Background
Quantitative fetal fibronectin testing has demonstrated accuracy for prediction of spontaneous preterm birth in asymptomatic women with a history of preterm birth. Predictive accuracy in women with previous cervical surgery (a potentially different risk mechanism) is not known.
Objective
We sought to compare the predictive accuracy of cervicovaginal fluid quantitative fetal fibronectin and cervical length testing in asymptomatic women with previous cervical surgery to that in women with 1 previous preterm birth.
Study Design
We conducted a prospective blinded secondary analysis of a larger observational study of cervicovaginal fluid quantitative fetal fibronectin concentration in asymptomatic women measured with a Hologic 10Q system (Hologic, Marlborough, MA). Prediction of spontaneous preterm birth (<30, <34, and <37 weeks) with cervicovaginal fluid quantitative fetal fibronectin concentration in primiparous women who had undergone at least 1 invasive cervical procedure (n = 473) was compared with prediction in women who had previous spontaneous preterm birth, preterm prelabor rupture of membranes, or late miscarriage (n = 821). Relationship with cervical length was explored.
Results
The rate of spontaneous preterm birth <34 weeks in the cervical surgery group was 3% compared with 9% in previous spontaneous preterm birth group. Receiver operating characteristic curves comparing quantitative fetal fibronectin for prediction at all 3 gestational end points were comparable between the cervical surgery and previous spontaneous preterm birth groups (34 weeks: area under the curve, 0.78 [95% confidence interval 0.64-0.93] vs 0.71 [95% confidence interval 0.64-0.78]; P = .39). Prediction of spontaneous preterm birth using cervical length compared with quantitative fetal fibronectin for prediction of preterm birth <34 weeks of gestation offered similar prediction (area under the curve, 0.88 [95% confidence interval 0.79-0.96] vs 0.77 [95% confidence interval 0.62-0.92], P = .12 in the cervical surgery group; and 0.77 [95% confidence interval 0.70-0.84] vs 0.74 [95% confidence interval 0.67-0.81], P = .32 in the previous spontaneous preterm birth group).
Conclusion
Prediction of spontaneous preterm birth using cervicovaginal fluid quantitative fetal fibronectin in asymptomatic women with cervical surgery is valid, and has comparative accuracy to that in women with a history of spontaneous preterm birth.
Introduction
Preterm birth (PTB) (birth <37 weeks’ completed gestation) is responsible for >1 million neonatal deaths annually. Representing approximately 10% of all deliveries worldwide, rates are continuing to rise. Although history of spontaneous PTB (sPTB) is known to be a limited predictor of subsequent sPTB, currently the 2 best available predictors for sPTB <34 weeks of gestation are cervical length (CL) by transvaginal ultrasound scan (TVS) and cervicovaginal fluid (CVF) fetal fibronectin (FFN).
FFN is an adhesive glycoprotein normally found in the fetal membranes and decidua. As the gestational sac implants and attaches to the interior of the uterus in early pregnancy, presence of FFN in the CVF is regarded as “physiological.” A high concentration of CVF FFN after 18 weeks of gestation may indicate mechanical or inflammatory medicated disruption of the attachment of the membranes to the decidua. Detection of CVF FFN has demonstrated accuracy at predicting sPTB in asymptomatic high-risk women (women who have had a previous sPTB or late miscarriage), and there is increasing evidence that the actual concentration of FFN (quantitative FFN [qFFN]) measured in CVF allows more accurate discrimination of risk of sPTB, although its role in clinical practice is not yet established.
It is well established that women who have undergone invasive cervical surgery (eg, laser loop excision or cone biopsy for premalignant changes) are at more than double the risk of sPTB than the background population, although this may differ with procedure and depth of biopsy. Although used increasingly in clinical practice, the ability of qFFN to predict premature birth in women with previous cervical surgery, compared with women at high risk by virtue of their obstetric history, has never been described and routine FFN testing in asymptomatic women with prior cervical surgery is not recommended by the National Institute for Health and Care Excellence (NICE). It is possible that the etiology underlying sPTB may be different in women with previous cervical surgery who have mechanically shortened cervices, compared with women with a previous sPTB, in whom decidual disruption results in activation of inflammatory pathways. The predictive power of qFFN may be different in these 2 groups.
We hypothesized that qFFN could be used to predict subsequent PTB in women with previous cervical surgery. The primary aim was to compare the predictive value of qFFN in a cohort of primiparous women with previous invasive cervical surgery, compared to women with prior sPTB.
