Steer (2005) observed that signs of immaturity at birth and shorter than average gestational length have an unusually high incidence in Homo sapiens compared with other mammals. This has been attributed to the development of a narrow pelvis for bipedal gait, coupled with evolution toward a large brain and head that is associated with language and social skill acquisition. It is hypothesized that this combination results in a relatively high incidence of obstructed labor, which favors an evolutionary trend toward shorter gestation and thus an earlier birth.
As previously noted, if infant mortality rates are used as the outcome of interest, the data in Table 42-1 suggest that optimal pregnancy outcomes vis-à-vis prematurity are achieved at 39 weeks’ gestation. Is the 39-week threshold correct for defining pathologically shortened human gestation? For example, if neonatal death is used as the outcome of interest, delivery at 380/7 through 386/7 weeks is equivalent to delivery at 39 weeks (McIntire, 2008). Similarly, if respiratory morbidity is used as the outcome of interest, 380/7 through 386/7 weeks is equivalent to 39 weeks (Consortium on Safe Labor, 2010). These examples suggest that shortened human gestation with regard to prematurity is birth before 380/7 weeks rather than before 390/7 weeks.
A consequence of defining optimal pregnancy outcomes to occur at 39 weeks has been the concern that some births before 39 weeks may be unnecessary, that is, intentional deliveries not based on medical indications. Indeed, Bailit (2012) observed, “The dangers of delivering a newborn before 39 weeks for nonmedical reasons have become increasingly clear.” The evidence that unnecessary deliveries are occurring before 39 weeks in the United States is not robust. Martin (2009b) used birth certificate data to analyze late preterm births between 1990 and 2006. The rate of infants born late preterm increased 20 percent during this time period. Moreover, the percentage of late preterm births for which labor was induced more than doubled between 1990 and 2006, climbing from 7.5 to 17.3 percent. The percentage of late preterm births delivered by cesarean also rose substantially, from 23.5 to 34.3 percent. Such increases in obstetrical interventions inevitably raise the specter of medically unnecessary interventions.
Reddy (2009) used 2001 United States birth certificate data to examine delivery indications for late preterm birth. A total of 23 percent of late preterm births had no recorded indication for delivery. Some of the factors significantly increasing the chance of no recorded indication were older maternal age, non-Hispanic white mother, and ≥ 13 years of education. Factors such as these raised the possibility that patient factors—as opposed to medical factors—were playing a role in late preterm births without a specified medical indication in the birth certificate. But Bailit (2012) has described the complexities of ascertaining the indications for delivery.
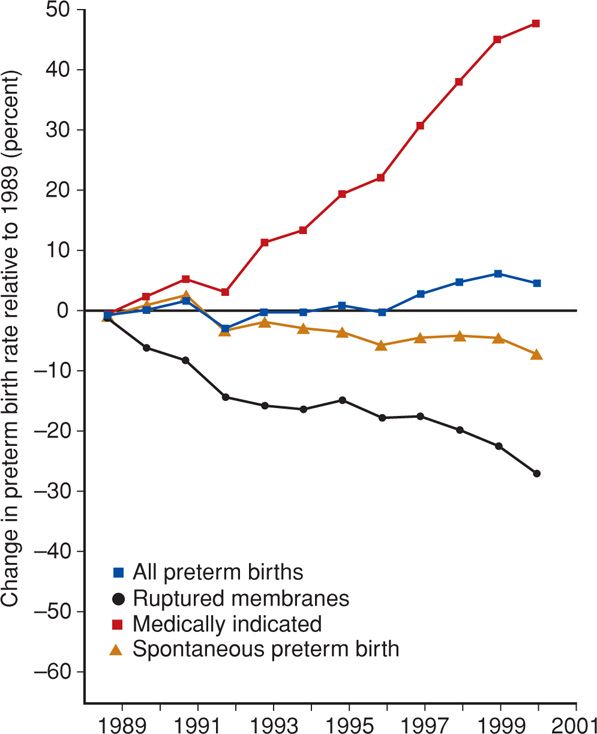
In contrast, an analysis of the indications for delivery of 21,771 late preterm births at Parkland Hospital using a research data set showed that 99.8 percent of such births were indicated and that 80 percent were due to idiopathic preterm labor or preterm spontaneously ruptured membranes. Indeed, and as shown in Figure 42-1, medically indicated preterm births are largely responsible for the increase in preterm births in the United States.
FIGURE 42-1 Rates of births < 37 weeks in the United States from 1989 to 2001. (Redrawn from Ananth, 2005, with permission.)
Undoubtedly, unnecessary obstetrical interventions are occurring before 38 or 39 weeks’ gestation, but the magnitude of this problem is unclear at this time. Caution is urged before assuming that obstetrical interventions before 38 or 39 weeks are unnecessary. For example, Koopmans and colleagues (2009) randomized women with mild preeclampsia or gestational hypertension at 36 weeks’ gestation to induction of labor versus expectant management. This trial showed that delivery at 37 weeks was better for women and their newborns compared with later delivery. The American College of Obstetricians and Gynecologists (2013b) also recommends caution before withholding indicated intervention.
TRENDS IN PRETERM BIRTH RATES
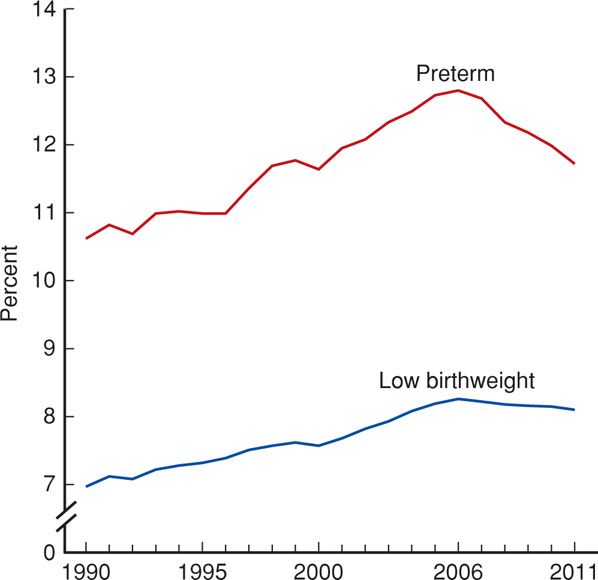
The percentage of preterm births increased 36 percent from 9.4 percent in 1984 to a high of 12.8 percent in 2006 (Mathews, 2013). Since 2006, however, the trend has reversed, and the percentage of preterm births declined to 11.7 percent in 2011 (Figure 42-2). This decline in the percentage of preterm births occurred for both the early—less than 34 weeks—and later preterm periods (Hamilton, 2012). Although the lowest level in more than a decade, the 2011 preterm birth rate is still higher than rates reported during the 1980s and most of the 1990s.
FIGURE 42-2 Preterm and low-birthweight rate: United States, final 1990 to 2010 and preliminary 2011. (Redrawn from Hamilton, 2012.)
Is the decrease in preterm births shown in Figure 42-2 real? It could be argued that the decrease since 2006 is a result of changes in the birth certificate that is used to compute United States preterm birth rates. In 2003, a revised birth certificate intended to expand the collection of clinical information was introduced in the United States. Implementation depends on the rapidity with which the various states transitioned to the new version. For example, by 2008, the revised birth certificate had been implemented in 27 states representing 65 percent of all 2008 births (Osterman, 2011). This “trickle in” implementation coincides with the decline in preterm births shown in Figure 42-2.
Importantly, the 2003 version of the birth certificate introduced use of a clinical estimate of gestational age rather than primarily the last menstrual period, which was used in the previous 1989 version of the birth certificate. Joseph and associates (2007) noticed that preterm birth rates were much higher in the United States compared with Canada. This difference, however, was reduced when the United States rate was based on the clinical estimate of gestational age rather than menstrual dating. For example, the preterm birth rate in the United States in 2002 was 12.3 percent if computed using menstrual dating compared with 10.1 percent when a clinical estimate was used. The decrease in preterm births shown in Figure 42-2 from 12.8 percent in 2006 to 11.7 percent in 2011 is well within the range of change to be expected if the change was attributable to the method used for determining gestational age for the 2003 birth certificate.
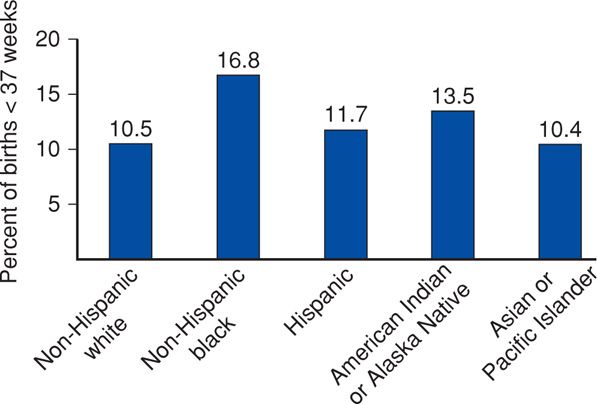
A disturbing aspect of the trend in preterm birth rates in the United States is the persistence of racial and ethnic disparity (Fig. 42-3). Indeed, 77 percent of the race/ethnicity-related disparity in infant mortality rates in the United States in 2009 was associated with preterm birth (Mathews, 2013). Some investigators attribute this disparity to socioeconomic circumstances (Collins, 2007). Rates of preterm birth in the United States are also higher compared with those in other industrialized countries (Ananth, 2009; Joseph, 2007). For example, the preterm birth rate was 12.3 percent in the United States in 2003 compared with 7.7 percent in Canada. Indeed, similar differences have been noted in the preterm delivery rates between the United States and virtually all the other industrialized countries.
