FIGURE 31-1 AP and lateral radiographs of a displaced radial neck fracture in an 8-year-old female.
Radial neck fractures are primarily classified according to anatomic location, translation, and angulation. These fractures have been further classified according to mechanism of injury and degree of displacement.4,8,15Group I injuries refer to those with primarily radial head displacement. Group IA fractures include Salter-Harris type I and II fractures, group IB fractures include Salter-Harris type IV fractures, and group IC fractures involve the proximal radial metaphysis. Group ID and IE injuries refer to radial head displacement that occurs during reduction or dislocation of ulnohumeral dislocations, respectively. Group II injuries denote displacement of the radial neck, either with angular (IIA) or torsional (IIB) deformity. Finally, Group III injuries denote stress injuries of the radial head articular surface, epiphysis, or physis (see Coach’s Corner).
Surgical Indications
While radial neck fractures have tremendous healing potential, excessive angulation or translation will result in loss of forearm rotation and/or elbow flexion-extension. Much of this is due to the constrained articulation of the proximal radioulnar joint (PRUJ) (Figure 31-2). With angulation or translation of the radial head on the radial shaft, cam impingement may occur, resulting in a bony block to forearm rotation.16 Surgical procedures are therefore intended to restore more normal anatomy in hopes of preserving motion and ultimately upper limb function.
Given these considerations, intervention is recommended for excessive fracture displacement. How much angulation and/or translation constitute “too much” is difficult to answer and has not been rigorously studied. Multiple authorities and retrospective studies have suggested that <30 to 45 degrees of angulation and <3 to 4 mm of translation will allow for acceptable functional results.5–8,10,11,17,18 While these radiographic guidelines are helpful, they can be misleading, as often the maximal deformity is not appreciated on static AP and lateral radiographs of the elbow. Furthermore, radiographic remodeling of proximal radial injuries is poor, and multiple studies have demonstrated that radiographic alignment and elbow/forearm motion plateau after 6 months postinjury.9
We favor observation and nonoperative treatment of most of the radial neck fractures with <30-degree angulation, <4-mm translation, congruent radiocapitellar reduction, and at least 80 degrees of forearm pronationsupination. For all other injuries, the simplest and least invasive method of fracture realignment is attempted to achieve the above-stated criteria. In essence, the question is not which injuries require intervention, but rather, which fractures do notrequire further reduction.
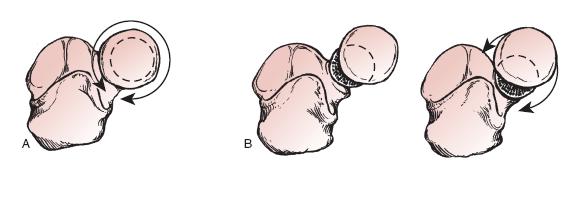
FIGURE 31-2 The effect of displaced radial neck fractures on forearm rotation. (From Beaty JH, Kasser JR. Rockwood & Wilkins Fractures inChildren. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
SURGICAL PROCEDURES
Ain’t no chance if you don’t take it.
—Guy Clark
While a host of surgical procedures can be performed, multiple published studies highlight some common, unifying principles. First, earlier intervention is better.19,20 Fracture reduction becomes much more difficult beyond 7 days postinjury, potentially compromising results. Second, open reduction and fracture stabilization should be deemed a last resort.7,9,21,22 While likely due to selection bias, the literature clearly supports the notion that the need for open reduction portends a worse prognosis. Third, an imperfect but acceptable closed reduction is preferred over an anatomic reduction achieved via open means. Finally, despite surgical skill and radiographic realignment, stiffness does occur, and patients/families should be counseled about the risk of post-traumatic loss of forearm rotation.
In cases where unacceptable alignment and loss of forearm pronation-supination exist, we advocate a step-wise progression of reduction maneuvers, from simple to complex, until a satisfactory clinical and radiographic result is achieved (Table 31.1).