Materials and Methods
This was a predefined prospective masked secondary analysis of a larger observational study of CVF qFFN concentration (ng/mL) in asymptomatic women using commercially available rapid bedside FFN testing (Hologic, Marlborough, MA). Samples were taken between 22 +0 –27 +6 weeks’ gestation. The primary end point of the study was sPTB (including premature prelabor rupture of membranes [PPROM]) with delivery <34 weeks, with secondary end points of delivery <30 and <37 weeks’ gestation. The study was conducted from October 2010 through July 2014 at 5 teaching hospitals in the United Kingdom: Guy’s and St Thomas’ National Health Service Foundation Trust, London, United Kingdom; University College London Hospitals Trust, London; West Middlesex University Hospital National Health Service Trust, London; City Hospitals Sunderland National Health Service Trust, Sunderland, United Kingdom; and Royal Infirmary of Edinburgh National Health Service Lothian, Edinburgh, United Kingdom.
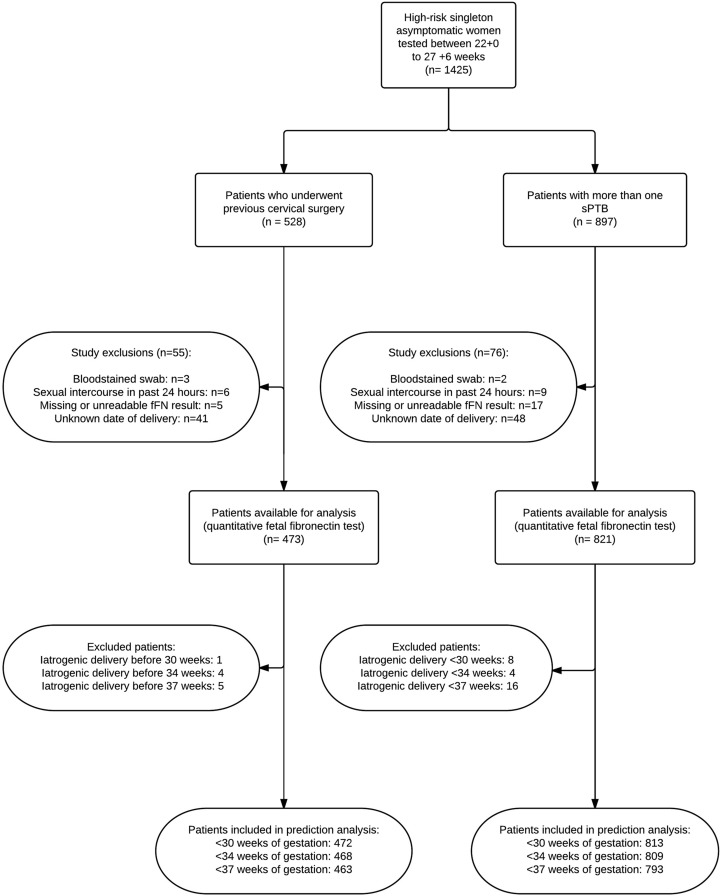
The study was approved by the South East London Research Ethics Committee, and all local research ethics committees associated with participating centers. Informed written consent was obtained from all participants. Gestational age was confirmed by early obstetric ultrasound examination. According to hospital protocol and the licensing recommendations on qFFN testing, women with cervical dilation >3 cm, frank bleeding, or rupture of membranes (on speculum examination) were excluded from the study because of interference with qFFN measurement ( Figure 1 ). Samples that were blood stained or from women who had undergone sexual intercourse or vaginal examination within the past 24 hours were excluded (due to known interference with qFFN measurement ), and the next eligible qFFN test was used if one was available within the gestational age limit of 22–27 +6 weeks.
Categorical TLIQ data (positive/negative) were provided to clinicians, but quantitative 10Q results remained masked (a random result code was generated by the analyzer) until after delivery. Thresholds of 10, 50, 200, and 500 ng/mL were predefined before analysis, based on the literature. A sterile speculum examination was performed, and a polyester swab was inserted for 10 seconds into the posterior fornix of the vagina to collect a sample of CVF. The swab was placed into the test buffer solution and 2 tests were run concurrently. The first aliquot (200 μL) of this solution was analyzed immediately with the conventional qualitative TLIQ rapid FFN analyzer (Hologic). Another aliquot was analyzed with the quantitative rapid 10Q FFN analyzer (Hologic) by placing on a test cassette and inserting into the analyzer; after 10 minutes a numerical result was displayed electronically. All clinicians were trained in the use of the FFN analyzer. After FFN swabs were taken, at the same appointment, CL was measured (in millimeters) using TVS performed by trained staff; the mean of 3 values was used in this analysis. All sonographers were formally trained by the institution’s governance requirements, which included formal assessment prior to accreditation. The mean value was taken to be consistent with our previous evidence. CL measurements were taken and recorded prior to any FFN assay.
