maternal characteristics and obstetric factors, relative risks were consistently lower than crude calculations. Compared with women without a mental illness, women with an illness were 1.5–1.6-times as likely to deliver before 32 weeks’ gestation because of premature rupture of the membranes or having spontaneous labor (adjusted relative risk for indicated birth before 32 weeks was not significant).
Women with a mental illness were not at a statistically significant increased risk of delivering between 32 and 36 weeks after adjustment ( Table 2 ). Overall, women in this sample with a mental illness diagnostic code were 1.2 times more likely to have a birth before 37 weeks compared with women with no such mental illness diagnosis (95% confidence interval, 1.1–1.3) ( Figure 2 ).
| Variable | Mental illness | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| None | Any | Depressive disorder, NOS | Anxiety disorders | Bipolar disorder | Schizophrenic disorders | Major depression | Personality disorders | More than one | |
| n, % | n, % | n, % | n, % | n, % | n, % | n, % | n, % | n, % | |
| aRR (95% CI) | aRR (95% CI) | aRR (95% CI) | aRR (95% CI) | aRR (95% CI) | aRR (95% CI) | aRR (95% CI) | aRR (95% CI) | aRR (95% CI) | |
| Sample | 24,792 | 6198 | 3435 | 1799 | 1004 | 196 | 168 | 56 | 406 |
| Gestation at birth | |||||||||
| <32 wks | 168 (0.7) | 97 (1.6) | 39 (1.1) | 43 (2.4) | 18 (1.8) | 7 (3.6) | 3 (1.8) | 2 (3.6) | 11 (2.7) |
| 1.5 (1.2, 1.8) a | 1.1 (0.8, 1.5) | 2.2 (1.6, 3.0) a | 1.6 (1.0, 2.6) b | 3.0 (1.4, 6.4) c | d | d | 2.5 (1.3, 4.5) c | ||
| PROM | 39 (0.2) | 28 (0.5) | 8 (0.2) | 13 (0.7) | 8 (0.8) | 1 (0.5) | 1 (0.6) | 1 (1.8) | 4 (1.0) |
| 1.6 (1.1, 2.3) b | 0.8 (0.4, 1.7) | 2.5 (1.4, 4.3) c | 2.5 (1.3, 5.1) c | d | d | d | 3.1 (1.1, 8.2) b | ||
| Spontaneous | 103 (0.4) | 59 (1.0) | 27 (0.8) | 26 (1.5) | 8 (0.8) | 5 (2.6) | 1 (0.6) | 1 (1.8) | 6 (1.5) |
| 1.5 (1.1, 1.9) c | 1.2 (0.8, 1.8) | 2.2 (1.5, 3.3) a | 1.2 (0.6, 2.5) | 3.3 (1.3, 8.1) b | b | b | 2.3 (1.0, 5.1) | ||
| Indicated | 20 (0.1) | 8 (0.1) | 2 (0.1) | 4 (0.2) | 2 (0.2) | 1 (0.5) | 1 (0.6) | 0 (0.0) | 1 (0.3) |
| 1.1 (0.5, 2.2) | d | 1.7 (0.6, 4.4) | d | d | d | d | d | ||
| ≥37 wks | 23,338 (94.1) | 5664 (91.4) | 31,969 (92.3) | 1634 (90.8) | 915 (91.1) | 166 (84.7) | 143 (85.1) | 43 (76.8) | 358 (88.2) |
| Reference | |||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