FIGURE 42-3 Preterm births in the United States in 2011 according to maternal race and ethnicity. (Redrawn from Hamilton, 2012.)
MORBIDITY IN PRETERM INFANTS
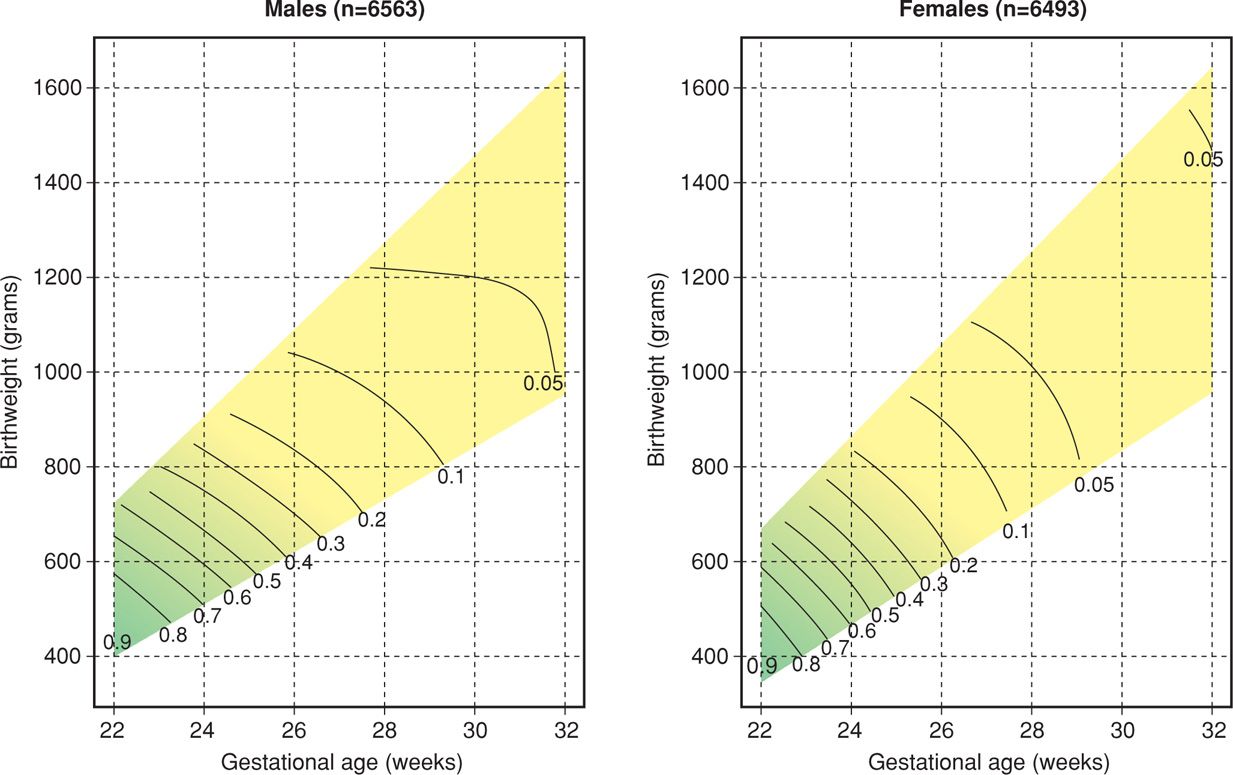
Various morbidities, largely due to organ system immaturity, are significantly increased in infants born before 37 weeks’ gestation compared with those delivered at term (Table 42-2). For approximately 40 years, complications in infants born before 34 weeks have been the primary focus. Only recently (2005) have late preterm infants—34 to 36 weeks—gained attention because of their increased morbidity. Attention has also been given to increasingly small preterm infants—very low birthweight and extremely low birthweight. These very small infants suffer disproportionately not only the immediate complications of prematurity but also long-term sequelae such as neurodevelopmental disability. Indeed, live births once considered “abortuses” because they weighed < 500 g are now classified as live births. Indeed, there were 6331 live births between 400 and 500 g recorded in the United States in 2009 (Martin, 2011). Remarkable strides have been made in neonatal survival for infants born preterm. This is especially true for those born after 28 weeks. Shown in Figure 42-4 are survival rates for more than 18,000 infants born between 400 and 1500 g or between 22 and 32 weeks’ gestation. Importantly, the results are shown as a function of both birthweight and gestational age. After achieving a birthweight of ≥ 1000 g or a gestational age of 28 weeks for females or 30 weeks for males, survival rates reach 95 percent.
TABLE 42-2. Major Short- and Long-Term Problems in Very-Low-Birthweight Infants
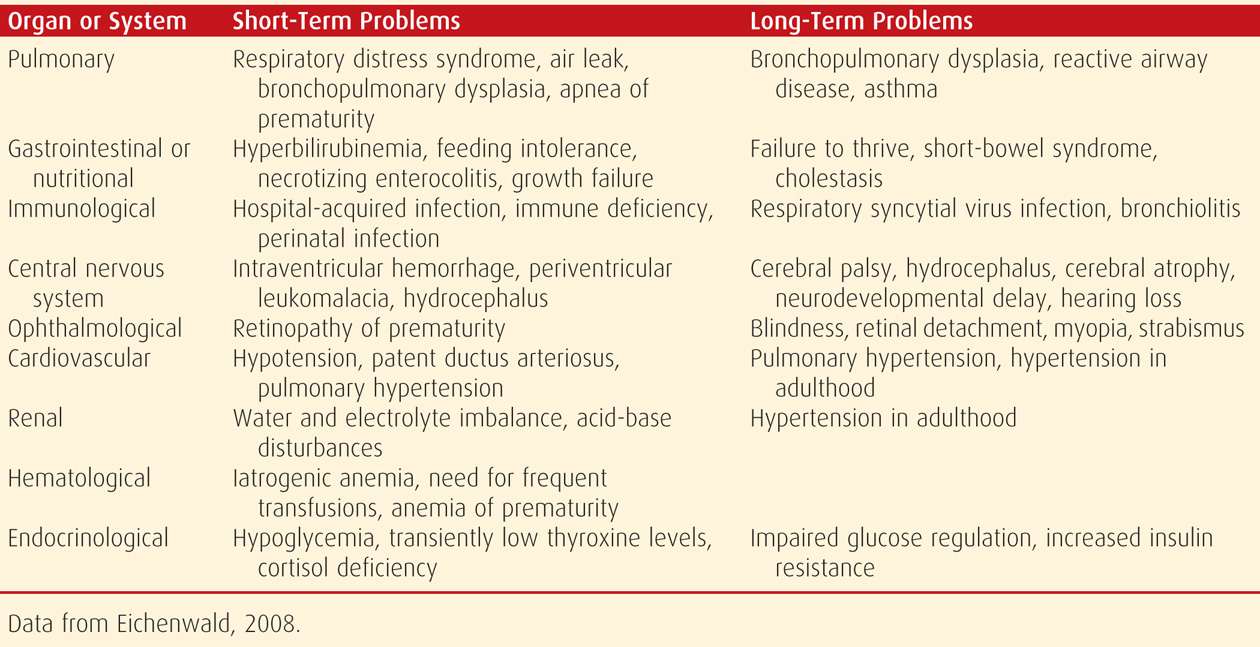
FIGURE 42-4 Mortality rates by birthweight, gestational age, and gender. The limits of the colored area indicate the upper 95th and lower 5th percentiles of birthweight for each gestational age. The curved lines indicate combinations of birthweight and gestational age with the same estimated probability of mortality from 10 to 90 percent. The gradation of color denotes the change in estimated probability of death. Green indicates infants of lower gestational age and birthweight who are more likely to die, whereas yellow indicates infants of higher gestational age and birthweight who are less likely to die. The methods used underestimate mortality rates in those at 22 and 23 weeks with a birthweight up to 600 g. (Redrawn from Fanaroff, 2007, with permission.)
Resources used to care for low-birthweight infants are a measure of the societal burden of preterm birth. The annual cost of preterm birth in the United States in 2006 was estimated to be $26.2 billion, or $51,000 per premature infant (Institute of Medicine, 2007). The economic consequences of preterm birth that reach beyond the newborn period into infancy, adolescence, and adulthood are difficult to estimate. However, they must be enormous when the effects of adult diseases associated with prematurity, such as hypertension and diabetes, are considered.
 Mortality and Morbidity at the Extremes of Prematurity
Mortality and Morbidity at the Extremes of Prematurity
The tremendous advances in the perinatal and neonatal care of the preterm infant have been found predominantly in those infants delivered at ≤ 33 weeks. With survival of increasingly very immature infants in the 1990s, there has been uncertainty and controversy as to the lower limit of fetal maturation compatible with extrauterine survival. This has resulted in continual reassessment of the threshold of viability.
Threshold of Viability
Births before 26 weeks are generally considered at the current threshold of viability, and these preterm infants pose various complex medical, social, and ethical considerations. For example, Sidney Miller is a child who was born at 23 weeks, weighed 615 g, and survived but developed severe physical and mental impairment (Annas, 2004). At age 7 years, she was described as a child who “could not walk, talk, feed herself, or sit up on her own … was legally blind, suffered from severe mental retardation, cerebral palsy, seizures, and spastic quadriparesis in her limbs.” An important issue for her family was the need for a lifetime of medical care estimated to cost tens of millions of dollars.