From the cohort of asymptomatic high-risk women who met the criteria for analysis (n = 1294), 2 groups of women were selected; primiparous women (no previous pregnancy lasting >14 weeks’ duration) with singleton pregnancies at 22–27 +6 weeks of gestation who had undergone invasive cervical surgery (eg, large loop excision of the transformation zone, cone/loop biopsy) (n = 473) prior to their index pregnancy, and women with singleton pregnancies at 22–27 +6 weeks of gestation, with prior sPTB <37 weeks, PPROM, or miscarriage >14 weeks’ gestation, who had never undergone any cervical surgery (n = 821). Where multiple visits had occurred, the first eligible visit in the gestational age bracket was used. A formal power calculation was not performed as this was a planned subgroup analysis of a previously powered study. We chose not to include multiparous women without prior sPTB into the cervical surgery group to limit the number of variables affecting the risk of PTB.
Descriptive characteristics were calculated for baseline demographics in both groups ( Table 1 ) . Logistic regression and interaction tests were used to assess whether the meaning of the FFN test results varied according to the women’s risk group. Calculations were carried out in software (Stata, Version 11.2; StataCorp, College Station, TX). The performance of qFFN as a predictor of sPTB was tested for different gestational age limits (<34 weeks [primary outcome], 30 weeks, and 37 weeks) and predictive statistics for sPTB were calculated and compared between the previous cervical surgery and previous PTB groups; receiver operating characteristic (ROC) areas were calculated and compared, and sensitivity, specificity, predictive values, likelihood ratios, and relative risk (RR) were assessed at prespecified end points: 10, 50, 200, and 500 ng/mL. The utility of CL measurement following stratification by qFFN category was explored, as well as the utility of qFFN following stratification by the presence and absence of a short cervix (<25 mm). A composite score was developed by using logistic regression for the continuous variables of CL and the log of qFFN concentration to predict prematurity <34 weeks. The composite score was compared with 2 continuous measurements of qFFN and CL using ROC curve analysis. Iatrogenic PTB prior to the gestational age outcome under consideration were excluded from statistical analysis ( Figure 1 ).
| Characteristic | Cervical surgery, n = 473 | Previous sPTB, n = 821 |
|---|---|---|
| Age, y, mean ± SD | 33 ± 4.2 | 32 ± 5.5 |
| Body mass index, kg/m 2 , mean ± SD | 23 ± 3.5 | 26.8 ± 5.6 |
| Ethnicity, n (%) | ||
| European | 411 (87) | 321 (39) |
| African and Afro-Caribbean | 9 (2) | 332 (41) |
| Other | 53 (11) | 168 (20) |
| Smoking history, n (%) | ||
| Current | 10 (2) | 50 (6) |
| Ex-smoker | 127 (27) | 101 (12) |
| Never | 336 (71) | 670 (82) |
| Obstetric history, n (%) | ||
| Any previous pregnancy | 155 (32.8) | 821 (100) |
| Gestation of previous pregnancy, wk (mean ± SD) | 8.1 (2.3) | 32.3 (7.6) |
| Outcome of previous birth, n (%) | ||
| sPTB | – | 566 (69) |
| PPROM | – | 290 (35) |
| Late miscarriage, 16–23 wk | – | 315 (38) |
| Cervical surgery, n (%) | ||
| Cone | 90 (19) | – |
| LLETZ | 370 (78.2) | – |
| Laser | 51 (10.7) | – |
| Trachelotomy | 2 (0.4) | – |
| Other | 34 (7.1) | – |
| Combination | 19 (4) |
Materials and Methods
This was a predefined prospective masked secondary analysis of a larger observational study of CVF qFFN concentration (ng/mL) in asymptomatic women using commercially available rapid bedside FFN testing (Hologic, Marlborough, MA). Samples were taken between 22 +0 –27 +6 weeks’ gestation. The primary end point of the study was sPTB (including premature prelabor rupture of membranes [PPROM]) with delivery <34 weeks, with secondary end points of delivery <30 and <37 weeks’ gestation. The study was conducted from October 2010 through July 2014 at 5 teaching hospitals in the United Kingdom: Guy’s and St Thomas’ National Health Service Foundation Trust, London, United Kingdom; University College London Hospitals Trust, London; West Middlesex University Hospital National Health Service Trust, London; City Hospitals Sunderland National Health Service Trust, Sunderland, United Kingdom; and Royal Infirmary of Edinburgh National Health Service Lothian, Edinburgh, United Kingdom.
The study was approved by the South East London Research Ethics Committee, and all local research ethics committees associated with participating centers. Informed written consent was obtained from all participants. Gestational age was confirmed by early obstetric ultrasound examination. According to hospital protocol and the licensing recommendations on qFFN testing, women with cervical dilation >3 cm, frank bleeding, or rupture of membranes (on speculum examination) were excluded from the study because of interference with qFFN measurement ( Figure 1 ). Samples that were blood stained or from women who had undergone sexual intercourse or vaginal examination within the past 24 hours were excluded (due to known interference with qFFN measurement ), and the next eligible qFFN test was used if one was available within the gestational age limit of 22–27 +6 weeks.