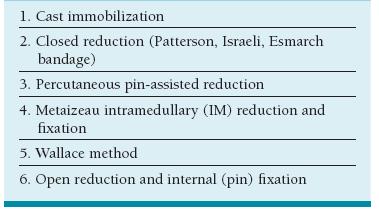
Table 31.1 Progression of treatment options for displaced radial neck fractures
 Closed Reduction
Closed Reduction
A number of closed reduction maneuvers may be utilized for displaced and angulated radial neck fractures, and the pediatric hand and upper extremity surgeon should have experience with all techniques. Typically these maneuvers are most successful in fractures angulated up to 60 degrees with less than complete translation. Given the sustained forces required during these maneuvers, closed reduction should be performed under general anesthesia or adequate conscious sedation with fluoroscopic assistance.
The Patterson technique is perhaps the easiest and most intuitive.23 With the elbow extended and forearm supinated (or in a position that rotates the radial head fragment into its most lateral position), a varus moment is applied across the elbow, and direct pressure is applied to the radial head fragment to effectuate reduction. Fluoroscopic confirmation is made of bony realignment, and passive forearm rotation is assessed. This technique relies upon the intact annular ligament to confer stability to the radial head.
The Israeli technique is performed with the elbow flexed instead of extended.24 With the elbow positioned at 90-degree flexion, the surgeon’s thumb is placed over the radiocapitellar joint, applying medially directed pressure. The forearm is then pronated or supinated to rotate the radial head fragment into the surgeon’s thumb, thereby achieving a congruent reduction against the capitellum and proximal lesser sigmoid notch of the ulna.
Rather than reduce the radial head to the shaft, closed reduction may also be performed by reducing the displaced radial neck and shaft to the head.25 In this technique, the elbow is placed in extension and a varus moment applied to the elbow. The surgeon’s thumbs are then used to push the proximal radial diaphysis laterally.
Finally, failing these maneuvers, an Esmarch bandage may be applied from distal to proximal in the forearm, utilizing the hydraulic effect to achieve reduction. Although not universally successful, this technique may result in surprising improvement in fracture alignment.
 Percutaneous Pin-Assisted Reduction
Percutaneous Pin-Assisted Reduction
When simple, closed reduction maneuvers fail to achieve adequate improvement in fracture alignment, percutaneous pin-assisted reduction may be used (Figure 31-3). Under general anesthesia and fluoroscopic visualization, the elbow is extended and forearm rotated until the radial head fragment is in its most lateral position. A smooth stainless steel Kirschner (K-) wire (typically 5/64″ in diameter) is percutaneously placed along the trajectory of the fracture site. If possible, the forearm is pronated to avoid iatrogenic injury to the posterior interosseous nerve (PIN), which is at risk during this procedure. Commonly, the forearm must be supinated to bring the radial head fragment into appropriate lateral position. In these cases, the pin should enter distally and posteriorly, just off the ulna.
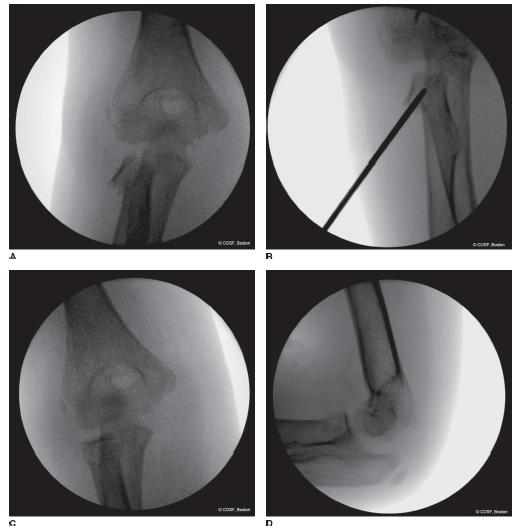
FIGURE 31-3 Percutaneous pin-assisted reduction of a displaced radial neck fracture. A: AP radiograph demonstrates significant angulation, and initial attempts at closed reduction were unsuccessful. B: A percutaneous pin is inserted and used to lever the fracture and translate the radial head fragment. C, D: Subsequent AP and lateral views demonstrate near anatomic reduction.