Infants now considered to be at the threshold of viability are those born at 22, 23, 24, or 25 weeks (American College of Obstetricians and Gynecologists, 2012a,b). These infants have been described as fragile and vulnerable because of their immature organ systems. Moreover, they are at high risk for brain injury from hypoxic-ischemic injury and sepsis. In this setting, hypoxia and sepsis start a cascade of events that lead to brain hemorrhage, white-matter injury that causes periventricular leukomalacia, and poor subsequent brain growth eventuating in neurodevelopmental impairment (Chap. 34, p. 656). Because active brain development normally occurs throughout the second and third trimesters, those infants born at 22 to 25 weeks are believed especially vulnerable to brain injury.
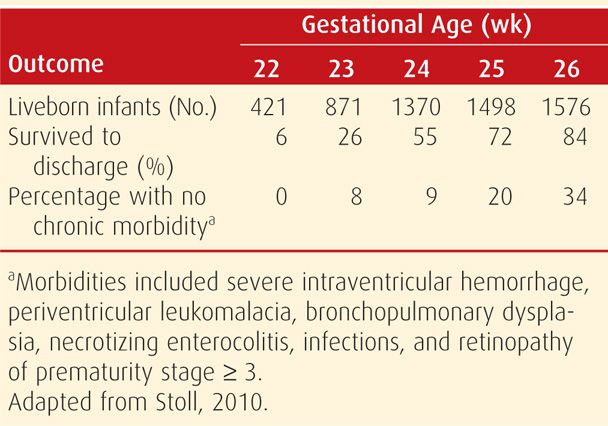
Until recently, discussion of clinical management and ethical and economic considerations of extremely premature infants were hampered by data compromised by ascertainment bias (American College of Obstetricians and Gynecologists, 2012a,b). For example, the mean survival rate was 45 percent if the denominator was all live births compared with 72 percent if the denominator used was only infants admitted to neonatal intensive care (Guillen, 2011). Another source of ascertainment bias was use of multicenter datasets. There were considerable center differences in obstetrical and early neonatal interventions, particularly at 22 and 23 weeks (Stoll, 2010).
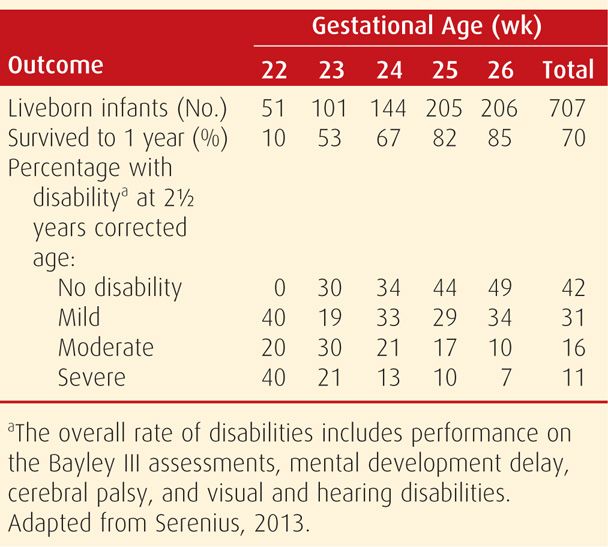
A remarkable report on infants born before 27 weeks was recently published (Serenius, 2013). This report is unique in that it details a national population-based prospective study of all infants born alive or stillborn before 27 weeks in Sweden. This country is a uniform society without extreme poverty, and antenatal care is easily accessible and used by almost 100 percent of mothers. All citizens are covered by health insurance including 480 days of parental leave after childbirth and additional benefits for severely sick children. Active perinatal care in Sweden includes early and free access to specialist perinatal care, centralization of extremely preterm births to level III hospitals, a low threshold to provide life support at birth, and near universal admission of infants born at 23 to 26 weeks for neonatal intensive care. Thus, this report likely describes infant outcomes at the threshold of viability under optimal circumstances.
Shown in Table 42-3 are the survival and disability rates for 707 infants born alive from 22 to 26 weeks between 2004 and 2007 in Sweden. The proportion of children with mild or no disabilities increased from 40 percent at 22 weeks to 83 percent at 26 weeks. Conversely, the number of infants with moderate or severe disabilities decreased with advancing gestational age at birth. Moderate or severe disabilities were found in 31 percent of preterm boys compared with 23 percent of preterm girls. No differences in overall outcomes were noted if singletons and multiple births were compared.
TABLE 42-3. Outcomes at 2½ Years Corrected Age by Gestational Age at Birth in Sweden, 2004–2007
The most recent report from the United States concerning survival and morbidity rates for births at 22 to 26 weeks is from the National Institute of Child Health and Human Development (NICHD) Neonatal Network. This dataset includes 5736 live births delivered between 2003 and 2007 at 20 medical centers across the United States. Rates of survival and survival without morbidity in the neonatal period are shown in Table 42-4.
TABLE 42-4. Survival and Disability Rates for 5736 Live Births Born between 22 and 26 Weeks’ Gestation at 20 Medical Centers in the United States During 2003–2007
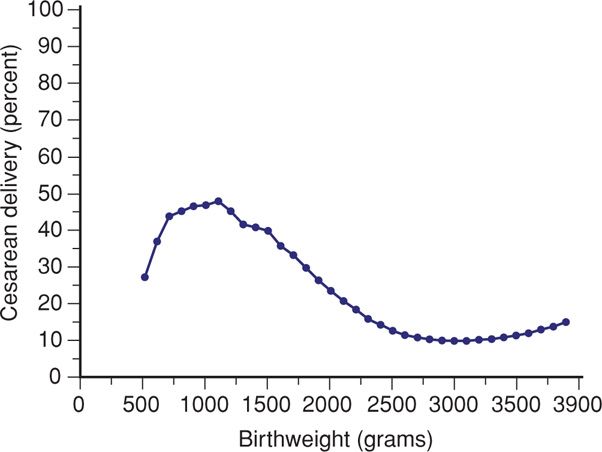
Cesarean delivery at the threshold of viability is controversial. For example, if the fetus-infant is perceived to be too immature for aggressive support, then cesarean delivery for common indications such as breech presentation or nonreassuring fetal heart rate patterns might be preempted. This aside, national data clearly show a high frequency of cesarean delivery for these small infants (Fig. 42-5). Determining the optimal delivery mode for newborns at the threshold of viability is virtually impossible given that randomizing the delivery route has extreme ethical considerations. That said, retrospective, nonrandomized studies have consistently failed to document a benefit of cesarean delivery for the extremely preterm fetus (American College of Obstetricians and Gynecologists, 2012a). Reddy (2012) analyzed 2906 singleton live births between 240/7 and 316/7 weeks selected because they were eligible for attempted vaginal birth after excluding those cases with fetal distress, placenta previa, placental abruption, and anomalies. Attempted vaginal delivery for cephalic presenting fetuses had a high success rate (84 percent), and there was no difference in the neonatal mortality rate compared with that with planned cesarean delivery. For breech presentations, however, there was a threefold increased relative risk in mortality when vaginal delivery was attempted. Werner (2013) analyzed 20,231 preterm infants at 24 to 34 weeks born in New York City between 1995 and 2003. Cesarean delivery was not protective against poor outcomes such as neonatal death, intraventricular hemorrhage, seizures, respiratory distress, and subdural hemorrhage.
FIGURE 42-5 United States cesarean delivery rates by birthweight from 1999 to 2000. (Redrawn from Lee, 2006, with permission.)
Threshold of Viability at Parkland Hospital
Policies were developed in conjunction with the Neonatology Service. We must emphasize that the decision not to perform cesarean delivery does not necessarily imply that the fetus is “nonviable” or “written off.” Neonatologists are consulted before delivery, and there is discussion of survival and morbidity with the woman and her family. A neonatologist attends each delivery and determines subsequent management.
From an obstetrical standpoint, all fetal indications for cesarean delivery in more advanced pregnancies are practiced in women at 25 weeks. Cesarean delivery is not offered for fetal indications at 23 weeks. At 24 weeks, cesarean delivery is not offered unless fetal weight is estimated at 750 g or greater. Aggressive obstetrical management is practiced in cases of growth restriction.
 Late Preterm Birth
Late Preterm Birth
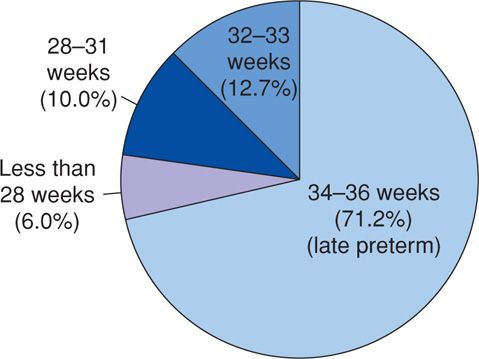
As shown in Figure 42-6, infants between 34 and 36 weeks account for more than 70 percent of all preterm births. These are the fastest increasing and largest proportion of singleton preterm births in the United States (Raju, 2006). Thus, increased attention is being given to determining optimal obstetrical and neonatal management of late preterm birth.
FIGURE 42-6 Distribution in percent of preterm births in the United States for 2004. (Redrawn from Martin, 2006.)
