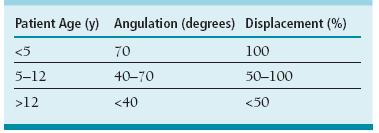
FIGURE 26-1 A: Anteroposterior radiograph of the left shoulder demonstrates a displaced proximal humeral physeal fracture with translation and varus angulation. B: Transthoracic “Y” view. C: Axillary view obtained intra-operatively highlights the translation and apex anterior angulation of the injury.
Clinical Evaluation
Take off the blinders. You have to see opportunity before you can seize it.
—Greg Hickman
Patients typically present with pain, swelling, ecchymosis, and limited shoulder and elbow motion. The affected extremity is usually held in adduction and internal rotation, with fullness or deformity about the injury site. A comprehensive physical examination should rule out concomitant neurovascular injury. Deltoid function and sensibility along the lateral aspect of the shoulder should be checked in cases of proximal humerus fractures to rule out concomitant axillary nerve injury. Careful assessment of radial nerve function (first dorsal web sensation, wrist extensor, and thumb and digital extensor motor function) is imperative in cases of humeral shaft fractures to assess for radial nerve palsy.
Plain radiographs will confirm the diagnosis. Recommended for evaluation are anteroposterior (AP) lateral (scapular Y view), and axillary views of the proximal humerus. While axillary views are sometimes difficult to obtain, they are necessary to quantify displacement and angulation, which is often apex anterior (Figure 26-1C). In situations where an axillary view cannot be obtained, an apical oblique view of the shoulder (AP radiograph with 45 degrees of caudal tilt) may be useful. Pathologic fractures in the setting of unicameral bone cysts, aneurysmal bone cysts, or other benign and malignant conditions commonly occur in the proximal humerus. Radiographs should be carefully evaluated for underlying bony abnormalities, and further diagnostic workup should be considered prior to any surgical intervention in cases of diagnostic unknowns.
Understanding of the normal appearance of the secondary centers of ossification in the proximal humerus is imperative for accurate diagnosis. The proximal humeral epiphysis becomes radiographically apparent at 6 months of age; for this reason, infantile proximal humerus fractures require other imaging modalities (e.g., ultrasound, magnetic resonance imaging (MRI)) for adequate visualization. The greater and lesser tuberosities appear by 3 and 5 years of age, respectively. The tuberosities coalesce between 5 and 7 years and fuse with the humeral epiphysis at 7 to 13 years of age. Unlike adults, pediatric proximal humerus fractures rarely require computed tomography (CT) scans to identify fracture pattern and guide treatment.
Proximal humerus fractures are characterized according to their anatomic location and displacement. Physeal fractures are typically classified according to the Salter-Harris classification.17 In addition, Neer and Horwitz18 have proposed a classification based on the amount of radiographic displacement (Table 26-1).
Radiographic evaluation of humeral diaphyseal injuries is straightforward and based upon AP and lateral views of the entire humerus. The shoulder and elbow joints should be visualized to confirm appropriate joint alignment and rule out the rare associated floating elbow or fracture dislocation. Humeral shaft fractures are similarly classified according to their anatomic location, displacement, and angulation.
Surgical Indications
The time is always right to do what is right.
—Martin Luther King, Jr.
As the proximal physis contributes approximately 80% of the longitudinal growth of the humerus, there is great remodeling potential of displaced proximal humerus fractures in skeletally immature patients. For this reason, the majority of proximal humerus fractures may be successfully treated nonoperatively. Surgical treatment is typically considered in older patients with fracture displacement or angulation beyond what might be expected to spontaneously correct with continued skeletal growth (Neer and Horwitz grade 3 and 4 injuries) or in those patients with concomitant musculoskeletal or neurovascular injury.
Traditional guidelines have been proposed regarding what constitutes “acceptable” proximal humeral deformity amenable to nonoperative care6,14,18 (Table 26-2). In cases of unacceptable displacement in an older child or adolescent, closed reduction (CR) and/or surgical stabilization of the proximal humerus fracture may provide the best long-term outcome. Current indications for surgical treatment with internal or percutaneous skeletal fixation include open fractures, fractures associated with vascular compromise, fractures in the multiple-trauma patient, displaced intra-articular fractures, and unstable or unacceptable fracture displacement in an older child or adolescent.7 In the older child, if the proximal aspect of the greater tuberosity impinges on the acromion with attempted elevation, and the child is too skeletally mature to remodel, then closed reduction percutaneous pinning (CRPP) or intramedullary fixation is performed. It is our preference to use percutaneous pins for displaced physeal fractures and intramedullary fixation for metaphyseal injuries.
