Cancer Survivorship and Recommendations for Follow-Up
Smita Bhatia and Anna T. Meadows
Five-year survival rates now approach 80%.1 This has resulted in a growing population of childhood cancer survivors—an estimated 300,000 survivors in the United States.2
Cancer and its treatment during childhood can result in a variety of long-term sequelae, such as impairment in growth and development, endocrine dysfunction, cognitive decline, cardiopulmonary compromise, as well as subsequent malignancies. These sequelae are primarily related to specific therapeutic exposures, and can reduce the overall quality of life (QOL) of the survivors. 
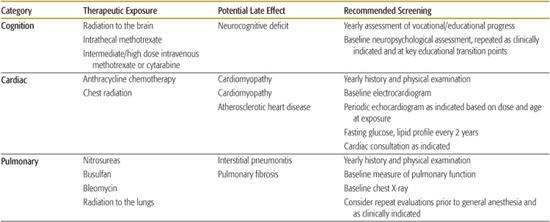
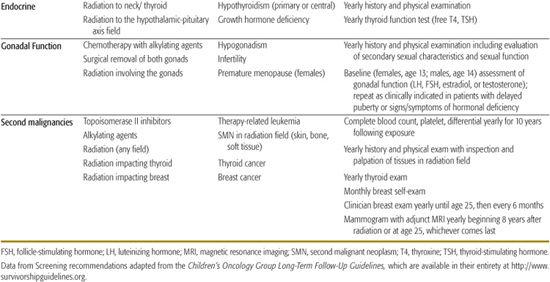
This chapter reviews some of these well-described, late-occurring adverse events in survivors of childhood cancer (Table 448-1). 
Table 448-1. Selected Exposure-Based Screening Recommedations
GROWTH AND DEVELOPMENT
Severe growth retardation (standing height below the fifth percentile for age- and sex-matched healthy individuals) has been observed in 30% of brain tumor survivors and in 15% of patients treated on certain antileukemia regimens,4,5 caused primarily by treatment with cranial irradiation. The effects of cranial irradiation are age and dose related.4 Treatment with growth hormone prior to closure of epiphyses in patients with documented growth hormone deficiency usually results in near normalization of final height. 
Screening
Monitoring of long-term survivors for growth problems relies on the use of standardized curves available online (http://www.cdc.gov/growthcharts). Frequent serial measurements should be obtained.  Endocrine consultation may be indicated for children whose height crosses two or more percentiles, or whose growth velocity is less than 5 cm/year, or whose height is less than the third percentile.
Endocrine consultation may be indicated for children whose height crosses two or more percentiles, or whose growth velocity is less than 5 cm/year, or whose height is less than the third percentile.
GONADAL FUNCTION
 MALE GONADAL FUNCTION
MALE GONADAL FUNCTION 
Bilateral orchiectomy results not only in infertility but also in testosterone deficiency, requiring ongoing hormonal replacement beginning in puberty. 
Radiation to the testes is known to result in germinal loss with decreases in testicular volume and sperm production, and increases in follicle-stimulating hormone (FSH). Effects are dose dependent, following exposures of 0.1 to 6 Gy. Higher doses than those toxic to germ (Sertoli) cells are needed to induce Leydig cell damage. Leydig cell damage is dose dependent and inversely related to age at treatment.6
Alkylating agents decrease spermatogenesis in a dose-dependent manner. Chemotherapy effects are less striking on slowly dividing Leydig cells, and may be age related. 
Screening
Screening includes an annual age-appropriate history and examination for Tanner staging, as well as measurement of serum luteinizing hormone (LH), follicle-stimulating hormone (FSH), and testosterone levels, is recommended as a baseline at age 14 years, and in boys in whom puberty appears to be delayed. Males at risk of infertility8 may benefit from semen analysis; close cooperation with an endocrinologist is essential in planning hormonal replacement therapy or in monitoring patients for spontaneous recovery.
 FEMALE GONADAL FUNCTION
FEMALE GONADAL FUNCTION 
Germ cell failure and loss of ovarian endocrine function occur concomitantly in females. Radiation effects are both age and dose dependent.9
Ovarian failure has also been associated with chemotherapy, especially the alkylating agents, and the toxicity demonstrates dose and age dependence.  For survivors who retain normal ovarian function after cancer therapy, there is an increased risk of premature menopause.15 The risk factors associated with an early menopause include exposure to high doses of alkylating agents and abdomino-pelvic radiation.