Two strategies of pin-assisted reduction have been suggested; both are useful. First, the pin may be placed into the fracture site and used to lever the angulated radial head back into position.26,27 Care should be taken not to violate the far periosteal sleeve, for fear of causing greater fracture instability. Second, the blunt end of the pin may be inserted to push directly against the lateral aspect of the radial head fragment, correcting the translation.28 Intraoperative fluoroscopy is used to confirm adequacy of reduction and stability with forearm rotation.
A similar percutaneous technique has been proposed by Wallace et al.29 Again with the elbow extended and forearm positioned to maximally lateralize the radial head fragment, a dorsal incision is made just off the palpable ulna. A small Freer or periosteal elevator is then placed into the interosseous space with care taken not to disturb the periosteum of the ulna. With direct medial pressure applied to the radial head, the elevator is used to push or lever the radial shaft laterally, achieving reduction. Additional stability may be conferred by percutaneous oblique K-wire fixation of the fracture.
 Metaizeau Technique
Metaizeau Technique
First described by and still attributed to Metaizeau, retrograde intramedullary titanium elastic nails may be used to both facilitate reduction and provide internal fixation of displaced radial neck fractures (Figure 31-4).28,30 Under general anesthesia, a small longitudinal incision is made along the distal radial metaphysis, just proximal to the physis. Careful spreading is performed in the subcutaneous tissues to identify and retract the radial sensory nerve and adjacent extensor tendons. Periosteal elevation is performed, and a corticotomy is made with a small drill bit, angled from distal radial to proximal ulnar to facilitate subsequent IM nail passage. A small (typically 2 mm) flexible titanium elastic nail (Synthes, West Chester, PA) is then passed in a retrograde fashion within the IM canal until its tip is just distal to the fracture site. Utilizing a bend in the tip of the IM nail (either provided by the implant design or contoured by the surgeon prior to nail passage), the nail is passed across the fracture and engages the radial head fragment. Rotation of the IM nail will then allow for correction of translation and angulation. The IM nail is then briskly tapped to engage the radial head fragment with care taken not to penetrate the proximal articular surface or overdistract the fracture site. The nail is then bent and cut outside the skin, providing internal fixation while facilitating easy removal in 4 weeks.

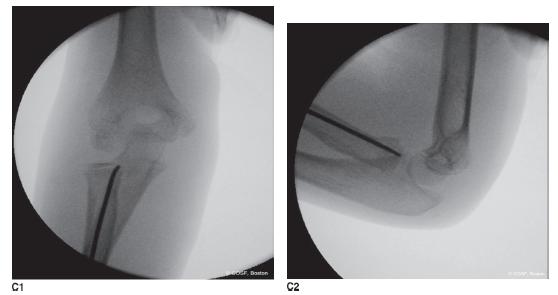
FIGURE 31-4 Reduction and stabilization using flexible elastic IM nails (Metaizeau technique). A: Schematic representation of the technique. B: Injury AP and lateral radiographs of an 8-year-old female after radial neck fracture. C: Intraoperative appearance after IM nail passage. The eccentric position of the tip of the implant in the epiphysis is a result of nail rotation used to correct both translation and angulation. (From Beaty JH, Kasser JR. Rockwood & Wilkins Fractures in Children. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010, with permission.)
 Open Reduction Pinning
Open Reduction Pinning
When closed and percutaneous methods fail, open reduction is required. The radial neck fracture is easily exposed via a Kocher posterolateral approach to the elbow, through the anconeus-extensor carpi ulnaris intermuscular interval. Following arthrotomy and evacuation of the hemarthrosis, the fracture is easily visualized. Reduction is performed under direct visualization with great care taken to avoid excessive stripping of the periosteum and soft tissue attachments to the radial head. After reduction is achieved, stability is assessed under direct and fluoroscopic visualization with forearm rotation and elbow flexion-extension. If there is adequate stability, no internal fixation is needed or utilized, which simplifies the procedure and obviates the need for a second procedure to remove the implants.16 For unstable injuries, fixation can be provided with obliquely placed K-wires, entering the articular margin of the radial head and passing distally across the fracture site, engaging the distal far cortex. These pins are bent and cut beneath the skin, left just outside the joint capsule, and require removal prior to initiation of range-of-motion exercises. Alternatively, if a Metaizeau technique was attempted but failed prior to open reduction, the previously placed IM nail may be used for internal fixation.