Table 26.1 Classification of pediatric proximal humerus fractures
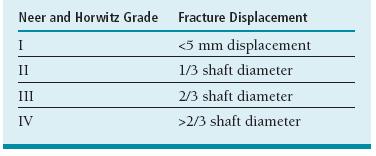
From Neer CS II, Horwitz BS. Fractures of the proximal humeral epiphysial plate. Clin Orthop Relat Res. 1965;41:24–31.
Table 26.2 Guidelines for “acceptable” alignment of proximal humerus fractures in children and adolescents
From Sherk HH, Probst C. Fractures of the proximal humeral epiphysis. Orthop Clin North Am. 1975;6:401–413, Beaty JH. Fractures of the proximal humerus and shaft in children. Instr Course Lect. 1992;41:369–372, and Neer CS II, Horwitz BS. Fractures of the proximal humeral epiphysial plate. Clin Orthop Relat Res. 1965;41:24–31.

FIGURE 26-2 Open humeral shaft fracture associated with a floating elbow injury in a 10-year-old female after a motor vehicle collision. A: AP radiograph of the humerus depicting an open humeral diaphysis fracture. B: Lateral radiograph. C: Postoperative radiograph of the right humerus after ORIF through the traumatic lateral wound. D: Radiograph of the forearm fracture after open plating of the radius, sparing the distal physis.
Similar considerations dictate humeral shaft fracture care. Due to the remodeling potential as well as the compensatory motion of the glenohumeral and scapulothoracic joints, considerable deformity is functionally and aesthetically acceptable. Indeed, up to 30 degrees of angulation, 2 cm of bayonet apposition, and 20 degrees of internal rotation are deemed acceptable. Surgical treatment is indicated in cases of excessive deformity, open fractures, fractures with associated vascular injury, floating elbow injuries, and the multiple-trauma patient (Figure 26-2).
SURGICAL PROCEDURES
A host of surgical techniques are available for reduction and stabilization of proximal humerus and shaft fractures. All are effective, and all should be in the quiver of the pediatric hand and upper extremity surgeon. The decision regarding which method of exposure, reduction, and fixation is dependent upon an array of individual patient factors, including skeletal maturity, injury pattern, and associated bony or soft tissue injuries. In general, the simplest and least invasive technique that can achieve the desired result should be selected.
Fracture reduction with percutaneous or internal fixation offers a number of theoretical advantages. First, bony fixation maintains fracture reduction, decreasing the risk of late displacement that may occur with immobilization alone. In addition, anatomic fracture reduction lessens the risk of shoulder impingement and loss of function. Furthermore, the fracture stability provided by skeletal fixation lessens pain and allows for a more expedient return to activities of daily living. Finally, in cases of severely displaced physeal fractures, anatomic reduction theoretically reduces the risk of post-traumatic growth disturbance.
Disadvantages include all the attendant risks of surgical intervention. In particular, there is a risk of a pin tract infection and/or iatrogenic axillary nerve injury with percutaneous pinning techniques. Finally, in cases where intramedullary fixation is utilized or where pins are cut beneath the skin, a second anesthetic is required for implant removal.
 Nonoperative Care
Nonoperative Care
Nonoperative care is appropriate and effective for the majority of proximal humerus and humeral diaphyseal fractures. For proximal humerus fractures, simple sling immobilization is sufficient, with the expectation for bony healing in 4 to 6 weeks. In cases of diaphyseal humerus fractures with acceptable alignment, initial sling or coaptation splint immobilization followed by Sarmiento fracture bracing is effective19 (Figure 26-3).
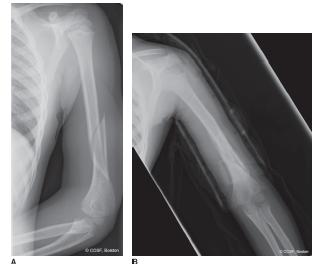
FIGURE 26-3 Nonoperative treatment of humeral shaft fracture. A: Injury AP radiograph of a 6-year-old male with an oblique distal third humeral diaphyseal fracture. B: AP radiograph after 1 month of Sarmiento fracture bracing. The alignment is well preserved, and early fracture healing is noted.
 Closed Reduction and Pinning of Proximal Humerus Fracture
Closed Reduction and Pinning of Proximal Humerus Fracture
You must not only aim right, but draw the bow with all your might.
—Henry David Thoreau
CRPP is commonly utilized in the treatment of displaced proximal humerus fractures in older children and adolescents. CR maneuvers must counteract the typical deforming forces imparted on the fracture fragments to be successful. In proximal fractures, the humeral head fragment typically abducts, flexes, and externally rotates, due to the action of the rotator cuff muscles. Conversely, the diaphyseal fracture fragment is displaced proximally by the deltoid and adducted and internally rotated by the pectoralis major. While successful CR may be achieved in many cases, up to 50% of patients will demonstrate a loss of reduction with immobilization alone.8,18 For this reason, percutaneous pinning is added to maintain alignment during the healing process.
