Bogue CW: Genetic and molecular basis of airway and lung development. In Haddad GG et al (eds): Basic Mechanisms of Pediatric Respiratory Disease. BC Decker; 2002.
Burri P: Structural aspects of prenatal and postnatal development and growth of the lung. In McDonald JA (ed): Lung Growth and Development. BC Decker; 1997.
Wharburton D et al: Molecular mechanisms of early lung specification and branching morphogenesis. Pediatr Res 2005;57(5 Pt 2): 26R [PMID: 15817505].
DIAGNOSTIC AIDS
PHYSICAL EXAMINATION OF THE RESPIRATORY TRACT
The four components of a complete pulmonary examination include inspection, palpation, auscultation, and percussion. Inspection of respiratory rate, depth, ease, symmetry, and rhythm of respiration is critical to the detection of pulmonary disease. In young children, an elevated respiratory rate may be an initial indicator of pneumonia or hypoxemia. In a study of children with respiratory illnesses, abnormalities of attentiveness, inconsolability, respiratory effort, color, and movement had a good diagnostic accuracy in detecting hypoxemia. Palpation of tracheal position, symmetry of chest wall movement, and vibration with vocalization can help in identifying intrathoracic abnormalities. For example, a shift in tracheal position can suggest pneumothorax or significant atelectasis. Tactile fremitus may change with consolidation or air in the pleural space. Auscultation should assess the quality of breath sounds and detect the presence of abnormal sounds such as fine or coarse crackles, wheezing, or rhonchi. Wheezing or prolonged expiratory compared to inspiratory time suggests intrathoracic airways obstruction. Tachypnea with an equal inspiratory and expiratory time suggests decreased lung compliance. Transmitted voice sounds in egophony and whispered pectoriloquy change with lung consolidation. It is important to know the lung anatomy in order to identify the location of abnormal findings (Figure 19–1). In older patients, unilateral crackles are the most valuable examination finding in pneumonia. Percussion may identify tympanic or dull sounds that can help define an intrathoracic process. (This component of the examination can prove challenging in young children, who may not cooperate.) Although chest radiography has replaced the utility of these tests, they can be helpful when imaging is not available.
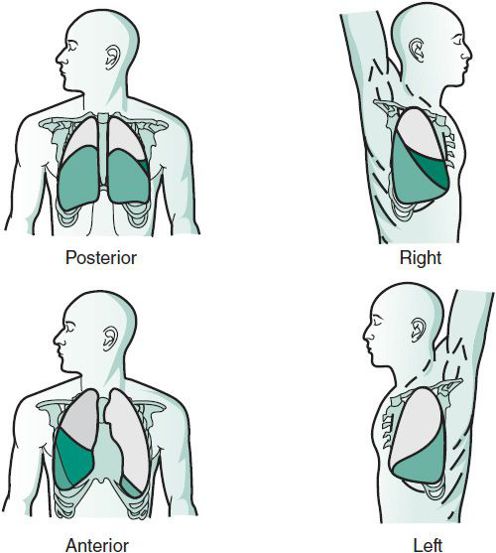
 Figure 19–1. Projections of the pulmonary lobes on the chest surface. The upper lobes are white, the right-middle lobe is the darker color, and the lower lobes are the lighter color.
Figure 19–1. Projections of the pulmonary lobes on the chest surface. The upper lobes are white, the right-middle lobe is the darker color, and the lower lobes are the lighter color.
Extrapulmonary manifestations of pulmonary disease include acute findings such as cyanosis and altered mental status and signs of chronic respiratory insufficiency such as growth failure, clubbing, and osteoarthropathy. Evidence of cor pulmonale (loud pulmonic component of the second heart sound, hepatomegaly, elevated neck veins, and rarely, peripheral edema) signifies pulmonary hypertension and may accompany advanced lung disease.
Respiratory disorders can be secondary to disease in other systems. It is therefore important to look for other conditions such as metabolic acidosis, congenital heart disease, neuromuscular disease, immunodeficiency, autoimmune disease, and occult malignancy (arthritis or hepatosplenomegaly). Children with an elevated body mass index are more likely to present with respiratory symptoms and need to be evaluated for pulmonary pathology versus deconditioning or dyspnea.
Wang WH et al: Joint effects of birth outcomes and childhood body mass index on respiratory symptoms. Eur Resp J 2012 May;39(5):1213-9. doi: 10.1183/09031936.00091311. Epub 2012 Mar 22.
Wipf JE et al: Diagnosing pneumonia by physical examination: Relevant or relic? Arch Intern Med 1999;159:1082 [PMID: 10335685].