For survivors who retain normal ovarian function after cancer therapy, there is an increased risk of premature menopause.15 The risk factors associated with an early menopause include exposure to high doses of alkylating agents and abdomino-pelvic radiation.
Screening
The diagnostic evaluation of ovarian dysfunction should include history and physical examination. Serum gonadotropin (FSH, LH) and estradiol levels should be obtained as a baseline at age 13 years and as clinically indicated, in order to assess the need for hormone therapy to induce puberty. In addition, because young women may experience early onset of menopause, they should also undergo assessment of gonadotropin and estradiol levels if there are clinical symptoms of estrogen deficiency. 
THYROID FUNCTION
Hypothyroidism is a common late effect and almost always is the result of radiation to the neck. The likelihood of abnormalities depends on radiation dose. For those exposed to radiation doses exceeding 45 Gy, the actuarial risk of hypothyroidism at 20 years approaches 50%.16
Screening
Recommendations, for monitoring include annual assessment of thyroid functions (thyroid-stimulating hormone and free T4).
COGNITIVE DECLINE
Cognitive decline can be seen in children treated with cranial irradiation, high-dose systemic methotrexate and/or cytarabine, or intrathecal methotrexate. Risk factors include increasing radiation dose, young age at the time of therapy, treatment with both cranial irradiation and systemic or intrathecal chemotherapy, and female gender.19 Neurocognitive deficits usually become evident within 1 to 2 years following radiation, and are progressive.20 Affected children most often experience academic difficulties in the areas of reading, language, and mathematics. Children in the younger age groups treated with cranial irradiation may experience significant drops in IQ scores. 
Screening
Patients  should undergo a baseline neuro-psychological evaluation, repeated as clinically indicated and at key transition points (eg, when moving from grade school to middle/junior high school), as well as annual assessment of the survivor’s vocational or educational progress.23
should undergo a baseline neuro-psychological evaluation, repeated as clinically indicated and at key transition points (eg, when moving from grade school to middle/junior high school), as well as annual assessment of the survivor’s vocational or educational progress.23
CARDIOVASCULAR FUNCTION
Anthracyclines (eg, doxorubicin, daunomycin and idarubicin) are a well-known cause of cardiotoxicity.24,25 Chronic cardiotoxicity usually manifests itself as cardiomyopathy with progression to congestive heart failure. The incidence of cardiomyopathy is dose dependent. A cumulative dose exceeding 250 mg/m2 is associated with a higher risk of clinical heart failure.26 Other risk factors include a younger age at exposure to anthracyclines, exposure to radiation to the chest, female sex, and presence of other cardiac-compromising comorbidities. 
Coronary artery disease has been reported following radiation to the mediastinum, with a cumulative risk of 21% at 20 years after radiation.28
Screening
Patients who have received anthracycline chemotherapy need ongoing monitoring for late-onset cardiomyopathy, with frequency of evaluation based on total cumulative dose and age at the time of initial therapy.29,30 In addition to monitoring for cardiomyopathy, survivors who received radiation to fields that include the heart also need monitoring for potential early-onset atherosclerotic heart disease  . Specific recommendations for monitoring based on age and therapeutic exposure are available at http://www.survivorshipguidelines.org.18
. Specific recommendations for monitoring based on age and therapeutic exposure are available at http://www.survivorshipguidelines.org.18
PULMONARY FUNCTION
Pulmonary radiation can lead to pulmonary fibrosis and pneumonitis. 
Interstitial pneumonitis and pulmonary fibrosis have been reported after exposure to bleomycin and nitosoureas,32 with the chronic lung toxicity being dose dependent. 
Monitoring for pulmonary dysfunction in childhood cancer survivors includes assessment of symptoms such as chronic cough or dyspnea on annual follow-up. Risks of smoking and exposure to secondhand smoke should be discussed with all patients, and they should be counseled accordingly. Pulmonary function tests (including carbon monoxide diffusing capacity [DLCO] and spirometry) and chest x-ray are recommended at baseline upon entry into long-term follow-up for patients at risk, and repeated as clinically indicated in symptomatic patients. 