The patient is placed supine on a radiolucent table or in the modified beach chair position (Figure 26-4). We prefer the modified beach chair position, as it allows full shoulder motion and facilitates intraoperative fluoroscopy in the AP and axillary projections. Due to the deforming muscle forces, CR is generally facilitated by general anesthesia with muscle indentlysis. The entire shoulder and ipsilateral upper extremity is prepped and draped to facilitate fracture manipulation and fixation. Longitudinal traction followed by flexion, abduction, and external rotation of the humeral diaphysis is applied, reversing the deformity and reducing the distal fragment to the proximal fragment. Alternatively, shoulder abduction followed by forward flexion to 90 degrees followed by external rotation may be utilized to achieve reduction. Intraoperative fluoroscopy in orthogonal planes is used to assess the adequacy of fracture reduction. In situations where an adequate CR cannot be achieved, usually due to soft tissue interposition (biceps tendon, periosteum), open reduction is required. The standard deltopectoral approach is used to expose the fracture site, clear any interposed soft tissue, and restore anatomic alignment. Direct visualization as well as intraoperative fluoroscopy is utilized to confirm reduction.
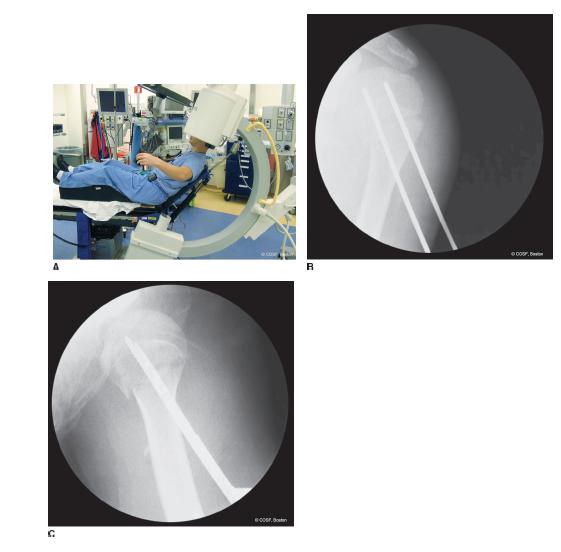
FIGURE 26-4 CRPP of displaced proximal humerus fractures. A: Modified beach chair positioning allows for fluoroscopic AP and axillary views of the proximal humerus. B: Intraoperative image depicting reduction and placement of two smooth K-wires. C: Intraoperative axillary view.
Once reduction is achieved, percutaneous skeletal fixation using smooth 0.0625″ or 5/64″ K-wires is performed. Stab incisions are made laterally at the level of the deltoid insertion through the dermis only. While this starting position necessitates a steeper angle for pin placement, this inferior starting position lessens the risk of iatrogenic axillary nerve injury.20 In adults, the starting point should be >8 cm below the acromion to avoid injuries to the axillary nerve. Blunt dissection is performed down to the level of the lateral cortex of the humeral diaphysis. Two K-wires are then passed from distal-lateral to proximal-medial, traversing the fracture site. A larger drill hole in the lateral cortex often makes exact positioning of the K-wires in the head easier. The risk is penetrating the joint cartilage or neighboring neurovascular structures. Exact placement of stable K-wires in the humeral head by CRPP can be harder than you would think. Pins should be placed parallel or slightly divergent to one another to confer rotational stability, and, again, care is taken not to violate the articular surface of the humeral head.
In cases of marked fracture instability, reduction may be lost when the arm is brought down into the adducted and internally rotated position. In these situations, it may be necessary to place the K-wires with the shoulder abducted, flexed, and externally rotated. As this is technically difficult, the K-wires may be started in the distal lateral humeral diaphysis, stopping short of the fracture site; fracture reduction may then be performed and the preplaced wires passed across the fracture into the proximal humeral segment. Alternatively, a “greater tuberosity pin” may be placed first and used as a joystick to reduce the proximal fracture fragment and provide provisional stability.
Intraoperative fluoroscopy is performed to confirm appropriate pin placement and fracture alignment; ranging the shoulder under live fluoroscopy will demonstrate fracture stability. If additional fixation is required, a third K-wire may be passed proximal-lateral to distal-medial from the greater tuberosity to the distal medial humeral cortex.
After the K-wires have been placed and fracture stability confirmed, the pins may be bent and cut outside the skin or cut beneath the skin. A bulky sterile bandage is applied, followed by a sling and swathe. In larger adolescents, more noncompliant patients, and/or more unstable fractures, an abduction brace or pillow can be used to impart additional stability and protection.