PULMONARY FUNCTION TESTS
Pulmonary function tests (PFTs) are objective measures of lung and airway physiology that can help differentiate obstructive from restrictive lung diseases, measure disease severity, measure disease progression, and evaluate response to therapy. Because the range of predicted normal values changes with growth, serial determinations of lung function are often more informative than a single determination. Patient cooperation and consistent effort is essential for almost all standard physiologic assessments. With a well-trained technician in a comfortable environment aided by visual incentives, and an interactive computer-animated system, most children age 3 years and older can produce satisfactory results. Lung function measurements in infants and toddlers are available at centers with specialized equipment and expertise. Despite these limitations, tests of lung function are valuable in the care of children. Children with cystic fibrosis perform pulmonary function testing routinely as early as they can cooperate. The Expert Panel Report (3) recommends pulmonary function testing be performed routinely for evaluation and management of asthmatic children age 5 and older. Current spirometers use a pneumotachograph to record flow over time and produce a volume-time tracing (spirogram) or a flow-volume curve. The patient inhales maximally, holds his or her breath for a short period, and then exhales as fast and hard as possible until they reach residual volume or for at least 3 seconds. The values reported include: the forced vital capacity (FVC), which is the total volume of air that is exhaled; the forced expiratory volume in the first second of the exhalation (FEV1); the ratio of the FEV1/FVC; the forced expiratory flow at the middle of the vital capacity (FEF25–75); and the peak expiratory flow rate (PEFR). A suggested range of normal for these measurements are included in Table 19–1 and examples are shown in the figures. Obstructive processes include asthma, bronchopulmonary dysplasia (BPD), and cystic fibrosis (CF). Restrictive lung disease can be caused by chest wall deformities that limit lung expansion, muscle weakness, and interstitial lung diseases such as collagen-vascular diseases, hypersensitivity pneumonitis, and interstitial fibrosis. Confirmation of restrictive lung or chest wall physiology requires lung volume measurements (eg, total lung capacity, residual volume, and functional residual capacity) because poor effort can mimic restrictive physiology. Lung volume measurements are usually only available at specialized centers. (For examples of pulmonary function tests, see Figures 19–2 to 19–4.)
Table 19–1. Classification of lung function abnormalities.
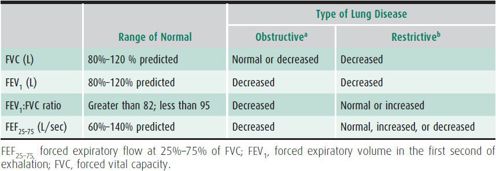
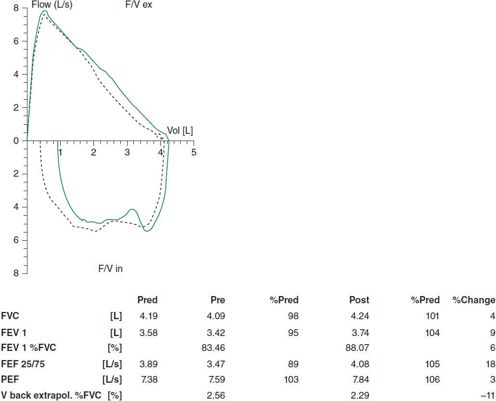
 Figure 19–2. Normal flow volume loop pre and post bronchodilator.
Figure 19–2. Normal flow volume loop pre and post bronchodilator.
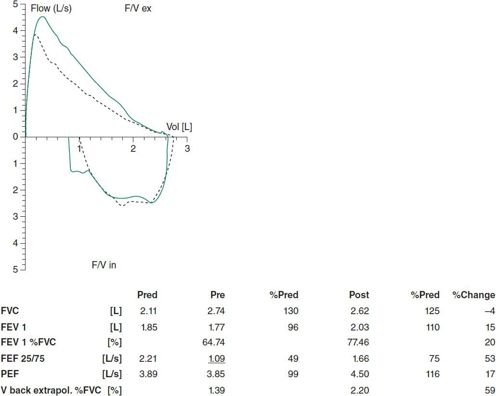
 Figure 19–3. Flow volume loops from a child with asthma (obstructive pattern).
Figure 19–3. Flow volume loops from a child with asthma (obstructive pattern).
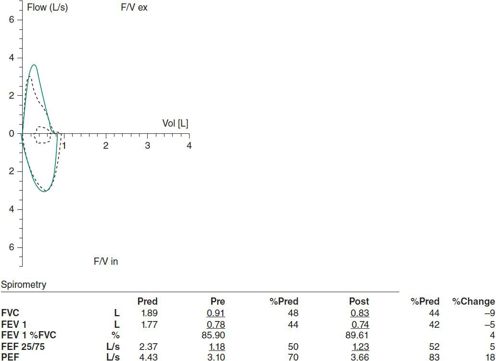
 Figure 19–4. Flow volume loops from a child with scoliosis (restrictive pattern): lung volume studies are needed to confirm restriction).
Figure 19–4. Flow volume loops from a child with scoliosis (restrictive pattern): lung volume studies are needed to confirm restriction).
The peak expiratory flow rate, the maximal flow recorded during an FVC maneuver, can be assessed by handheld devices. These devices are not as well calibrated as spirometers and the PEFR measurement can vary greatly with patient effort, so they are not good substitutes for actual spirometry. However, peak flow monitoring can be helpful in a patient with asthma that is difficult to control or for patients with poor perception of their airflow obstruction
Couriel JM, Child F: Applied physiology: lung function tests in children. Curr Paediatrics 2006;16:413–419.
Galant SP, Nickerson B: Lung function measurement in the assessment of childhood asthma: recent important developments. Curr Opin Allergy Clin Immunol 2010;10:149–154 [PMID: 20035221].