SECOND MALIGNANT NEOPLASMS 
Childhood cancer survivors demonstrate a 6-fold increased risk of developing a second cancer, when compared with the general population, and this risk continues to increase as the cohort ages.54
Ionizing radiation is associated with several types of second cancers, with the risk being highest when the exposure occurs at a younger age.55,56 The risk increases with the total dose of radiation,57-60 and with increasing follow-up.61 Examples of radiation-associated tumors include breast,62 lung, and thyroid cancers59; brain tumors60; and sarcomas.63
Female patients treated with mantle radiation before age 30 years are at a significantly higher risk of developing radiation-related breast cancer, in comparison with those treated in their adult years.62,64 The large majority of childhood cancer survivors are diagnosed with secondary breast cancer at a relatively young age, often before 40 years of age. 
An increased risk of developing thyroid cancer has been described after radiation therapy for several primary cancers, including Hodgkin lymphoma, acute lymphoblastic leukemia, and brain tumors.59
Therapy-related leukemia has been associated with specific chemotherapeutic agents, such as alkylating agents and topoisomerase II inhibitors.56 Although the risk for t-MDS/AML plateaus after 10 years, that for radiation-related solid tumors continues to climb with increasing follow-up.62
Screening 
Screening recommendations include careful annual physical examination of the radiation field with radiographic or other cancer-screening evaluations as indicated. Recommendations for females who received radiation with potential impact to the breast (ie, radiation doses of 20 Gy or higher to the mantle, mediastinal, whole lung, and axillary fields) include monthly breast self-examination beginning at puberty, annual clinical breast examinations beginning at puberty until age 25 years, and then a clinical breast examination every 6 months, with annual mammograms and magnetic resonance imaging (MRIs) beginning 8 years after radiation or at age 25 (whichever occurs later). 
Recommendations for monitoring for therapy-related leukemia include annual complete blood count for 10 years after exposure to alkylating agents or topoisomerase II inhibitors.
BURDEN OF MORBIDITY 
Approximately two-thirds of the survivors will experience at least one chronic medical problem and about one third will experience a late effect that is severe or life threatening.3
These data support a critical need for continuing follow-up of childhood cancer survivors into adult life. 
Only 35% of the survivors understood that serious health problems could result from their past treatment.71
Childhood cancer survivors, an especially high-risk population, seek and receive care from a wide variety of health care professionals, including oncologists, medical and pediatric specialists, surgeons, primary care physicians, gynecologists, advanced practice nurses, psychologists, and social workers. 
Therefore, finding ways to educate survivors and their local health care providers regarding needed follow-up is a priority. 
The Children’s Oncology Group (COG) has developed risk-based, exposure-related guidelines18 specifically designed to direct follow-up care for patients who have completed treatment for pediatric malignancies. Specially tailored patient education materials, known as Health Links, accompany the guidelines, offering detailed information on guideline-specific topics in order to enhance health promotion in this population with specialized health care needs. Examples of screening strategies outlined within the COG are summarized in Table 448-1. The Guidelines and the Health Links are available at http://www.survivorshipguidelines.org. 
Regardless of the setting for follow-up, the first step in any evaluation is to have at hand an outline of the patient’s medical history and, most important, a treatment summary (Table 448-2). Once completed, the treatment summary allows the survivor or his health care provider to interface with the COG’s Long-Term Follow-Up Guidelines to determine recommended follow-up care. 
Table 448-2. Components of a Comprehensive Treatment Summary
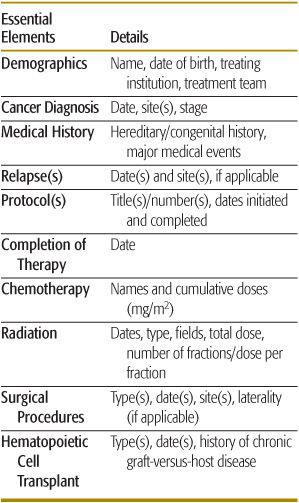
Follow-up should ideally begin at the completion of active therapy, with a documented summary of therapeutic exposures that dictates recommendations within the long-term follow-up guidelines, thus ensuring standardization of care received by the survivors. 
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