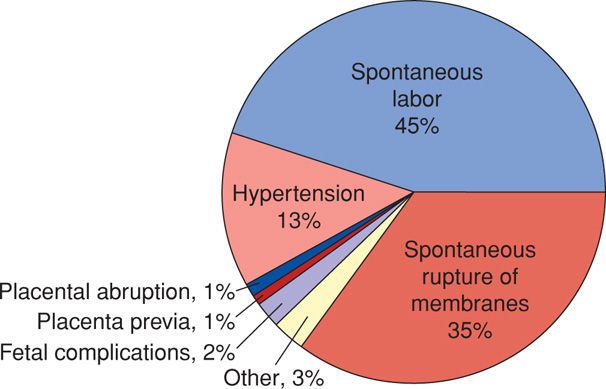
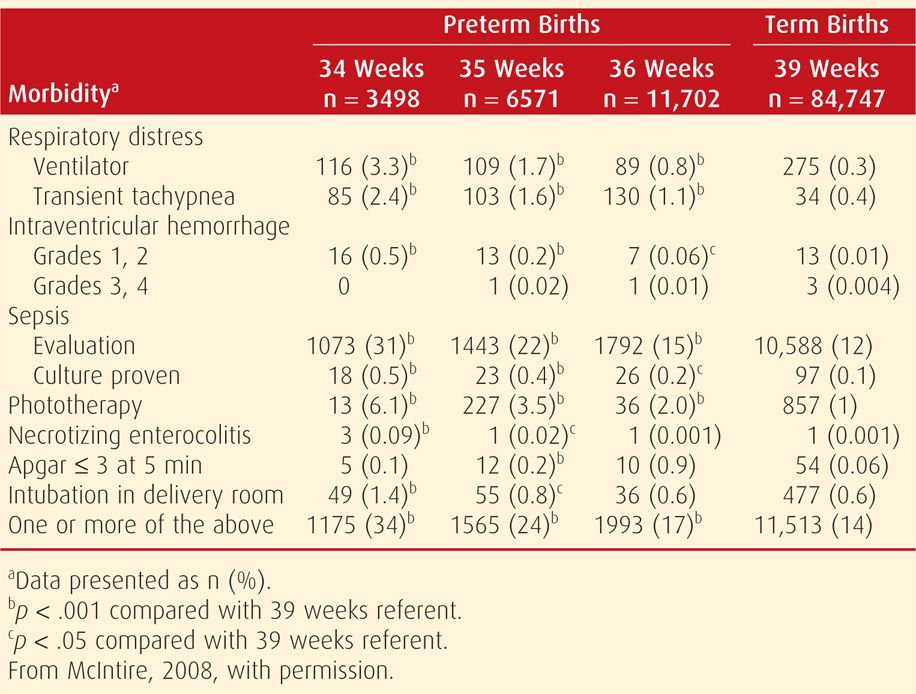
To estimate the risks associated with late preterm births, we analyzed neonatal mortality and morbidity rates at 34, 35, and 36 weeks compared with those of births at term between 1988 and 2005 at Parkland Hospital (McIntire, 2008). We were particularly interested in obstetrical complications during this time, because if modified, rates of late preterm birth can possibly be decreased. Approximately 3 percent of all births during the study period occurred between 24 and 32 weeks, and 9 percent were during the late preterm weeks. Thus, late preterm births accounted for three fourths of all preterm births. Approximately 80 percent of these were due to idiopathic spontaneous preterm labor or prematurely ruptured membranes (Fig. 42-7). Complications such as hypertension or placental accidents were implicated in the other 20 percent of cases.
FIGURE 42-7 Obstetrical complications associated with 21,771 late preterm births at Parkland Hospital. (Adapted from McIntire, 2008.)
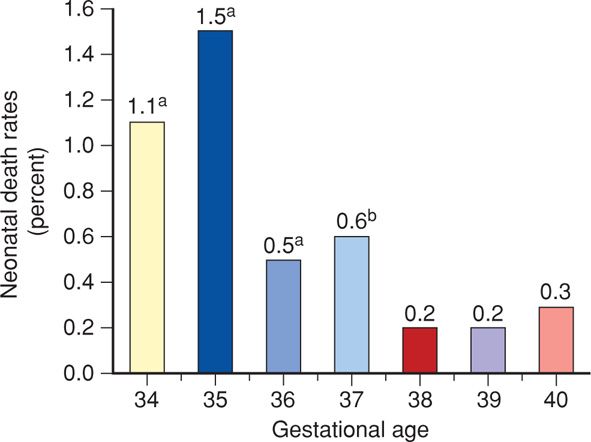
Neonatal mortality rates were significantly increased in each late preterm week compared with those at 39 weeks as the referent and as shown in Figure 42-8. Similarly, Tomashek (2007) analyzed all United States births between 1995 and 2002 and also found higher neonatal mortality rates for late preterm infants. Importantly, indices of neonatal morbidity shown in Table 42-5 are increased in these late preterm infants born at Parkland. Fuchs (2008) reported similar results regarding respiratory morbidity in 722 infants. Specifically, the frequency of respiratory morbidity decreased by approximately 50 percent per week from 34 to 37 completed weeks. Increased rates of adverse neurodevelopment have also been found in late preterm infants compared with term newborns (Petrini, 2009).
FIGURE 42-8 Neonatal death rates at Parkland Hospital from 34 to 40 weeks’ gestation in singleton infants without malformations. ap < .001 compared with 39 weeks as the referent. bp = .02 compared with 39 weeks as the referent. (Redrawn from McIntire, 2008, with permission.)
TABLE 42-5. Neonatal Morbidity Rates at Parkland Hospital in Live Births Delivered Late Preterm Compared with 39 Weeks
These findings suggest that the health-care focus on prematurity should be expanded to include late preterm births. Even so, because approximately 80 percent of these women begin labor spontaneously—similar to births before 34 weeks—attempts to interrupt preterm labor have not been satisfactory. Specifically, the Institute of Medicine (2007) report, Preterm Birth: Causes, Consequences, and Prevention, acknowledges that treatment of preterm labor has not prevented preterm birth. Thus, we are of the view that a national strategy aimed at prevention of late preterm births is unlikely to provide discernible benefit without new developments in the prevention and management of preterm labor. In the meantime, the Maternal-Fetal Medicine Units (MFMU) Network is studying the efficacy of corticosteroids in late preterm births. The American College of Obstetricians and Gynecologists (2013b) has emphasized that intentional late preterm deliveries should occur only when an accepted maternal or fetal indication for delivery exists.
CAUSES OF PRETERM DELIVERY
There are four main direct reasons for preterm births in the United States. These include: (1) spontaneous unexplained preterm labor with intact membranes, (2) idiopathic preterm premature rupture of membranes (PPROM), (3) delivery for maternal or fetal indications, and (4) twins and higher-order multifetal births. Of all preterm births, 30 to 35 percent are indicated, 40 to 45 percent are due to spontaneous preterm labor, and 30 to 35 percent follow preterm membrane rupture (Goldenberg, 2008). Indeed, much of the increase in the singleton preterm birth rate in the United States is explained by rising numbers of indicated preterm births (Ananth, 2005).
Reasons for preterm birth have multiple, often interacting, antecedents and contributing factors. This complexity has greatly confounded efforts to prevent and manage this complication. This is particularly true for preterm ruptured membranes and spontaneous preterm labor, which together lead to 70 to 80 percent of preterm births. Last, according to data from Martin (2006), approximately one in six preterm births in the United States is from twins or higher-order multifetal pregnancies (Chap. 45, p. 891). For example, in 2004, there were 508,356 preterm births, and of these, 86,116 or 17 percent were from multifetal pregnancies. Many of these pregnancies were achieved using ovulation-inducing drugs and assisted reproductive technologies (ART).
Analogous to other complex disease processes, multiple coexistent genetic alterations and environment may lead to preterm birth (Esplin, 2005; Ward, 2008). There are polymorphisms in genes associated with inflammation and infection and in those associated with collagen turnover (Velez, 2008). Inherited mutations in genes regulating collagen assembly may predispose individuals to cervical insufficiency or prematurely ruptured membranes (Anum, 2009; Wang, 2006; Warren, 2007).
 Basic Science of Spontaneous Preterm Labor
Basic Science of Spontaneous Preterm Labor
For both clinical and research purposes, pregnancies with intact fetal membranes and spontaneous preterm labor must be distinguished from those complicated by preterm prematurely ruptured membranes. Even so, those with spontaneous preterm labor do not constitute a homogeneous group characterized singularly by early initiation of parturition (American College of Obstetricians and Gynecologists, 2012b). This certainly is one reason why preventative therapies and clinical tools to assess the risks for preterm birth have been difficult to identify. Among the more common associated findings are multifetal pregnancy, intrauterine infection, bleeding, placental infarction, premature cervical dilatation, cervical insufficiency, hydramnios, uterine fundal abnormalities, and fetal anomalies. Severe maternal illness as a result of infections, autoimmune diseases, and gestational hypertension also increases preterm labor risks.
Although there are unique aspects to each cause of preterm labor, these diverse processes culminate in a common end point, which is premature cervical dilatation and effacement and premature activation of uterine contractions. It seems important to emphasize that the actual process of preterm labor should be considered a final step—one that results from progressive or acute changes that could be initiated days or even weeks before labor onset. Indeed, many forms of spontaneous preterm labor that result from premature initiation of phase 2 of parturition may be viewed in this light (Chap. 21, p. 410). Although the end result in preterm birth is the same as at term, namely cervical ripening and myometrial activation, recent studies in animal models support the idea that preterm birth is not always an acceleration of the normal process. Diverse pathways to instigate parturition exist and are dependent on the etiology of preterm birth. Identification of both common and uncommon factors has begun to explain the physiological processes of human parturition at term and preterm. Four major causes of spontaneous preterm labor include uterine distention, maternal–fetal stress, premature cervical changes, and infection.