ASSESSMENT OF OXYGENATION & VENTILATION
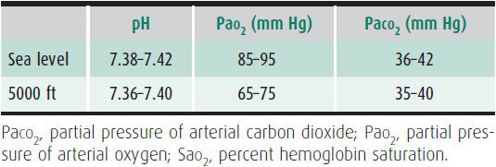
Arterial blood gas measurements define the acid-base balance between respiration at the tissue level and that in the lungs. Blood gas measurement is essential in critically ill children to evaluate hypoxemia, acidosis, and hypercarbia. Blood gas measurements can be used to categorize acid-base disturbances as respiratory, metabolic, or mixed. Blood gas measurements are affected by abnormalities of respiratory control, gas exchange, respiratory mechanics, and the circulation. In pediatrics, hypoxemia (low partial pressure of arterial oxygen [Pao2]) most commonly results from ventilation (V’) and perfusion (Q’) mismatch. Common pediatric diseases that may be associated with
hypoxemia due to V’/Q’ mismatch include acute asthma, cystic fibrosis (CF), pneumonia, bronchiolitis, and bronchopulmonary dysplasia (BPD). Other causes of hypoxemia include hypoventilation, shunts, and diffusion barrier for oxygen. Hypercapnia (elevated partial pressure of arterial carbon dioxide [Paco2]) results from inadequate alveolar ventilation (ie, inability to clear the CO2 produced). This is termed hypoventilation. Causes include decreased central respiratory drive, respiratory muscle weakness, and low-tidal-volume breathing as seen in restrictive lung diseases, severe scoliosis, or chest wall trauma. Hypercapnea can also occur when severe V’/Q’ mismatch is present which may occur with severe CF or BPD. Table 19–2 gives normal values for arterial pH, Pao2, and Paco2 at sea level and at 5000 ft.
Table 19–2. Normal arterial blood gas values on room air.
Venous blood gas analysis or capillary blood gas analysis can be useful for the assessment of Pco2 and pH, but not Po2 or saturation. Noninvasive assessment of oxygenation can be achieved with pulse oximetry (measuring light absorption by transilluminating the skin). Oxygenated hemoglobin absorbs light at different wavelengths than deoxygenated hemoglobin. Measurement during a systolic pulse allows estimation of arterial oxygen saturation. No heating of the skin is necessary. Values of oxygen saturation are reliable as low as 80%. The pulse oximeter has reduced reliability during conditions causing reduced arterial pulsation such as hypothermia, hypotension, or infusion of vasoconstrictor drugs. Carbon monoxide bound to hemoglobin results in falsely high oxygen saturation readings. Transcutaneous assessment of Pao2 is not commonly utilized because of the multiple factors that can interfere with accurate measurements.
Exhaled or end-tidal CO2 monitoring can be used to noninvasively estimate arterial CO2 content. It is used to monitor alveolar ventilation and is most accurate in patients without significant lung disease, particularly those with a good match of ventilation and perfusion and without airway obstruction. Monitoring of exhaled or end-tidal CO2 is commonly used during a polysomnogram and by anesthesia. Transcutaneous Pco2 monitoring is also feasible but may be less reliable than transcutaneous Po2 monitoring and should be used with caution if at all.
Ayers P, Warrington L: Diagnosis and treatment of simple acid-base disorders. Nutr Clin Pract 2008;23(2):122–127 [PMID: 18390779].
Fouzas S, Priftis KN, Anthracopoulos MB: Pulse oximetry in pediatric practice. Pediatrics 2011;128:740 [PMID: 21930554].
Kirk VG, Batuyong Ed, Bohn SG: Transcutaneous carbon dioxide monitoring and capnography during pediatric polysomnography. Sleep 2006;29(12):1601–168 [PMID: 17252891].
Salyer JW: Neonatal and pediatric pulse oximetry. Respir Care 2003 Apr;48(4):386–396 [PMID: 12667266].
Tobias JD: Transcutaneous carbon dioxide monitoring in infants and children. Paediatr Anaesth 2009 May;19(5):434–444 [PMID: 19236597].
DIAGNOSIS OF RESPIRATORY TRACT INFECTIONS
Respiratory tract infections may be caused by bacteria, viruses, atypical bacteria (eg, Mycoplasma pneumonia and Chlamydia pneumoniae), Mycobacterium tuberculosis, nontuberculous mycobacterium, or fungi (eg, Aspergillus and Pneumocystis jiroveci). The type of infection suspected and appropriate diagnostic tests vary depending on host factors such as underlying lung disease, immune function, and geographic region. Sources of respiratory tract secretions for diagnostic testing include nasopharyngeal and oropharyngeal swabs; expectorated and induced sputum; tracheal aspirates; direct lung or pleural fluid sampling; bronchoalveolar lavage fluid; and gastric aspirates, specifically for M tuberculosis. Blood and urine samples may also be used for serologic and antigen testing. Spontaneously expectorated sputum is the least invasive way to collect a sample for diagnostics, though it is rarely available from patients younger than age 6 years. Sputum induction, performed by inhaling aerosolized hypertonic saline, is a relatively safe, noninvasive means of obtaining lower airway secretions. Sputum induction has been used in patients with CF and may be useful in patients with suspected M tuberculosis, P jiroveci pneumonia, or complicated community-acquired pneumonia. Tracheal aspirates can be obtained easily from patients with endotracheal or tracheostomy tubes. Culture of respiratory tract samples is the most commonly used approach to detect and identify airway pathogens. Molecular diagnostic tests, based on PCR amplification and detection of nucleic material from microbes, may offer more rapid and sensitive testing for microbes. Molecular assays are used for detection of viruses and atypical bacteria in many laboratories. PCR is also used as an adjunct to culture for identification of M tuberculosis, nontuberculous mycobacteria, and some fastidious bacteria. Molecular approaches to the diagnosis of M tuberculosis and P jiroveci are also available and their use is likely to become more widespread.
Hammitt Laura L et al: Specimen collection for the diagnosis of pediatric pneumonia. Clin Infect Dis 2012;54(S2):S132–S139 [PMID: 22403227].
Murboch DR et al: Laboratory methods for determining pneumonia etiology in children. Clin Infect Dis 2012 Apr;54(Suppl 2): S146–S152 [PMID: 22403229].