 Intramedullary Rodding of Proximal Humerus Fracture
Intramedullary Rodding of Proximal Humerus Fracture
Intramedullary fixation using flexible titanium or stainless steel nails has also been utilized to stabilize proximal humerus as well as humeral diaphyseal fractures.9,21–23 This technique is familiar to pediatric orthopaedists, and the principles echo those used in forearm and femur fracture fixation.
Again, under general anesthesia in the supine or beach chair position, closed fracture reduction is performed (Figure 26-5). Following bony realignment, preindenttion is made for intramedullary nail insertion. A longitudinal incision is made along the lateral column of the distal humerus at the level of the superior aspect of the olecranon fossa. Blunt soft tissue dissection is performed through the subcutaneous tissues down to the level of the distal humerus. With adequate soft tissue protection, a 3.2 or 4.5 mm drill bit is used to create a cortical window in the lateral column; care is taken to create this starting hole obliquely from distal-lateral to proximal-medial to facilitate subsequent nail passage. Appropriately sized flexible titanium nails (typically 2.5 to 4 mm in diameter) are then prebent; if both nails are to be passed via a lateral entry point, one nail is bent in the shape of a gentle “C” and the other in the shape of a lazy “S” to allow for some divergence of the nail ends in the proximal fracture fragment. Nails are then passed through the lateral column entry site, up the intramedullary canal of the humerus, across the fracture site, and into the proximal fracture fragment. Typically, the nails must be impacted into the proximal humerus with care to avoid distraction at the fracture site. Translation or angulation at the fracture site may be corrected with nail rotation once the proximal fragment is engaged. Intraoperative fluoroscopy is utilized to confirm nail placement, fracture alignment, and stability. Nails are then cut beneath the skin with the distal ends prominent to allow for subsequent removal. Wound(s) are then closed, the dressing applied, and the upper extremity placed in sling-and-swathe immobilization.
Several variations of intramedullary nail fixation for pediatric proximal humerus fractures have been used with success. Although there have been reports of successful healing and maintenance of reduction with the use of a single nail, it is our preference to use two nails.9 Furthermore, while the technique of dual nail placement via lateral column entry is described here, nails may be safely and effectively placed via medial column, medial epicondyle, or posterior humeral entry sites. In cases of posterior nail insertion, a small posterior triceps-splitting approach is used to expose the humeral cortex just superior to the olecranon fossa. Our preference is to use the lateral column entry site to avoid complications of stiffness, nail migration, and ulnar nerve injury seen with posterior and medial entry respectively.
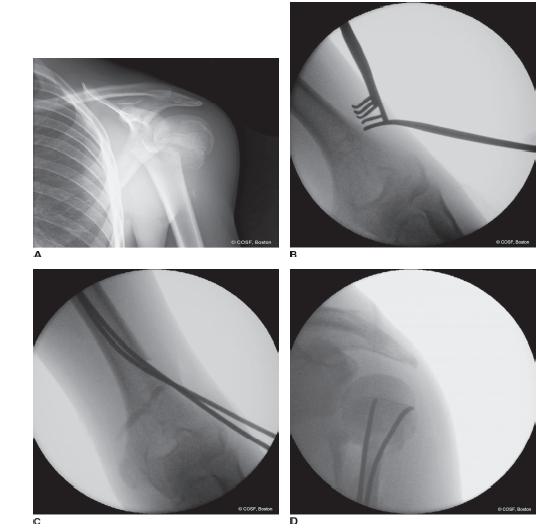
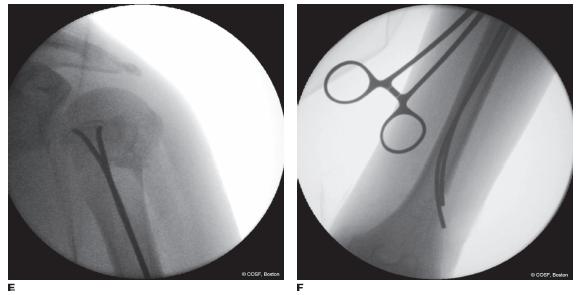
FIGURE 26-5 Intramedullary fixation of proximal humerus fractures. A: AP radiograph depicting a displaced proximal humerus fracture. B: Intraoperative fluoroscopic image depicting preindenttion of the nail entry site along the lateral column of the distal humerus. C, D: Precontoured flexible titanium nails are then passed into the intramedullary canal of the humerus, engaging the humeral head fragment across the fracture site. E: Rotation of the implants may be used to correct residual translation and angulation. F: Nails are cut beneath the skin and allowed to recoil against the lateral column, avoiding soft tissue irritation while providing access for subsequent removal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