Uterine Distention
There is no doubt that multifetal pregnancy and hydramnios lead to an increased risk of preterm birth (Chap. 45, p. 913). It is likely that early uterine distention acts to initiate expression of contraction-associated proteins (CAPs) in the myometrium. The CAP genes that are influenced by stretch include those coding for gap-junction proteins such as connexin 43, for oxytocin receptors, and for prostaglandin synthase (Korita, 2002; Lyall, 2002; Sooranna, 2004). Recent reports suggest that gastrin-releasing peptides (GRPs) are increased with stretch to promote myometrial contractility and that GRP antagonists can inhibit uterine contractility (Tattershell, 2012). There is also a stretch-induced potassium channel—TREK-1—that is upregulated during gestation and downregulated in labor. This pattern of expression is consistent with a potential role in uterine relaxation during pregnancy (Buxton, 2010). Expression of TREK-1 splice variants that block function of the full-length TREK-1 have been recently identified in myometrium from women with preterm labor. This further implicates a role for TREK-1 in uterine quiescence (Wu, 2012). Although these and other regulatory factors remain to be validated, it is clear that excessive uterine stretch causes premature loss of myometrial quiescence.
Excessive uterine stretch also leads to early activation of the placental–fetal endocrine cascade shown in Figure 21-17 (p. 425). The resulting early rise in maternal corticotropin-releasing hormone and estrogen levels can further enhance the expression of myometrial CAP genes (Warren, 1990; Wolfe, 1988). Finally, the influence of uterine stretch should be considered with regard to the cervix. For example, cervical length is an important risk factor for preterm birth in multifetal pregnancies (Goldenberg, 1996). Prematurely increased stretch and endocrine activity may initiate events that shift the timing of uterine activation, including premature cervical ripening.
Maternal–Fetal Stress
Stress is defined as a condition or adverse circumstance that disturbs the normal physiological or psychological functioning of an individual. But the complexities of measuring “stress” are what cause difficulty in defining its exact role (Lobel, 1994). That said, considerable evidence shows a correlation between some sort of maternal stress and preterm birth (Hedegaard, 1993; Hobel, 2003; Ruiz, 2003). Moreover, there is a correlation between maternal psychological stress and the placental–adrenal endocrine axis that provides a potential mechanism for stress-induced preterm birth (Lockwood, 1999; Petraglia, 2010; Wadhwa, 2001).
As discussed earlier, the last trimester is marked by rising maternal serum levels of placental-derived corticotropin-releasing hormone (CRH). This hormone works with adrenocorticotropic hormone (ACTH) to increase adult and fetal adrenal steroid hormone production, including the initiation of fetal cortisol biosynthesis. Rising levels of maternal and fetal cortisol further increase placental CRH secretion, which develops a feed-forward endocrine cascade that does not end until delivery (Fig. 21-17, p. 425). Rising levels of CRH further stimulate fetal adrenal dehydroepiandrosterone sulfate (DHEA-S) biosynthesis, which acts as substrate to increase maternal plasma estrogens, particularly estriol.
It has been hypothesized that a premature rise in cortisol and estrogens results in an early loss of uterine quiescence. A number of studies have reported that spontaneous preterm labor is associated with an early rise in maternal CRH levels and that CRH determination may be a useful biomarker for preterm birth risk assessment (Holzman, 2001; McGrath, 2002; McLean, 1995; Moawad, 2002). Because of large variations in CRH levels among pregnant women, however, a single CRH measurement has low sensitivity (Leung, 2001; McGrath, 2002). It may be that the rate of increase in maternal CRH levels is possibly a more accurate predictor of preterm birth. Confounding factors include CRH variability among ethnic groups. Another is that placental CRH enters the fetal circulation—albeit at lower levels than in the maternal circulation. In vitro studies have shown that CRH can directly stimulate fetal adrenal production of DHEA-S and cortisol (Parker, 1999; Smith, 1998). Thus, current studies do not support the idea that CRH levels alone have a positive-predictive value for preterm birth risk.
If preterm delivery is associated with early activation of the fetal adrenal–placental endocrine cascade, maternal estrogen levels would likely be prematurely elevated. This is indeed the case. An early rise in serum estriol concentrations is noted in women with subsequent preterm labor (Heine, 2000; McGregor, 1995). Physiologically, this premature rise in estrogen levels may alter myometrial quiescence and accelerate cervical ripening.
Taken together, these observations suggest that preterm birth is associated, in many cases, with a maternal–fetal biological stress response. The stressors that activate this cascade likely are broad, and the stress response is dependent on the stressor. For example, CRH or estriol levels are prematurely elevated in preterm birth due to infection and multifetal pregnancies but not in pregnant women with perceived stress (Gravett, 2000; Himes, 2011; Warren, 1990). Chronic, psychological stress—resulting for example from racial discrimination—appears to promote impaired cellular immune competence (Christian, 2012b). A growing body of work in the area of psychoneuroimmunology will perhaps enhance the understanding of pathways that link stress with adverse birth outcomes (Christian, 2012a).
Infection
There is great interest in the role of infection as a primary cause of preterm labor in pregnancies with intact membranes (Goncalves, 2002; Iams, 1987). In some cases, there is histological evidence of inflammation in the fetal membranes, decidua, or umbilical cord, whereas other cases are deemed “subclinical.” More recently, new technologies based on genomic analysis of a mixed population of microorganisms have shown that the nonpregnant vaginal tract hosts a complex microbial community that can differ widely between women who are all healthy (Gajer, 2012; White, 2011). The application of the field of metagenomics to understanding microbiome complexity in term and preterm birth and to identifying microbe populations that may mediate subclinical infection holds great promise. Aagaard and coworkers (2012) used metagenomics to determine how the vaginal microbiome changes during normal pregnancy. They reported that the diversity and richness of microbes is reduced through pregnancy. Compared with nonpregnant controls, there is an increased dominance of Lactobacillus species. These findings lay the foundation for future studies to identify microbial populations associated with “subclinical” infection-induced preterm birth.
Current data suggest that microbial invasion of the reproductive tract is sufficient to induce infection-mediated preterm birth—more specifically, there is ongoing “subclinical” infection. However, microorganisms certainly are not ubiquitous in the amnionic fluid of all women with preterm labor, and indeed, positive cultures are found in only 10 to 40 percent (Goncalves, 2002). This minority of women with amnionic fluid bacteria are more likely to develop clinical chorioamnionitis and preterm ruptured membranes compared with women with sterile cultures. Moreover, their neonates are also more likely to have complications (Hitti, 2001). Although infection is more severe when there is clinically obvious intraamnionic infection, inflammation in the absence of detectable microorganisms is also a risk factor for a fetal inflammatory response (Lee, 2007, 2008). The earlier the onset of preterm labor, the greater the likelihood of documented infection (Goldenberg, 2000; Watts, 1992). It is enigmatic that the incidence of culture-positive amnionic fluids collected by amniocentesis during spontaneous term labor is similar to that with preterm labor (Gomez, 1994; Romero, 1993). It has been suggested that at term, amnionic fluid is infiltrated by bacteria as a consequence of labor, whereas in preterm pregnancies, bacteria represent an important cause of labor. If true, this explanation questions the contribution of fetal infection as a major cause of preterm labor and delivery.
Despite these observations, there are considerable data that associate chorioamnionitis with preterm labor (Goldenberg, 2002; Üstün, 2001). In such infections, the microbes may invade maternal tissue only and not amnionic fluid. Despite this, endotoxins can stimulate amnionic cells to secrete cytokines that enter amnionic fluid. This scenario may serve to explain the apparently contradictory observations concerning an association between amnionic fluid cytokines and preterm labor, in which microbes were not detectable in the amnionic fluid.
Sources for Intrauterine Infection. The patency of the female reproductive tract, although essential for achievement of pregnancy and delivery, is theoretically problematic during phase 1 of parturition. It has been suggested that bacteria can gain access to intrauterine tissues through: (1) transplacental transfer of maternal systemic infection, (2) retrograde flow of infection into the peritoneal cavity via the fallopian tubes, or (3) ascending infection with bacteria from the vagina and cervix. The lower pole of the fetal membrane–decidual junction is contiguous with the cervical canal orifice, which is patent to the vagina. This anatomical arrangement provides a passageway for microorganisms, and ascending infection is considered to be the most common. A thoughtful description of the potential degrees of intrauterine infection has been provided by Goncalves and associates (2002). They categorize intrauterine infection into four stages of microbial invasion that include bacterial vaginosis—stage I, decidual infection—stage II, amnionic infection—stage III, and finally, fetal systemic infection—stage IV. As expected, progression of these stages is thought to increase rates of preterm birth and neonatal morbidity.
Based on these insights, it is straightforward to construct a theory for the pathogenesis of infection-induced preterm labor. Ascending microorganisms colonize the cervix, decidua, and possibly the membranes, where they then may enter the amnionic sac. Lipopolysaccharide (LPS) or other toxins elaborated by bacteria induce immune-cell recruitment into the reproductive tract and cytokine production by immune cells and by cells within the cervix, decidua, membranes, or fetus itself. Both LPS and cytokines then provoke prostaglandin release from the membranes, decidua, or cervix. These influence both cervical ripening and loss of myometrial quiescence (Challis, 2002; Keelan, 2003; Olson, 2003). Current evidence based on animal and human studies suggests that many aspects of infection-mediated preterm birth differ from pathways that regulate term parturition (Hamilton, 2012; Holt, 2011; Shynlova, 2013a,b).
Microbes Associated with Preterm Birth. Some micro-organisms—examples include Gardnerella vaginalis, Fusobacterium, Mycoplasma hominis, and Ureaplasma urealyticum—are detected more frequently than others in amnionic fluid of women with preterm labor (Gerber, 2003; Hillier, 1988; Yoon, 1998). This finding was interpreted by some as presumptive evidence that specific microorganisms are more commonly involved as pathogens in the induction of preterm labor. Another interpretation, however, is that given direct access to the membranes after cervical dilatation, selected microorganisms, such as fusobacteria, that are more capable of burrowing through these exposed tissues will do so. Fusobacteria are found in the vaginal fluid of only 9 percent of women but in 28 percent of positive amnionic fluid cultures from pregnancies with preterm labor and intact membranes (Chaim, 1992). Knowledge from metagenomic studies will better define these interactions in the future. In addition, host responses to pathogens with respect to mucosal immunity, barrier protection of cervical and vaginal epithelia, and expression of antimicrobial peptides is likely to provide insights. Specifically, the mechanisms that render some women more susceptible to infection-mediated preterm birth may be found.