Zumla A et al: Tuberculosis. N Engl J Med 2013;368(8):745–755 [PMID: 23425167].
IMAGING OF THE RESPIRATORY TRACT
The plain chest radiograph remains the foundation for investigating the pediatric thorax. Both frontal (posterior-anterior) and lateral views should be obtained if feasible. The radiograph is useful for evaluating chest wall abnormalities, heart size and shape, mediastinum, diaphragm, and lung parenchyma. When pleural fluid is suspected, lateral decubitus radiographs may be helpful in determining the extent and mobility of the fluid. When a foreign body is suspected, forced expiratory radiographs may show focal air trapping and shift of the mediastinum to the contralateral side. Lateral neck radiographs can be useful in assessing the size of adenoids and tonsils and also in differentiating croup from epiglottitis, the latter being associated with the “thumbprint” sign.
Barium swallow is indicated for detection of swallowing dysfunction in patients with suspected aspiration, tracheoesophageal fistula, gastroesophageal reflux, vascular rings and slings, and achalasia. Airway fluoroscopy assesses both fixed airway obstruction (eg, tracheal stenosis, masses, or tracheal compression) and dynamic airway obstruction (eg, tracheomalacia). Fluoroscopy or ultrasound of the diaphragm can detect paralysis by demonstrating paradoxic movement of the involved hemidiaphragm.
Chest CT is useful in evaluation of congenital lung lesions, pleural disease (eg, effusion or recurrent pneumothorax), mediastinum (eg, lymphadenopathy), pulmonary nodules or masses. High-resolution CT is best for evaluating interstitial lung disease (ILD) or bronchiectasis while decreasing radiation exposure compared to a standard CT. Magnetic resonance imaging (MRI) is useful for defining vascular or bronchial anatomical abnormalities. Ventilation-perfusion scans can provide information about regional ventilation and perfusion and can help detect vascular malformations and pulmonary emboli. Pulmonary angiography is occasionally necessary to define the pulmonary vascular bed more precisely. Recent concerns about radiation exposure in children led to the Image Gently campaign, an initiative of The Alliance for Radiation Safety in Pediatric Imaging, dedicated to increasing awareness of the need for radiation protection for children. Identified challenges include the need for continued education particularly at adult-focused hospitals, increased emphasis on appropriateness of pediatric imaging and outcomes research to validate the use of CT, and establishing ranges of optimal CT technique when imaging children.
Goske MJ et al: Image Gently: progress and challenges in CT education and advocacy. Pediatr Radiol 2011 Sep;41(Suppl 2): 461–466 [PMID: 22988269].
Image Gently Campaign website: http://www.pedrad.org/associations/5364/ig/.
Schneebaum et al: Use and yield of chest computed tomography in the diagnostic evaluation of pediatric lung disease. Pediatrics 2009;124:472–479 [PMID: 19620200].
LARYNGOSCOPY & BRONCHOSCOPY
Direct visualization of the airways may be necessary to establish the etiology of the respiratory problem despite an extensive history and physical and sophisticated imaging. This can be achieved with rigid or flexible instrumentation. Indications for laryngoscopy include hoarseness, stridor, symptoms of obstructive sleep apnea, and laryngeal wheezing. Indications for bronchoscopy include wheezing, suspected foreign body, recurrent pneumonia, persistent atelectasis, chronic cough, and hemoptysis. A flexible bronchoscope can also be used to assess placement and patency of an endotracheal tube. In general, the more specific the indication, the higher the diagnostic yield. Each method, rigid or flexible, has advantages and for some patients both should be employed sequentially under the same anesthesia.
The rigid, open tube instruments have the best optics and allow surgical intervention to be easily achieved such as removal of a foreign body. Rigid bronchoscopy is done with general anesthesia. Flexible laryngoscopy may be done with topical anesthesia or light sedation and flexible bronchoscopy can be done with either conscious sedation or general anesthesia. The flexible bronchscopy is of a smaller caliber and allows more distal examination of the airways. Because it is smaller, the flexible bronchoscope does not stent the airway open during the procedure and often dynamic airway collapse is more easily documented by the flexible procedure. Bronchoalveolar lavage is useful to sample the alveolar space for infection, inflammation, hemorrhage, or aspiration. Although removal of foreign bodies has been achieved with the flexible bronchoscope in larger children, the standard of care in most institutions is to remove foreign bodies via the rigid bronchoscope.
Transbronchial biopsy in children is limited to evaluation of infection and rejection in lung transplant patients. There is low diagnostic yield in most conditions. Transbronchial biopsy may have a role in sarcoidosis. Video-assisted thoracoscopic lung biopsy (VATS) provides a more substantial specimen for pathologic assessment.
Nicholai T: The role of rigid and flexible bronchoscopy in children. Paediatr Respir Rev 2011;12:190–195 [PMID: 21722848].
GENERAL THERAPY OF PEDIATRIC LUNG DISEASES
OXYGEN THERAPY
The goal of supplemental oxygen (O2) therapy is to relieve hypoxemia. Supplemental oxygen can reduce the work of breathing, resulting in fewer respiratory symptoms; relax the pulmonary vasculature, lessening the potential for pulmonary hypertension and congestive heart failure; and improve feeding. Patients breathing spontaneously can be treated by nasal cannula, head hood, or mask (including simple, rebreathing, nonrebreathing, or Venturi masks). The goal of O2 therapy is to achieve an arterial oxygen tension of 65–90 mm Hg or an oxygen saturation above 92%, although lower Pao2 or Spo2 levels may be acceptable in certain situations. The actual O2 concentration achieved by nasal cannula or mask depends on the flow rate, the type of mask used, and the patient’s age. Small changes in flow rate during oxygen administration by nasal cannula can lead to substantial changes in inspired oxygen concentration in young infants. The amount of oxygen required to correct hypoxemia may vary according to the child’s activity. It is not unusual, for example, for an infant with chronic lung disease to require 0.75 L/min while awake but 1 L/min while asleep or feeding.
