Protocol for Delivery Room Management of Hydrops
INTRODUCTION
The transition to breathing for the hydropic infant after birth is a particularly tenuous situation. The delivery room management of hydrops can be a critical period of intervention and a highly intense event with a critically sick infant requiring extensive resuscitation and multiple procedures immediately following delivery.1 The basic principles for resuscitation of high-risk newborns still apply. However, because of the possibility of pleural effusions and ascites in hydrops, the team must be prepared to perform two additional procedures that are not commonly performed by delivery room personnel: thoracentesis and paracentesis. This chapter outlines the overall approach to delivery room management for hydrops and provides detailed descriptions of these two procedures.
PREPARATION FOR DELIVERY
Prenatal Counseling
Prior to delivery, appropriate counseling of the family may involve discussion of the etiology of hydrops, if known, and the prognosis.2 In some situations, hydrops may be an end-stage process, and comfort care after delivery may be a reasonable alternative to intensive resuscitation. This decision can be made prior to delivery with informed consent of the parents, allowing them to hold the infant soon after birth and to provide comfort. Prognosis in hydrops is dependent on the etiology, although the etiology may be indeterminate in about a quarter of cases. The prognosis can be discussed prior to delivery if time is available.
If resuscitation is planned, counseling of the parents should involve explaining the procedures that may be carried out in the delivery room. The delivery room will be a busy and intense environment; thus, preparation of the parents may help to relieve some degree of anxiety.
Delivery Room Staff
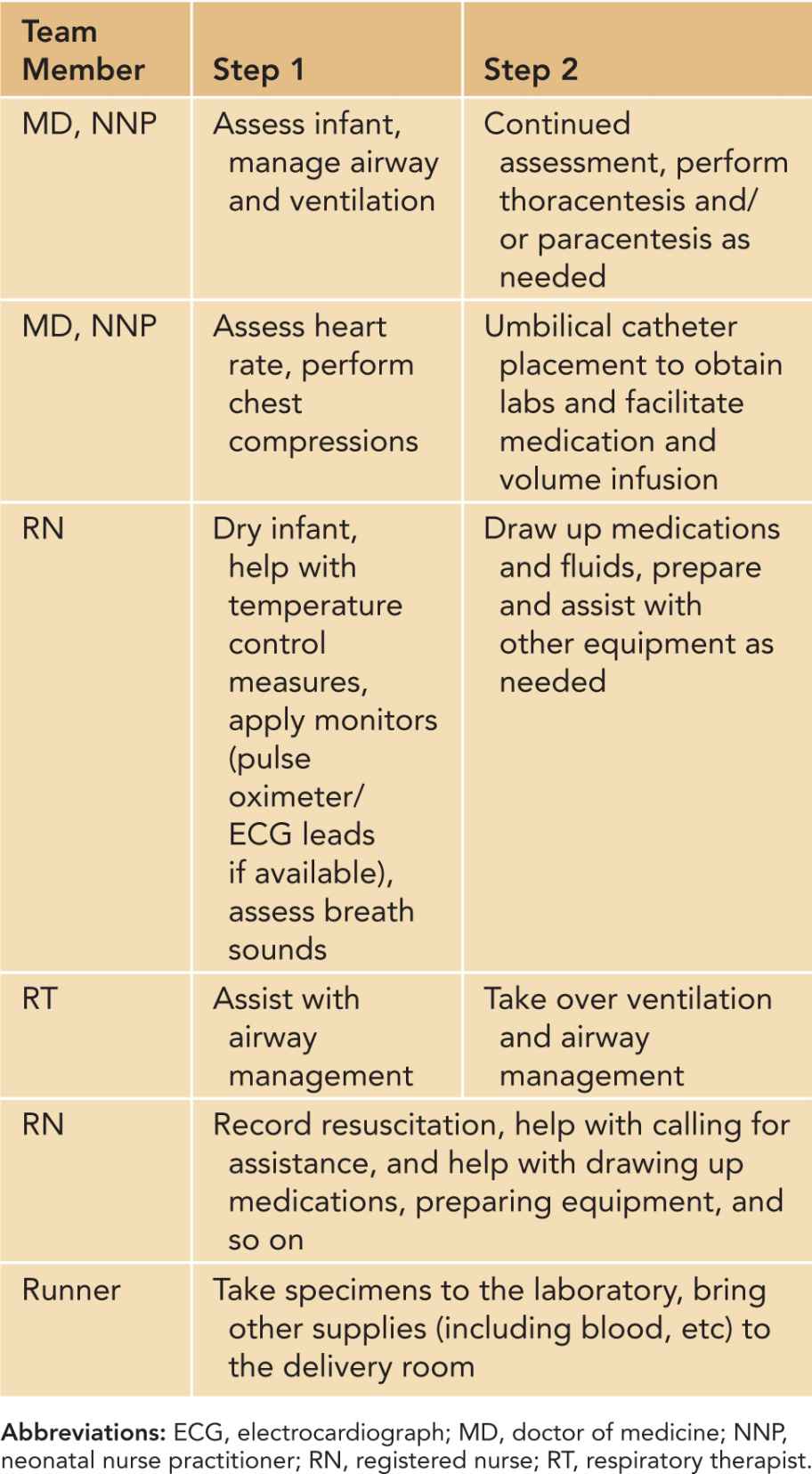
The makeup of the resuscitation team may vary by institution. Table 68-1 offers a potential delineation of roles that can be modified depending on availability of specific clinical personnel. The expected duties of clinicians may vary by institution, and this table can serve as a template for developing protocols that are more specific. However, it should be noted that the list of tasks is extensive, and a team consisting of at least 5, and possibly more, members is not an unreasonable expectation for this scenario.