Intrauterine Inflammatory Response. The initial inflammatory response elicited by bacterial toxins is mediated, in large measure, by specific receptors on mononuclear phagocytes, decidual cells, cervical epithelia, and trophoblasts. These Toll-like receptors represent a family that has evolved to recognize pathogen-associated molecules (Janssens, 2003). Toll-like receptors are present in the placenta on trophoblast cells, in the cervical epithelia, and on fixed and invading leukocytes (Chuang, 2000; Gonzalez, 2007; Holmlund, 2002). Loss of specific Toll-like receptors results in delayed parturition in mouse models (Montalbano, 2013).
Under the influence of ligands such as bacterial LPS, these receptors increase chemokine, cytokine, and prostaglandin release as part of an inflammatory response. One example is interleukin-1β (IL-1β), which is produced rapidly after LPS stimulation (Dinarello, 2002). This cytokine in turn acts to promote a series of responses that include: (1) increased synthesis of others, that is, IL-6, IL-8, and tumor-necrosis factor alpha (TNF-α); (2) proliferation, activation, and migration of leukocytes; (3) modifications in extracellular matrix proteins; and (4) mitogenic and cytotoxic effects such as fever and acute-phase response (El-Bastawissi, 2000). Also, IL-1 promotes prostaglandin formation in many tissues, including myometrium, decidua, and amnion (Casey, 1990). The importance of prostaglandins to infection-mediated preterm birth is supported by the observation that prostaglandin inhibitors can reduce the rate of LPS-induced preterm birth in both the mouse and nonhuman primate (Gravett, 2007; Gross, 2000). Inhibition of cyclooxygenase-2 prevents inflammation-mediated preterm labor in the mouse. And immunomodulators plus antibiotics delay preterm delivery after experimental intraamnionic infection in a nonhuman primate model. Thus, there appears to be a cascade of events once an inflammatory response is initiated that can result in preterm labor.
Origin of Cytokines. Cytokines within the normal term uterus are likely important for normal and preterm labor. The transfer of cytokines such as IL-1 from decidua across the membranes into amnionic fluid appears to be severely limited. It is reasonable that cytokines produced in maternal decidua and myometrium will have effects on that side, whereas cytokines produced in the membranes or in cells within the amnionic fluid will not be transferred to maternal tissues. The human myometrium expresses chemokine receptors that decline during labor (Hua, 2013). Macrophages are reported to infiltrate the human and rat decidua before labor onset and may be important for decidual activation (Hamilton, 2012). Still, the requirement of leukocytes for initiation of term labor in women remains inconclusive. In most cases of inflammation resulting from infection, resident and invading leukocytes produce the bulk of cytokines. Indeed, with infection, leukocytes—mainly neutrophils, macrophages, and T lymphocytes—infiltrate the cervix, lower uterine segment, fundus, and membranes at the time of labor. Thus, invading leukocytes may be the major source of cytokines in preterm labor. Along with proinflammatory cytokines, studies in women and animal models highlight the importance of the antiinflammatory limb of the immune response in parturition (Gotsch, 2008; Timmons, 2009).
Immunohistochemical studies in the term laboring uterus have shown that both invading leukocytes and certain parenchymal cells produce cytokines. These leukocytes appear to be the primary source of myometrial cytokines, including IL-1, IL-6, IL-8, and TNF-α (Young, 2002). By contrast, in the decidua, both stromal cells and leukocytes are likely to contribute because they have been shown to produce these same cytokines. In the cervix, glandular and surface epithelial cells appear to produce IL-6, IL-8, and TNF-α. Of these, IL-8 is considered a critical cytokine in cervical dilation, and it is produced in both cervical epithelial and stromal cells.
The presence of cytokines in amnionic fluid and their association with preterm labor has been well documented. But their exact cellular origin—with or without recoverable microorganisms—has not been well defined. Although the rate of IL-1 secretion from forebag decidual tissue is great, Kent (1994) found that there is negligible in vivo transfer of radiolabeled IL-1 across the membranes. Amnionic fluid IL-1 probably does not arise from amnion, fetal urine, or fetal lung secretions. It most likely is secreted by mononuclear phagocytes or neutrophils activated and recruited into the amnionic fluid. Therefore, IL-1 in amnionic fluid likely is generated in situ from newly recruited cells (Young, 2002). Thus, the amount of amnionic fluid IL-1 would be determined by the number of leukocytes recruited, their activational status, or the effect of amnionic fluid constituents on their IL-1 secretion rate.
Leukocyte infiltration may be regulated by fetal membrane synthesis of specific chemokines. In term labor, there are increased amnionic fluid concentrations of the potent chemoattractant and monocyte-macrophage activator monocyte chemotactic protein-1 (MCP-1), which is also called chemokine (C-C motif) ligand 2 (CCL2). As is true for prostaglandins and other cytokines, the levels of MCP-1 are much higher in the forebag compared with the upper compartment (Esplin, 2003). Levels in preterm labor were significantly higher than those found in normal term amnionic fluid (Jacobsson, 2003). MCP-1 may initiate fetal leukocyte infiltration of the placenta and membranes, and its production may act as a marker for intraamnionic infection and inflammation.
 Preterm Premature Rupture of Membranes
Preterm Premature Rupture of Membranes
This term defines spontaneous rupture of the fetal membranes before 37 completed weeks and before labor onset (American College of Obstetricians and Gynecologists, 2013d). Such rupture likely has various causes, but intrauterine infection is believed by many to be a major predisposing event (Gomez, 1997; Mercer, 2003). There are associated risk factors that include low socioeconomic status, body mass index ≤ 19.8, nutritional deficiencies, and cigarette smoking. Women with prior preterm premature rupture of membranes (PPROM) are at increased risk for recurrence during a subsequent pregnancy (Bloom, 2001). Despite these known risk factors, none is identified in most cases of preterm rupture.
Molecular Changes
Preterm membrane rupture pathogenesis may be related to increased apoptosis of membrane cellular components and to increased levels of specific proteases in membranes and amnionic fluid. Most tensile strength of the membranes is provided by the amnionic extracellular matrix and interstitial amnionic collagens—primarily type I and III—which are produced in mesenchymal cells (Casey, 1996). For that reason, collagen degradation has been a focus of research. The matrix metalloproteinase (MMP) family is involved with normal tissue remodeling and particularly with collagen degradation. The MMP-1, MMP-2, MMP-3, and MMP-9 members of this family are found in higher concentrations in amnionic fluid from pregnancies with preterm prematurely ruptured membranes (Maymon, 2000; Park, 2003; Romero, 2002). MMP activity is in part regulated by tissue inhibitors of matrix metalloproteinases—TIMPs. Several of these inhibitors are found in lower concentrations in amnionic fluid from women with ruptured membranes. Elevated MMP levels found at a time when protease inhibitor expression decreases supports further that their expression alters amnionic tensile strength. Studies of amniochorion explants have demonstrated that the expression of MMPs can be increased by treatment with IL-1, TNF-α, and IL-6 (Fortunato, 1999a,b, 2002). Recent studies by Mogami (2013) provide a mechanism by which bacterial endotoxin or TNF-α elicits release of fetal fibronectin (fFN) by amnion epithelial cells. The fFN then binds Toll-like receptor 4 in the amnion mesenchymal cells to activate signaling cascades. These result in increased prostaglandin E (PGE2) synthesis and elevated activity of MMP-1, MP-2, and MMP-9. Increased prostaglandin levels promote cervical ripening and uterine contractions. Increased MMPs allow collagen breakdown in the fetal membranes resulting in premature rupture.
In pregnancies with PPROM, the amnion exhibits a higher degree of cell death and more apoptosis markers than that in term amnion (Arechavaleta-Velasco, 2002; Fortunato, 2003). In vitro studies indicate that apoptosis is likely regulated by bacterial endotoxin, IL-1, and TNF-α. Last, there are proteins involved in the synthesis of mature cross-linked collagen or matrix proteins that bind collagen and thereby promote tensile strength. These proteins are altered in membranes with premature rupture (Wang, 2006). Taken together, these observations suggest that many PPROM cases result from collagen degradation, altered collagen assembly, and cell death, which all lead to a weakened amnion.
Infection
Several studies have been done to ascertain the incidence of infection-induced premature membrane rupture. Bacterial cultures of amnionic fluid support a role for infection in a significant proportion. A review of 18 studies comprising almost 1500 women with PPROM found that in a third, bacteria were isolated from amnionic fluid (Goncalves, 2002). Accordingly, some have given prophylactic antimicrobial treatment to prevent premature rupture (Miyazaki, 2012; Phupong, 2012).
Overall, there is compelling evidence that infection causes a significant proportion of PPROM cases. The inflammatory response that leads to membrane weakening is currently being defined. Research is focused on mediators of this process with a goal to identify early risk markers for PPROM.
 Multifetal Gestation
Multifetal Gestation
Twins and higher-order multifetal births account for approximately 3 percent of infants born in the United States (Martin, 2009a). The majority—95 percent—of these births are twins. Compared with 1980, the rates of multiple births increased steadily and peaked in 1998. Current rates have declined since then, but remain higher than the 1980s. The increased rate of multifetal births is due to the increased number of women having babies after the age of 30, at which time the risk to conceive multiples rises. In addition, the use of fertility treatments has contributed to the elevated rates of multifetal pregnancies. Preterm delivery continues to be the major cause of the excessive perinatal morbidity and mortality with multifetal pregnancies. The effects of uterine stretch discussed on page 837 are obvious in these pregnancies, and this likely is related to the increased incidence of preterm cervical dilatation. Many of these interrelationships are discussed in Chapter 45.