Although the head hood is an efficient device for delivery of oxygen in young infants, the nasal cannula is used more often because it allows greater mobility. The cannula has nasal prongs that are inserted in the nares. Flow through the cannula should generally not exceed 3 L/min to avoid excessive drying of the mucosa. Even at high flow rates, oxygen by nasal cannula rarely delivers inspired oxygen concentrations greater than 40%–45%. In contrast, partial rebreathing and nonrebreathing masks or head hoods achieve inspired oxygen concentrations as high as 90%–100%. Heated high-flow nasal cannulas have been developed recently to deliver a high flow rate without a high Fio2.
Physical findings of hypoxemia are subtle. Adequate oxygenation should be measured by the arterial oxygen tension or pulse oximetry. The advantages of the latter noninvasive method include the ability to obtain continuous measurements during normal activities and to avoid artifacts caused by crying or breath-holding during arterial puncture. For children with cardiopulmonary disorders that require chronic supplemental oxygen therapy (eg, bronchopulmonary dysplasia or cystic fibrosis), frequent noninvasive assessments are essential to ensure the safety and adequacy of O2 treatment.
AARC Clinical Practice Guidelines: selection of an oxygen delivery device for neonatal and pediatric patients-2002 revision and update. Respir Care 2002;47:707–716 [PMID: 12078654].
Ralston M et al (eds): Pediatric Advanced Life Support Provider Manual. American Heart Association and American Academy of Pediatrics; 2006.
INHALATION OF MEDICATIONS
Inhalation of medications is a mainstay of therapy for pediatric respiratory conditions and are routinely used in patients with chronic diseases such as cystic fibrosis (CF), bronchopulmonary dysplasia (BPD), and asthma, as well as in acute illnesses such as infectious laryngotracheobronchitis and bronchiolitis (Table 19–3). Short-acting β-agonists and anticholinergics provide acute bronchodilitation (relievers), whereas inhaled corticosteroids and cromones provide anti-inflammatory effects (controllers). Nebulized antibiotics have documented benefit in CF and nebulized mucolytic medications are used in CF and other conditions with impaired secretion control such as non-CF bronchiectasis.
Table 19–3. Common uses for inhaled medications in pediatric respiratory illness.
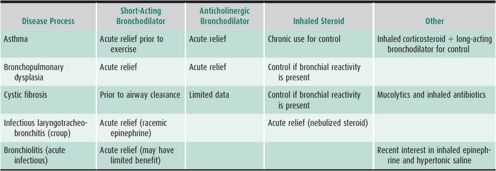
The medications can be delivered by pressurized metered dose inhaler (pMDI), dry powder inhaler (DPI), or compressed air-driven wet nebulization. Careful attention to delivery technique is critical to optimize medication delivery to the airways. A valved holding chamber or similar spacer should be used with pMDI use, and this technique has been shown to be effective in infants as young as 4 months of age. A face-mask interface is recommended for both pMDI and wet nebulization in infants and toddlers; a simple mouth piece suffices for older children who can form a seal around the mouth piece. Delivery technique should be assessed and reviewed at each clinical visit.
Ahrens RC, Hess DR, Anderson P, Dhand R, Rau JL et al: Device selection and outcomes of aerosol therapy: evidence-based guidelines. Chest 2005;127:335–371 [PMID: 15654001].
Janssens HM, Tiddens HA: Aerosol therapy: the special needs of young children. Paediatr Respir Rev 2006;7(Suppl 1) [PMID: 16798606].
AIRWAY CLEARANCE THERAPY
Chest physical therapy, with postural drainage, percussion, and forced expiratory maneuvers, has been widely used to improve the clearance of lower airway secretions in children with CF, bronchiectasis, and neuromuscular disorders. Currently available airway clearance techniques include: chest physiotherapy, autogenic drainage, blowing therapies (bubbles, pinwheels), active coughing, positive expiratory pressure (PEP) with handheld devices, intrapulmonary percussive ventilation, or high-frequency chest compression. The decision about which technique to use should be based on the patient’s age and preference after trying different approaches. Daily exercise is an important adjunctive therapy for airway clearance and overall lung health. Cough assist devices (eg, mechanical insufflator-exsufflators) are useful for children with a weak cough. For example, they are useful for children with neuromuscular disorders such as muscular dystrophy and spinal muscular atrophy. Bronchodilators or mucolytic medications may be given prior to or during airway clearance therapy. Inhaled corticosteroids and inhaled antibiotics should be given after airway clearance therapy so that the airways are first cleared of secretions, allowing the medications to maximally penetrate into the lung. Airway clearance has not been shown to be beneficial for patients with acute respiratory illnesses such as pneumonia, bronchiolitis, and asthma.
De Boeck K et al: Airway clearance techniques to treat acute respiratory disorders in previously healthy children: where is the evidence? Eur J Pediatr 2008;167;607–612 [PMID: 18322699].
Kravitz RM: Airway clearance in Duchenne muscular dystrophy. Pediatrics 2009;123:S231–S235 [PMID: 19420150].
Lester MK et al: Airway-clearance therapy guidelines and implementation. Resp Care 2009;54(6):733–750 [PMID: 19467161].
AVOIDANCE OF ENVIRONMENTAL HAZARDS
Environmental insults can aggravate existing lung diseases and impair pulmonary function, and probably cause lung disease in children. Outdoor air pollution (ozone and particulates), indoor pollution, diesel exhaust, and household fungi are examples. Environmental tobacco poisoning, either second or third hand, dramatically increases childhood pulmonary morbidity. Many adolescents personally abuse tobacco and become addicted. Public health policies that limit smoke exposure and reduce advertising to children have had a positive impact. Smoking family members should be admonished to quit smoking and do everything possible to minimize environmental smoke exposure to the children around them. Homes with mold should have remediation, particularly if children with lung disease are in residence. Ozone exposure can be limited by avoiding outdoor activities during the height of daily ozone levels, but additional public policy changes will be required to further reduce ozone pollutants in the air.
For children with asthma, family pets may be a significant trigger as can household cockroach infestation. Despite the known risk, many families are reluctant to eliminate risk of exposure to the pet. Families should also be counseled about risks of foreign body aspiration in curious toddlers.
Anderson ME, Bogdan GM: Environments, indoor air quality, and children. Pediatr Clin N Am 2007;54:295–307 [PMID: 17448361].
State of the Air Report 2012: Report by the American Lung Association: http://www.stateoftheair.org/. Accessed March 13, 2013.
Tzivian L: Outdoor air pollution and asthma in children. J Asthma 2011;48:470 [PMID: 21486196].
DISORDERS OF THE CONDUCTING AIRWAYS
The conducting airways include the nose, mouth, pharynx, larynx, trachea, bronchi, and terminal bronchioles. These airways direct inspired air to the gas-exchange units of the lung but do not participate in gas exchange. Airflow obstruction in the conducting airways can occur at extrathoracic sites (eg, above the thoracic inlet) or at intrathoracic sites (eg, below the thoracic inlet). Extrathoracic or upper airway obstruction disrupts the inspiratory phase of respiration and is often manifest by stridor or “noisy breathing.” Intrathoracic obstruction disrupts the expiratory phase of respiration and is often manifest by wheezing and prolongation of the expiratory phase. After assessing whether the obstruction is extrathoracic or intrathoracic the next challenge is to determine if the obstruction is fixed or variable. Fixed obstructions disrupt each breath and the abnormal sounds are consistently heard. Fixed obstructions can be intrinsic to the airway or due to airway compression (extrinsic). They are often associated with anatomic abnormalities that may be amenable to surgical correction (Table 19–4).
Table 19–4. Classification and causes of upper airway obstruction.
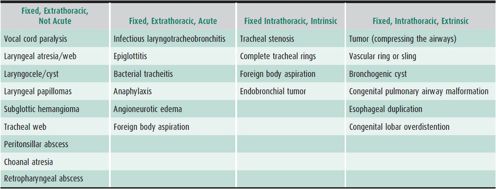
Variable obstruction leads to abnormal sounds with breathing that are softer or absent with normal quiet breathing and may sound different with every breath. Variable obstructions are often due to dynamic changes in airway caliber that occurs with laryngomalacia, tracheomalacia, or bronchomalacia. The onset and progression of the obstruction can provide important clues as to the etiology and help determine the urgency of evaluation and management. Obstructions due to dynamic airway collapse often improve with age, whereas fixed obstructions typically progress or fail to improve with age. Acute onset extrathoracic obstruction is often infectious. Clinical indications that the obstruction is severe include high-pitched stridor or wheezing, biphasic stridor, drooling or dysphagia, poor-intensity breath sounds, severe retractions, and poor color or cyanosis.
Helpful diagnostic studies in the evaluation of extrathoracic obstruction include chest and lateral neck radiographs, airway fluoroscopy, and barium swallow. Patients who have symptoms of severe chronic obstruction should have an electrocardiogram and/or ECHO to evaluate for right ventricular hypertrophy and pulmonary hypertension. Patients suspected to have obstructive sleep apnea should have polysomnography (see section on Sleep Disordered Breathing). Diagnostic studies for intrathoracic obstruction include two-view chest radiographs, a sweat test, and pulmonary function tests. Other diagnostic studies are dictated by the history and physical findings. If asthma is suspected, a trial of bronchodilators and/or anti-inflammatories should be considered. If noninvasive studies are unable to establish the cause of airway obstruction, laryngoscopy and bronchoscopy remaim the procedures of choice to establish the precise diagnosis. In older children, pulmonary function tests can differentiate fixed from variable airflow obstruction and may identify the site of obstruction. Treatment should be directed at relieving airway obstruction and correcting the underlying condition if possible.
LARYNGOMALACIA & CONGENITAL DISORDERS OF THE EXTRATHORACIC AIRWAY
LARYNGOMALACIA
Laryngomalacia is a benign congenital disorder in which the cartilaginous support for the supraglottic structures is underdeveloped. It is the most common cause of variable extrathoracic airway obstruction and manifests as intermittent stridor in infants and usually is seen in the first 6 weeks of life. Stridor has been reported to be worse in the supine position, with increased activity, with upper respiratory infections, and during feeding; however, the clinical presentation can be variable. Patients may have slight oxygen desaturation during sleep. The condition usually improves with age and resolves by the time the child is 2 years old, but in some cases symptoms persist for years. The diagnosis is established by direct laryngoscopy, which shows inspiratory collapse of an omega-shaped epiglottis (with or without long, redundant arytenoids). In mildly affected patients with no stridor at rest and no retractions, treatment is not usually needed. Patients with either severe symptoms of airway obstruction such as stridor with each breath, retractions, and increased work of breathing or more chronic signs such as feeding difficulties, failure to thrive, obstructive sleep apnea, hypoxemia, or severe dyspnea may benefit from surgical epiglottoplasty.