Categorical TLIQ data (positive/negative) were provided to clinicians, but quantitative 10Q results remained masked (a random result code was generated by the analyzer) until after delivery. Thresholds of 10, 50, 200, and 500 ng/mL were predefined before analysis, based on the literature. A sterile speculum examination was performed, and a polyester swab was inserted for 10 seconds into the posterior fornix of the vagina to collect a sample of CVF. The swab was placed into the test buffer solution and 2 tests were run concurrently. The first aliquot (200 μL) of this solution was analyzed immediately with the conventional qualitative TLIQ rapid FFN analyzer (Hologic). Another aliquot was analyzed with the quantitative rapid 10Q FFN analyzer (Hologic) by placing on a test cassette and inserting into the analyzer; after 10 minutes a numerical result was displayed electronically. All clinicians were trained in the use of the FFN analyzer. After FFN swabs were taken, at the same appointment, CL was measured (in millimeters) using TVS performed by trained staff; the mean of 3 values was used in this analysis. All sonographers were formally trained by the institution’s governance requirements, which included formal assessment prior to accreditation. The mean value was taken to be consistent with our previous evidence. CL measurements were taken and recorded prior to any FFN assay.
From the cohort of asymptomatic high-risk women who met the criteria for analysis (n = 1294), 2 groups of women were selected; primiparous women (no previous pregnancy lasting >14 weeks’ duration) with singleton pregnancies at 22–27 +6 weeks of gestation who had undergone invasive cervical surgery (eg, large loop excision of the transformation zone, cone/loop biopsy) (n = 473) prior to their index pregnancy, and women with singleton pregnancies at 22–27 +6 weeks of gestation, with prior sPTB <37 weeks, PPROM, or miscarriage >14 weeks’ gestation, who had never undergone any cervical surgery (n = 821). Where multiple visits had occurred, the first eligible visit in the gestational age bracket was used. A formal power calculation was not performed as this was a planned subgroup analysis of a previously powered study. We chose not to include multiparous women without prior sPTB into the cervical surgery group to limit the number of variables affecting the risk of PTB.
Descriptive characteristics were calculated for baseline demographics in both groups ( Table 1 ) . Logistic regression and interaction tests were used to assess whether the meaning of the FFN test results varied according to the women’s risk group. Calculations were carried out in software (Stata, Version 11.2; StataCorp, College Station, TX). The performance of qFFN as a predictor of sPTB was tested for different gestational age limits (<34 weeks [primary outcome], 30 weeks, and 37 weeks) and predictive statistics for sPTB were calculated and compared between the previous cervical surgery and previous PTB groups; receiver operating characteristic (ROC) areas were calculated and compared, and sensitivity, specificity, predictive values, likelihood ratios, and relative risk (RR) were assessed at prespecified end points: 10, 50, 200, and 500 ng/mL. The utility of CL measurement following stratification by qFFN category was explored, as well as the utility of qFFN following stratification by the presence and absence of a short cervix (<25 mm). A composite score was developed by using logistic regression for the continuous variables of CL and the log of qFFN concentration to predict prematurity <34 weeks. The composite score was compared with 2 continuous measurements of qFFN and CL using ROC curve analysis. Iatrogenic PTB prior to the gestational age outcome under consideration were excluded from statistical analysis ( Figure 1 ).
| Characteristic | Cervical surgery, n = 473 | Previous sPTB, n = 821 |
|---|---|---|
| Age, y, mean ± SD | 33 ± 4.2 | 32 ± 5.5 |
| Body mass index, kg/m 2 , mean ± SD | 23 ± 3.5 | 26.8 ± 5.6 |
| Ethnicity, n (%) | ||
| European | 411 (87) | 321 (39) |
| African and Afro-Caribbean | 9 (2) | 332 (41) |
| Other | 53 (11) | 168 (20) |
| Smoking history, n (%) | ||
| Current | 10 (2) | 50 (6) |
| Ex-smoker | 127 (27) | 101 (12) |
| Never | 336 (71) | 670 (82) |
| Obstetric history, n (%) | ||
| Any previous pregnancy | 155 (32.8) | 821 (100) |
| Gestation of previous pregnancy, wk (mean ± SD) | 8.1 (2.3) | 32.3 (7.6) |
| Outcome of previous birth, n (%) | ||
| sPTB | – | 566 (69) |
| PPROM | – | 290 (35) |
| Late miscarriage, 16–23 wk | – | 315 (38) |
| Cervical surgery, n (%) | ||
| Cone | 90 (19) | – |
| LLETZ | 370 (78.2) | – |
| Laser | 51 (10.7) | – |
| Trachelotomy | 2 (0.4) | – |
| Other | 34 (7.1) | – |
| Combination | 19 (4) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