 Summary of Preterm Labor Pathophysiology
Summary of Preterm Labor Pathophysiology
Preterm labor is a pathological condition with multiple etiologies. Romero (2006) termed it the preterm parturition syndrome. Most research in this field has been focused on the role of infection in mediating preterm birth. It is possible that intrauterine infection causes some cases currently categorized as idiopathic spontaneous preterm labor. There are various sites for intrauterine infection—maternal, fetal, or both—and increasing evidence that the inflammatory response may have distinct and compartment-specific functions that differ between uterus, fetal membranes, and cervix in normal birth. Thus, determining the proportion of pregnancies that end prematurely because of infection is difficult.
Infection does not explain all causes of preterm birth. In recent years, our understanding of other influences on the parturition process, such as maternal nutrition before or during pregnancy, genetics, the vaginal microbiome, and dynamic regulation of the extracellular matrix, has led to new avenues of research and a broader understanding of this complicated and multifactorial process. The current and future application of genomic and bioinformatics as well as molecular and biochemical studies will shed light on pathways involved in term and preterm labor and identify processes critical to all phases of cervical remodeling and uterine function.
ANTECEDENTS AND CONTRIBUTING FACTORS
Myriad genetic and environmental factors affect the frequency of preterm labor.
 Threatened Abortion
Threatened Abortion
Vaginal bleeding in early pregnancy is associated with increased adverse outcomes later. Weiss (2004) reported outcomes with vaginal bleeding at 6 to 13 weeks in nearly 14,000 women. Both light and heavy bleeding were associated with subsequent preterm labor, placental abruption, and subsequent pregnancy loss before 24 weeks.
 Lifestyle Factors
Lifestyle Factors
Cigarette smoking, inadequate maternal weight gain, and illicit drug use have important roles in both the incidence and outcome of low-birthweight neonates (Chap. 12, p. 253). Overweight and obese mothers have an elevated risk of preterm birth (Cnattingius, 2013). Other maternal factors implicated include young or advanced maternal age, poverty, short stature, and vitamin C deficiency (Casanueva, 2005; Gielchinsky, 2002; Kramer, 1995; Meis, 1995; Satin, 1994).
As discussed on page 837, psychological factors such as depression, anxiety, and chronic stress have been reported in association with preterm birth (Copper, 1996; Li, 2008; Littleton, 2007). Neggers and coworkers (2004) found a significant link between low birthweight and preterm birth in women injured by physical abuse (Chap. 47, p. 951).
Studies of work and physical activity related to preterm birth have produced conflicting results (Goldenberg, 2008). There is some evidence, however, that working long hours and hard physical labor are probably associated with increased risk of preterm birth (Luke, 1995).
 Genetic Factors
Genetic Factors
The recurrent, familial, and racial nature of preterm birth has led to the suggestion that genetics may play a causal role. An accumulating literature on genetic variants buttresses this concept (Gibson, 2007; Hampton, 2006; Li, 2004; Macones, 2004). As discussed on page 839, several such studies have also implicated immunoregulatory genes in potentiating chorioamnionitis in cases of preterm delivery due to infection (Varner, 2005).
Birth Defects
In a secondary analysis of data from the First- and Second-Trimester Evaluation of Risk (FASTER) Trial, it was found that birth defects were associated with preterm birth and low birthweight (Dolan, 2007).
 Periodontal Disease
Periodontal Disease
Gum inflammation is a chronic anaerobic inflammation that affects as many as 50 percent of pregnant women in the United States (Goepfert, 2004). Vergnes and Sixou (2007) performed a metaanalysis of 17 studies and concluded that periodontal disease was significantly associated with preterm birth—odds ratio 2.83. The researchers concluded, however, that the data were not robust enough to recommend screening and treatment of pregnant women (Stamilio, 2007).
To better study the relationship with periodontitis, Michalowicz (2006) randomly assigned 813 pregnant women between 13 and 17 weeks’ gestation who had periodontal disease to treatment during pregnancy or postpartum. They found that treatment during pregnancy improved periodontal disease and that it is safe. However, treatment failed to significantly alter preterm birth rates.
 Interval between Pregnancies
Interval between Pregnancies
Short intervals between pregnancies have been known for some time to be associated with adverse perinatal outcomes. In a metaanalysis, Conde-Agudelo and colleagues (2006) reported that intervals < 18 months and > 59 months were associated with increased risks for both preterm birth and small-for-gestational age newborns.
 Prior Preterm Birth
Prior Preterm Birth
A major risk factor for preterm labor is prior preterm delivery (Spong, 2007). Shown in Table 42-6 is the incidence of recurrent preterm birth in nearly 16,000 women delivered at Parkland Hospital. The recurrent preterm delivery risk for women whose first delivery was preterm was increased threefold compared with that of women whose first neonate was born at term. More than a third of women whose first two newborns were preterm subsequently delivered a third preterm newborn. Most—70 percent—of the recurrent births in this study occurred within 2 weeks of the gestational age of the prior preterm delivery. Importantly, the causes of prior preterm delivery also recurred.
TABLE 42-6. Recurrent Spontaneous Preterm Births According to Prior Outcome

Although women with prior preterm births are clearly at risk for recurrence, they contributed only 10 percent of the total preterm births in this study. Expressed another way, 90 percent of the preterm births at Parkland Hospital cannot be predicted based on a history of preterm birth. Extrapolating data from the 2003 revised birth certificates, it is estimated that approximately 2.5 percent of women delivered in 2004 had a history of prior preterm birth (Martin, 2007).
 Infection
Infection
As discussed, a link between preterm birth and infection seems irrefutable. Goldenberg and coworkers (2008) have reviewed this association. Intrauterine infections are believed to trigger preterm labor by activation of the innate immune system. In this hypothesis, microorganisms elicit release of inflammatory cytokines such as interleukins and TNF-α, which in turn stimulate the production of prostaglandin and/or matrix-degrading enzymes. Prostaglandins stimulate uterine contractions, whereas degradation of extracellular matrix in the fetal membranes leads to preterm rupture of membranes. It is estimated that 25 to 40 percent of preterm births result from intrauterine infection. The basic science of preterm birth due to infection is discussed at length beginning on page 838.
In several studies, antimicrobial treatment has been given to prevent preterm labor due to microbial invasion. Based on available data, these strategies especially targeted mycoplasma species. Morency and colleagues (2007) performed a metaanalysis of 61 articles and suggested that antimicrobials given in the second trimester may prevent subsequent preterm birth. Andrews and associates (2006) reported results of a double-blind interconceptional trial in which they gave a course of azithromycin plus metronidazole every 4 months to 241 nonpregnant women whose last pregnancy resulted in spontaneous delivery before 34 weeks. Approximately 80 percent of the women with subsequent pregnancies had received study drug within 6 months of their subsequent conception. Such interconceptional antimicrobial treatment did not reduce the rate of recurrent preterm birth. Tita and coworkers (2007) performed a subgroup analysis of these same data and concluded that such use of antimicrobials may be harmful. In another study, Goldenberg and colleagues (2006) randomized 2661 women at four African sites to placebo or metronidazole plus erythromycin between 20 and 24 weeks’ gestation followed by ampicillin plus metronidazole during labor. This antimicrobial regimen did not reduce the rate of preterm birth or that of histological chorioamnionitis.
Bacterial Vaginosis
In this condition, normal, hydrogen peroxide-producing, lactobacillus-predominant vaginal flora is replaced with anaerobes that include Gardnerella vaginalis, Mobiluncus species, and Mycoplasma hominis (Hillier, 1995; Nugent, 1991). Its diagnosis and management are discussed in Chapter 65 (p. 1276). Using Gram staining, relative concentrations of the bacterial morphotypes characteristic of bacterial vaginosis are determined and graded as the Nugent score.
Bacterial vaginosis has been associated with spontaneous abortion, preterm labor, PPROM, chorioamnionitis, and amnionic fluid infection (Hillier, 1995; Kurki, 1992; Leitich, 2003a,b). Environmental factors appear to be important in bacterial vaginosis development. Exposure to chronic stress, ethnic differences, and frequent or recent douching have all been associated with increased rates of the condition (Culhane, 2002; Ness, 2002). A gene-environment interaction has been described (Macones, 2004). Women with bacterial vaginosis and a susceptible TNF-α genotype had a ninefold increased incidence of preterm birth. From all of these studies, there seems no doubt that adverse vaginal flora is associated in some way with spontaneous preterm birth. Unfortunately, to date, screening and treatment have not been shown to prevent preterm birth. Indeed, microbial resistance or antimicrobial-induced change in the vaginal flora has been reported as a result of regimens intended to eliminate bacterial vaginosis (Beigi, 2004; Carey, 2005). Okun and associates (2005) performed a systematic review of antibiotics given for bacterial vaginosis and for Trichomonas vaginalis. They found no evidence to support such use for the prevention of preterm birth in either low-risk or high-risk women.
DIAGNOSIS
Preterm labor is primarily diagnosed by symptoms and physical examination. Sonography is used to identify asymptomatic cervical dilation and effacement.
 Symptoms
Symptoms
Early differentiation between true and false labor is difficult before there is demonstrable cervical effacement and dilatation. Uterine activity alone can be misleading because of Braxton Hicks contractions, which are discussed in detail in Chapter 21 (p. 409). These contractions, described as irregular, nonrhythmical, and either painful or painless, can cause considerable confusion in the diagnosis of true preterm labor. Not infrequently, women who deliver before term have uterine activity that is attributed to Braxton Hicks contractions, prompting an incorrect diagnosis of false labor. Accordingly, the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (2012) define preterm labor to be regular contractions before 37 weeks that are associated with cervical change.