Meier JD et al: Improved growth curve measurements after supraglottoplasty. The Laryngoscope 2011;121(7):1574 [PMID: 21647914].
Thompson DM et al: Laryngomalacia: factors that influence disease severity and outcomes of management. Curr Opin Otolaryngol Head Neck Surg 2010;18(6):564 [PMID: 20962644].
OTHER CAUSES OF CONGENITAL EXTRATHORACIC OBSTRUCTION
Other congenital lesions of the larynx such as laryngeal atresia, laryngeal web, laryngocele and cyst of the larynx, subglottic hemangioma, and laryngeal cleft usually present as fixed extrathoracic obstruction and are best evaluated by direct laryngoscopy.
Laryngeal atresia presents at birth with severe respiratory distress and is usually fatal. Laryngeal web, representing fusion of the anterior portion of the true vocal cords, is associated with hoarseness, aphonia, and stridor. Surgical correction is usually necessary. Laryngeal cysts and lanryngocoeles present with stridor and significant airway obstruction. Laryngeal cysts are superficial and are generally fluid filled. Laryngoceles communicate with the interior of the larynx and may be either air- or fluid-filled. Both require surgery or laser therapy.
Subglottic hemangiomas are a rare cause of upper airway obstruction in infants and are associated with cutaneous vascular lesions of the skin in 50%–60% of patients. Although vascular malformations regress spontaneously, airway obstruction usually necessitates intervention. Medical management options include propranolol, systemic steroids, or intralesional steroids. Surgical intervention with laser ablation is usually successful, but rarely tracheostomy is required. Laryngeal cleft is an uncommon condition resulting from failure of posterior cricoid fusion. Patients present with stridor, dysphagia, or silent aspiration. A type 1 laryngeal cleft (above the vocal cords) may not show aspiration on a modified barium swallow while more severe type 2 and 3 laryngeal clefts almost always do. All types of clefts may result in recurrent or chronic pneumonia and failure to thrive. The diagnosis is made by direct laryngoscopy with attention to spreading the glottis structures apart and assessing for the absence of tissue above the vocal folds. The decision to correct type 1 clefts should be made after multidisciplinary consideration of the pulmonary complications and other comorbidities. Repair of type 1 clefts may be addressed surgically or with an injection laryngoplasty. More severe clefts require surgical repair and may require tracheostomy. Normal swallow function without aspiration may take months to occur, even after repair.
Ahmad SM, Soliman AM: Congenital anomalies of the larynx. Otolaryngol Clin North Am 2007 Feb;40(1):177–191 [PMID: 17346567].
Cohen M et al: Injection laryngoplasty for type 1 laryngeal cleft in children. Otolaryngol Head Neck Surg 2011;144(5):789 [PMID: 21493369].
Starkey E et al: Propranolol for infantile haemangiomas: a review. Arch Dis Child 2011;96(9):890 [PMID: 21622997].
ACQUIRED DISORDERS OF THE EXTRATHORACIC AIRWAY
Acquired disorders of the extrathoracic airway can present acutely or with recurrent symptoms of upper airway obstruction. Children with acquired disorders of the extrathoracic airway present with inspiratory sounds consistent with stridor. The pitch of the sound varies depending on the diagnosis. Upper airway obstruction can progress quickly and may be life-threatening, requiring close observation.
FOREIGN BODY ASPIRATION IN THE EXTRATHORACIC AIRWAY
Aspiration of a foreign body into the respiratory tract is a significant cause of accidental death each year.
The foreign body can lodge anywhere along the respiratory tract. Foreign bodies that lodge in the esophagus may compress the airway and cause respiratory distress. More typically, the foreign body lodges in the supraglottic airway, triggering protective reflexes that result in laryngospasm. Small objects such as coins may pass through the glottis and obstruct the trachea. Objects that pass into the lower airway cause coughing but more variable respiratory distress (see section Acquired Causes of Intrathoracic Airway Obstruction).
Foreign body aspiration is commonly seen with small, round foods such as nuts and seeds, berries, corn/popcorn, hot dogs, and beans. Children 6 months to 4 years are at highest risk. Homes and child care centers in which an older sibling or child feeds age-inappropriate foods (eg, peanuts, hard candy, or carrot slices) to the younger child are typical. Without treatment, progressive cyanosis, loss of consciousness, seizures, bradycardia, and cardiopulmonary arrest can follow.
 Clinical Findings
Clinical Findings
Signs at the time of ingestion can include coughing, choking, or wheezing. Onset is generally abrupt, with a history of the child running with food in the mouth or playing with seeds, small coins, or toys.
The diagnosis is established by acute onset of choking along with inability to vocalize or cough and cyanosis with marked distress (complete obstruction), or with drooling, stridor, and ability to vocalize (partial obstruction). Chest x-rays and other imaging studies have been used to evaluate for foreign body ingestion. However, rigid bronchoscopy is the gold standard for diagnosis.