Table 68-1 Roles of Team Members in Delivery Room Management of Hydrops
Delivery Room Equipment
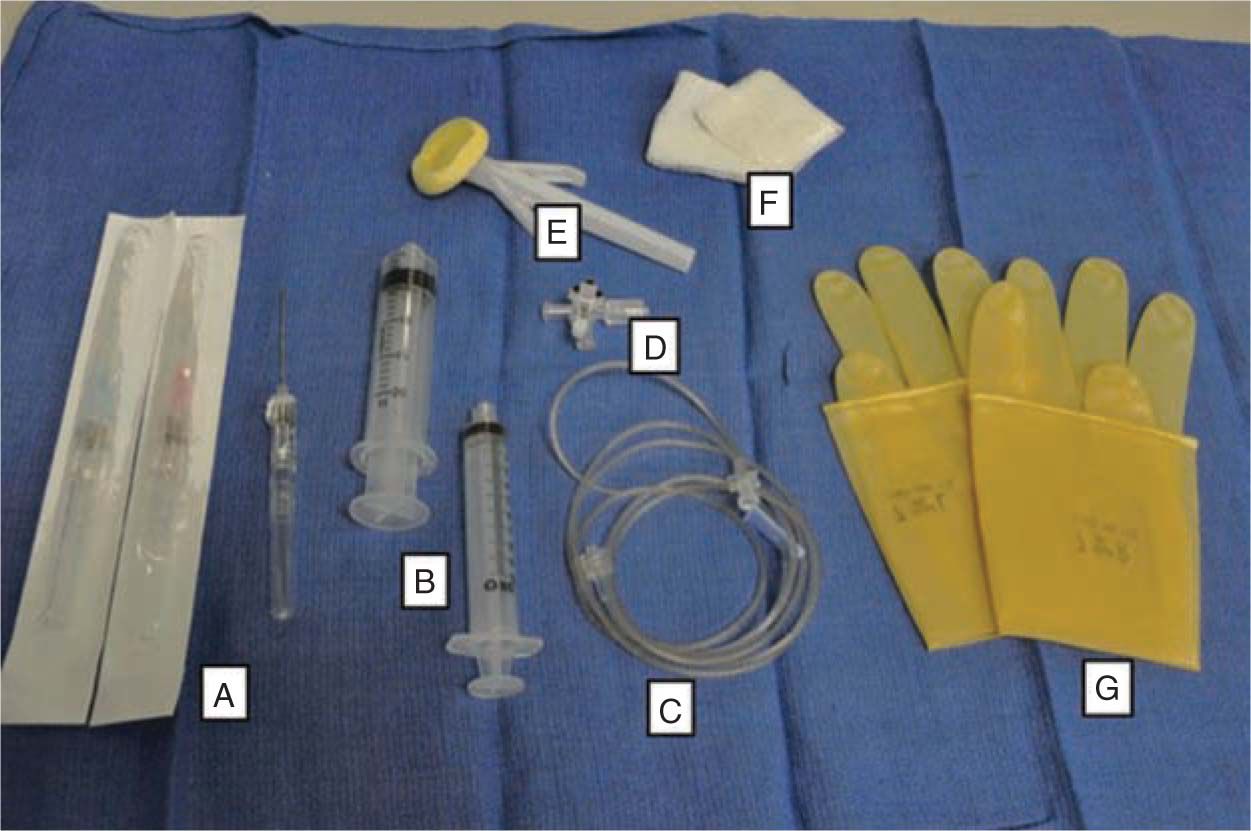
The equipment necessary for delivery room management of an infant with hydrops will include the basic equipment necessary for resuscitation of any high-risk infant, including a radiant warmer, and equipment for intubation and airway management. Furthermore, as the likelihood for volume resuscitation and medications may be high, supplies for umbilical line placement should be readily available. Difficulty with ventilation in hydrops may lead to the need for paracentesis or thoracentesis, and supplies for these procedures should also be prepared. The typical equipment used for these procedures is shown in Figure 68-1. A list of other equipment that may be used in the resuscitation of hydropic infants is provided in Table 68-2.
Table 68-2 Equipment That May Be Used in Delivery Room Management of Infant With Hydrops
Warming equipment
Oxygen saturation probe/pulse oximeter/electrocardiograph monitor
Equipment for intubation/airway management
Equipment for intubation/airway management
Equipment for umbilical line placement
Equipment for blood transfusion (if indicated)
Equipment for paracentesis or thoracentesis
Transducing equipment/defibrillator/pacing equipment (if indicated)
Collection containers for laboratory evaluation
FIGURE 68-1 Supplies needed for paracentesis or thoracentesis: A, 18- to 20-gauge intravenous catheter with stylet; B, syringe(s); C, connection tubing; D, 3-way stopcock; E, sterile prep; F, sterile gauze; G, sterile gloves.
AIRWAY/BREATHING
As in all neonatal resuscitation, airway and breathing should be the first priority. Assessment and management should generally follow the procedures as described previously. However, there are several special considerations that can complicate management of the airway and ventilation in an infant with hydrops.
Edema
There may be a significant amount of soft tissue edema caused by hydrops that can distort both external and internal anatomy.
Congenital Airway Malformation
Congenital Airway Malformation may be a possible etiology of hydrops. Therefore, it is important that a clinician who is skilled in intubation be assigned the task of airway management. A smaller endotracheal tube may be necessary if there is significant edema. If airway abnormalities are expected, involvement of a pediatric otolaryngologist or anesthesiologist in the delivery room may be warranted.
Asphyxia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree