Reproductive Growth and Development in the Male Adolescent
David J. Breland and Mark L. Rubinstein
TESTIS
Testicular growth and maturation are largely influenced by testosterone, which is produced by the testicle both before and after birth.1 Testosterone production is regulated centrally by the hypothalamic-pituitary-testicular axis as well as intragonadally. Testosterone effects include embryologic male genital differentiation, neonatal imprinting of androgen-dependent target tissue, maturation of the genitalia at puberty, growth of skeletal muscle, deepening of the voice from laryngeal growth, epiphyseal cartilage growth during puberty, male hair growth and distribution, erythropoiesis, stimulation of sebaceous glands, and male social behavior.1,2
 DEVELOPMENTAL ANATOMY AND HISTOLOGY
DEVELOPMENTAL ANATOMY AND HISTOLOGY
The adult testicle is ovoid in shape with a volume of 15 to 25 mL, an average length of 4.6 cm (range 3.6–5.5 cm), and an average width of 2.6 cm (range 2.1–3.2 cm). Each testis is surrounded by a capsule made up of 3 layers: the outer visceral layer of the tunica vaginalis, the tunica albuginea, and the inner layer of the tunica vasculosa. Contained by the capsule, each testis is divided into 250 lobules by fibrous septae, with 1 to 4 seminiferous tubules in each lobule. The tubules account for 90% of testicular mass, and the interstitium accounts for the remaining 10%. The interstitium consists of Leydig cells, blood vessels, lymphatic channels, macrophages, and mast cells. Leydig cells are the major source of testosterone and are closely applied to the outer wall of the seminiferous tubule. Each seminiferous tubule is approximately 60 cm in length and 150 to 175 μm in diameter.3 The tubule is the site of spermatogenesis and contains 2 cell types, Sertoli cells and germ cells.4,5
 GONADAL DIFFERENTIATION
GONADAL DIFFERENTIATION
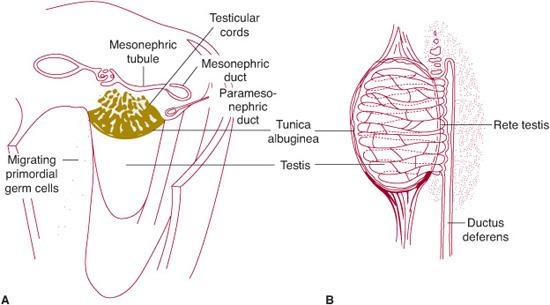
Although the sex of the embryo is determined at conception, the potential male and female gonads do not differ morphologically until the seventh week of development. Initially, they appear as gonadal ridges, into which the primordial germ cells migrate in the sixth week of growth. Primitive sex cords develop before incorporation of the germ cells and are the progenitors of the seminiferous tubules.1 By the fourth month, the primitive germ cells and Sertoli cells can be identified in the tubules (Fig. 65-1). Leydig cells are abundant during the fourth to sixth month and assist in influencing the sexual differentiation of the genital ducts and external genitalia by means of testosterone production. The fetal testes produce inducer substances, which promote growth of the mesonephric or wolffian duct and inhibit development of the paramesonephric or mÜllerian duct. The mesonephric duct persists (except for the most cranial portion, the appendix epididymis) and gives rise to the epididymis, ductus deferens, and seminal vesicle. The paramesonephric duct completely degenerates except for a small portion at the cranial end, which persists as the appendix testis. Descent of the testes from their abdominal origin to their final location in the scrotal sac begins in the seventh or eighth month.1,5 It is typically complete shortly before birth. However, testicular descent is sometimes completed post-natally. From birth until puberty, the testis remains static, although histologic and ultrastructural changes do occur, as outlined below.4 The prepubertal testis demonstrates tubules of small diameter and is populated by two cell types, progenitors of Sertoli cells and primary spermatogenic cells.4,5 The genetic determinants of sex differentiation is discussed in detail in Chapter 538.
Leydig Cells
Leydig cells are situated between the testicular cords and can first be recognized during the eighth week of gestation.4 They differentiate, multiply, and increase in size from weeks 9 to 14, until they occupy more than 50% of the testicle. Activation of the Leydig cells results in increased testosterone secretion, which peaks at about week 14 of fetal development.4,5 The Leydig cells gradually involute after weeks 17 to 18 of gestation. Involution is complete within a few weeks following birth. Levels of free testosterone are also thought to decline during the first several months after birth. At 4 to 8 years of age, precursors of the Leydig cells reappear and can be found grouped around vessels.1,4,5 At puberty, Leydig cells dramatically increase in number and size. They become well differentiated and are capable of steroid synthesis. In the mature testis, Leydig cells are the main source of testosterone in the pubertal and postpubertal male and thereby are responsible for development of secondary sexual characteristics of puberty.3-5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