We do not advocate the use of transarticular radiocapitellar pinning except in rare circumstances in which the entire radial shaft is displaced anteriorly due to interosseous ligament disruption. Recognition of this unusual situation of separate and unstable displacements of both the radial head and the radial shaft requires careful inspection of the injury and intraoperative fluoroscopic images. If that occurs in the young, a stout smooth pin is placed across the capitellum, anatomically reduced radial head, and into the medullary canal of the anatomically aligned proximal radius. Postoperative immobilization to protect the pin from breakage until removal is mandatory in these rare situations. The option in the older patient is an open reduction internal fixation (ORIF) with a plate and soft tissue repair.
In older patients nearing or at skeletal maturity, or in patients with intra-articular or comminuted radial head and neck fractures, formal ORIF with plate and screw constructs is performed (Figure 31-5). Advantages of plate and screw fixation include the ability to restore articular congruity and provision of rigid fixation to allow early motion.
Under general anesthesia and tourniquet control, a posterolateral approach is made to the radiocapitellar joint, pronating the forearm to avoid iatrogenic injury to the PIN. Arthrotomy is performed and extended distally, allowing for adequate access to the radial shaft while preserving the annular ligament. At times, the annular ligament may require transection for fixation and then repair during closure. Anatomic reduction is performed, and plate and screw fixation applied in the anatomic “safe zone” (see Sidebar). Choice of implant will depend upon the exact fracture pattern. In general, intra-articular marginal fractures of the radial head may be stabilized using countersunk interfragmentary 2.0- or 2.4-mm screws (Synthes, West Chester, PA). For comminuted fractures of the head and neck, locking plates or mini-blade plates may be used to restore both radial head architecture and fixation of the head to the radial shaft. Following reduction and fixation, full elbow flexion-extension and forearm rotation without implant impingement or fracture instability are confirmed. The capsule and soft tissues are closed in layers, and the limb is immobilized with a long-arm bivalved cast or long posterior splint until adequate wound healing. Early range of motion with hinged elbow brace protection is desired to avoid post-traumatic stiffness.
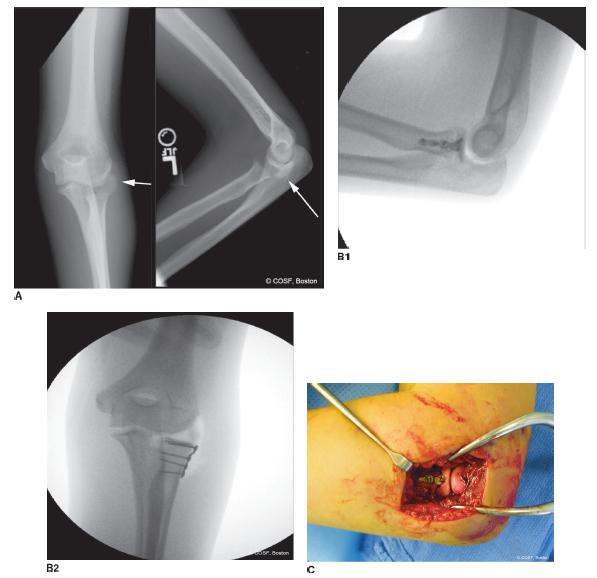
FIGURE 31-5 ORIF of a completely displaced radial neck fracture in a 13-year-old female following a fall off a horse. A: Injury radiographs demonstrate a radial neck fracture; the radial head fragment is completely displaced and rotated. B: Intraoperative fluoroscopic images depicting fracture reduction and internal fixation using plate and screw constructs. C: Intraoperative photograph depicting implant placement in the “safe zone.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 ORIF with Plate
ORIF with Plate