 Treatment
Treatment
The emergency treatment of upper airway obstruction due to foreign body aspiration has changed over the last few years. If complete obstruction is present, then one must intervene immediately. If partial obstruction is present, then the choking subject should be allowed to use his or her own cough reflex to remove the foreign body. If, after a brief observation period, the obstruction increases or the airway becomes completely obstructed, acute intervention is required. The American Academy of Pediatrics and the American Heart Association distinguish between children younger than and older than 1 year of age. In an awake child younger than 1 year of age with a complete obstruction, the child should be placed face down over the rescuer’s arm. Five measured back blows are delivered rapidly followed by rolling the infant over and delivering 5 rapid chest thrusts. This sequence is repeated until the obstruction is relieved. In a choking child older than 1 year of age, abdominal thrusts (Heimlich maneuver) should be performed, with special care in younger children because of concern about possible intra-abdominal organ injury. If the child of any age becomes unresponsive, cardiopulmonary resuscitation is recommended. Chest compressions may help to dislodge the foreign body.
Blind finger sweeps should not be performed in infants or children because the finger may push the foreign body further into the airway causing worse obstruction. The airway may be opened by jaw thrust, and if the foreign body can be directly visualized, careful removal with the fingers or instruments should be attempted. Patients with persistent apnea and inability to achieve adequate ventilation may require emergency intubation, tracheotomy, or needle cricothyrotomy, depending on the setting and the rescuer’s skills. Foreign body removal is most successfully performed using a rigid bronchoscopy under general anaesthesia.
Berg MD et al: Pediatric basic life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics 2010 Nov;126(5):e1345-60. doi: 10.1542/peds.2010-2972C. Epub 2010 Oct 18 [PMID:20956430].
Fiedkowski CW, Zheng H, Firth PG: The anesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12,979 cases. Anesth Analg 2010;111(4):1016–1025 [PMID: 20802055].
CROUP SYNDROMES
Croup describes acute inflammatory diseases of the larynx, including viral croup (laryngotracheobronchitis), epiglottitis (supraglottitis), and bacterial tracheitis. These are the main entities in the differential diagnosis for patients presenting with acute stridor, although spasmodic croup, angioedema, laryngeal or esophageal foreign body, and retropharyngeal or peritonsillar abscess should be considered as well.
1. Viral croup
Viral croup generally affects young children 6 months to 5 years of age in the fall and early winter months and is most often caused by parainfluenza virus serotypes. Other organisms causing croup include respiratory syncytial virus (RSV), human coronavirus NL63, rhinovirus, human metapneumovirus, influenza virus A&B, rubeola virus, adenovirus, and M pneumoniae. Although inflammation of the entire airway is usually present, edema formation in the subglottic space accounts for the predominant signs of upper airway obstruction.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Usually a prodrome of upper respiratory tract symptoms is followed by a barking cough and stridor. Fever is usually absent or low-grade but may on occasion be high-grade. Patients with mild disease may have stridor when agitated. As obstruction worsens, stridor occurs at rest, accompanied in severe cases by retractions, air hunger, and cyanosis. On examination, the presence of cough and the absence of drooling favor the diagnosis of viral croup over epiglottitis.
B. Imaging
Anteroposterior and lateral neck radiographs in patients with classic presentations are not required but can be diagnostically supportive if the x-ray shows subglottic narrowing (the steeple sign) without the irregularities seen in tracheitis and a normal epiglottis. However, a severely ill patient should never be left unattended in the imaging suite.
 Treatment
Treatment
Treatment of viral croup is based on the symptoms. Mild croup, signified by a barking cough and no stridor at rest, requires supportive therapy with oral hydration and minimal handling. Mist therapy has historically been used but clinical studies do not demonstrate effectiveness. Conversely, patients with stridor at rest require active intervention. Oxygen should be administered to patients with oxygen desaturation. Nebulized racemic epinephrine (0.5 mL of 2.25% solution diluted in sterile saline) is commonly used because it has a rapid onset of action within 10–30 minutes. Both racemic epinephrine and epinephrine hydrochloride (l-epinephrine, an isomer) are effective in alleviating symptoms and decreasing the need for intubation.
The efficacy of glucocorticoids in croup is now firmly established. Dexamethasone, 0.6 mg/kg intramuscularly as one dose, improves symptoms, reduces the duration of hospitalizations and frequency of intubations, and permits earlier discharge from the emergency department. Oral dexamethasone (0.15 mg/kg) may be equally effective for mild to moderate croup. Inhaled budesonide (2–4 mg) also improves symptoms and decreases hospital stay and may be as effective as dexamethasone. Dexamethasone has also been shown to be more effective than prednisolone in equivalent doses.
If symptoms resolve within 3 hours of glucocorticoids and nebulized epinephrine, patients can safely be discharged without fear of a sudden rebound in symptoms. If, however, recurrent nebulized epinephrine treatments are required or if respiratory distress persists, patients require hospitalization for close observation, supportive care, and nebulization treatments as needed. In patients with impending respiratory failure, an airway must be established. Intubation with an endotracheal tube of slightly smaller diameter than would ordinarily be used is reasonably safe. Extubation should be accomplished within 2–3 days to minimize the risk of laryngeal injury. If the patient fails extubation, tracheostomy may be required. Other underlying causes should be considered in hospitalized patients with persistent symptoms over 3–4 days despite treatment.
 Prognosis
Prognosis
Most children with viral croup have an uneventful course and improve within a few days. Some evidence suggests that patients with a history of croup associated with wheezing may have airway hyperreactivity. It is not always clear if the hyperreactivity was present prior to the croup episode or if the viral infection causing croup altered airway function.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