In addition to painful or painless uterine contractions, symptoms such as pelvic pressure, menstrual-like cramps, watery vaginal discharge, and lower back pain have been empirically associated with impending preterm birth. Such complaints are thought by some to be common in normal pregnancy and are therefore often dismissed by patients, clinicians, and nurses.
The importance of these symptoms as a harbinger of labor has been emphasized by some but not all investigators (Iams, 1990; Kragt, 1990). Iams and coworkers (1994) found that the signs and symptoms signaling preterm labor, including uterine contractions, appeared only within 24 hours of preterm labor.
Chao (2011) prospectively studied 843 women with singletons who presented to Parkland Hospital with preterm labor symptoms, between 240/7 and 336/7 weeks, intact membranes, and cervical dilation < 2 cm. These women underwent electronic fetal and uterine contraction monitoring for 2 hours. Those whose cervix remained < 2 cm were sent home with a diagnosis of false preterm labor. When analyzed compared with the general obstetrical population, women sent home had a similar and nonsignificant rate of birth before 34 weeks—2 versus 1 percent. However, these women had a significantly higher rate of birth between 34 and 36 weeks—5 percent compared with 2 percent. Women with cervical dilation of 1 cm at discharge were significantly more likely to deliver before 34 weeks compared with women without cervical dilatation—5 percent versus 1 percent. Importantly, almost 90 percent of the 1-cm group delivered > 21 days after the initial presentation.
 Cervical Change
Cervical Change
Dilatation
Researchers have evaluated asymptomatic cervical changes that may presage and thus predict preterm labor. Asymptomatic cervical dilatation after midpregnancy is suspected to be a risk factor for preterm delivery, although some clinicians consider it to be a normal anatomical variant. Moreover, study results have suggested that parity alone is not sufficient to explain cervical dilatation discovered early in the third trimester. Cook (1996) longitudinally evaluated cervical status with transvaginal sonography between 18 and 30 weeks in both nulliparous and parous women who all subsequently gave birth at term. Cervical length and diameter were identical in both groups throughout these critical weeks. In a study from Parkland Hospital, routine digital cervical examinations were performed between 26 and 30 weeks in 185 women. Approximately 25 percent of women whose cervix was dilated 2 or 3 cm delivered before 34 weeks. Other investigators have verified cervical dilatation as a predictor of increased preterm delivery risk (Copper, 1995; Pereira, 2007).
Although women with dilatation and effacement in the third trimester are at increased risk for preterm birth, detection does not improve pregnancy outcome. Buekens and associates (1994) randomly assigned 2719 women to undergo routine cervical examinations at each prenatal visit and compared them with 2721 women in whom serial examinations were not performed. Knowledge of antenatal cervical dilatation did not affect any pregnancy outcome related to preterm birth or the frequency of interventions for preterm labor. The investigators also reported that cervical examinations were not related to preterm membrane rupture. At this time, it seems that prenatal cervical examinations are neither beneficial nor harmful.
Length
Vaginal-probe sonographic cervical assessment has been evaluated extensively during the past two decades. When performed by trained operators, cervical length analysis using transvaginal sonography is safe, highly reproducible, and more predictive than transabdominal sonographic screening (American College of Obstetricians and Gynecologists, 2012b). Unlike the transabdominal approach, transvaginal cervical sonography is not affected by maternal obesity, cervix position, or shadowing from the fetal presenting part. Technique is important, and Yost and colleagues (1999) have cautioned that special expertise is needed. Iams and coworkers (1996) measured cervical length at approximately 24 weeks’ gestation and again at 28 weeks in 2915 women not at risk for preterm birth. The mean cervical length at 24 weeks was approximately 35 mm, and those women with progressively shorter cervices experienced increased rates of preterm birth.
Until recently, routine cervical length evaluation in women at low risk was not advocated because, like other factors associated with potentially higher preterm birth risk, no effective treatments were available. Randomized trials done to investigate vaginal progesterone use in women with short cervix diagnosed during screening have stimulated consideration of whether or not such screening is warranted (Fonseca, 2007; Hassan, 2011). These trials are discussed subsequently on page 844.
 Ambulatory Uterine Monitoring
Ambulatory Uterine Monitoring
An external tocodynamometer belted around the abdomen and connected to an electronic waist recorder allows a woman to ambulate while uterine activity is recorded. Results are transmitted via telephone daily. Women are educated concerning signs and symptoms of preterm labor, and clinicians are kept apprised of their progress. The 1985 approval of this monitor by the Food and Drug Administration (FDA) prompted its widespread clinical use. Subsequently, the American College of Obstetricians and Gynecologists (1995) concluded that the use of this expensive, bulky, and time-consuming system does not reduce preterm birth rates. A subsequent study by the Collaborative Home Uterine Monitoring Study Group (1995) confirmed these conclusions. And Iams and associates (2002) analyzed data from almost 35,000 hours of daily home monitoring and verified that no contraction pattern efficiently predicted preterm birth. The American College of Obstetricians and Gynecologists (2012a) does not recommend home uterine activity monitoring.
 Fetal Fibronectin
Fetal Fibronectin
This glycoprotein is produced in 20 different molecular forms by various cell types, including hepatocytes, fibroblasts, endothelial cells, and fetal amnion. Present in high concentrations in maternal blood and in amnionic fluid, it is thought to function in intercellular adhesion during implantation and in maintenance of placental adherence to uterine decidua (Leeson, 1996). Fetal fibronectin is detected in cervicovaginal secretions in women who have normal pregnancies with intact membranes at term. It appears to reflect stromal remodeling of the cervix before labor.
Lockwood (1991) reported that fibronectin detection in cervicovaginal secretions before membrane rupture was a possible marker for impending preterm labor. Fetal fibronectin is measured using an enzyme-linked immunosorbent assay, and values exceeding 50 ng/mL are considered positive. Sample contamination by amnionic fluid and maternal blood should be avoided. Interventional studies based on the use of fetal fibronectin screening in asymptomatic women have not demonstrated improved perinatal outcomes (Andrews, 2003; Grobman, 2004). The American College of Obstetricians and Gynecologists (2012b) does not recommend screening with fetal fibronectin tests.
PRETERM BIRTH PREVENTION
Prevention of preterm birth has been an elusive goal. Recent reports, however, suggest that prevention in selected populations may be achievable.
 Cervical Cerclage
Cervical Cerclage
There are at least three circumstances when cerclage placement may be used to prevent preterm birth. Two are done prophylactically, and a third is done for treatment. The first prophylactic cerclage is used in women who have a history of recurrent midtrimester losses and who are diagnosed with cervical insufficiency (Chap. 18, p. 360). The second prophylactic cerclage is for women identified during sonographic examination to have a short cervix. The third indication is “rescue” cerclage, done emergently when cervical incompetence is recognized in women with threatened preterm labor.
For women with a short cervix detected by sonography, Berghella and colleagues (2005) reviewed several small trials of cerclage in this group and concluded that cerclage may reduce preterm birth rates in those women with a prior preterm birth. Owen (2009) randomly assigned 302 women with prior preterm birth from 16 centers with a short cervix—defined as length < 25 mm—to cerclage or no procedure. Women with a cervical length < 15 mm delivered before 35 weeks significantly less often following cerclage compared with women with no cerclage—30 versus 65 percent. This study suggests that recurrent preterm birth can be prevented in a subset of women who have a history of prior preterm births.
In a multinational study, To and associates (2004) screened 47,123 women and randomized the 253 women with cervices < 15 mm to cerclage or no cerclage. The frequency of preterm delivery < 33 weeks was not significantly different between the treatment groups. Thus, cerclage for sonographically detected short cervix alone has not been found to be beneficial. In contrast, women with a very short cervix, that is, < 15 mm, and a history of prior preterm birth may benefit.
 Prophylaxis with Progestin Compounds
Prophylaxis with Progestin Compounds
Progesterone levels in most mammals fall rapidly before the onset of labor. This is termed progesterone withdrawal and is considered to be a parturition-triggering event. During human parturition, however, maternal, fetal, and amnionic fluid progesterone levels remain elevated with no decline. It has been proposed that human parturition involves functional progesterone withdrawal mediated by decreased progesterone activity of progesterone receptors (Ziyan, 2010). It follows conceptually that the administration of progesterone to maintain uterine quiescence may block preterm labor. This hypothesis has stimulated several studies in the past half century.
 Prior Preterm Birth and Progestin Compounds
Prior Preterm Birth and Progestin Compounds
Initial Studies
Studies in the past 15 years have included several investigations to evaluate progestin compounds given prophylactically. A pivotal study was done by the MFMU Network to evaluate prophylactic progestin treatment for women at high-risk for recurrent preterm birth (Meis, 2003). In this trial, 310 women with a prior preterm birth were randomized to receive 17-hydroxyprogesterone caproate (17-OHPC) (Romero, 2013). Another 153 women received placebo, and these were administered as weekly intramuscular injections of either inert oil or 17-OHPC from 16 through 36 weeks’ gestation. Delivery rates before 37, 35, and 32 weeks were all significantly reduced by 17-OHPC therapy. At the same time, however, similar studies of 17-OHPC in both twins and triplets done by the Network showed no improvement in preterm birth rates (Caritis, 2009; Rouse, 2007).
The 17-OHPC study by Meis and colleagues (2003) has been challenged because of the unexpectedly high preterm delivery rate in the placebo arm of the trial. Fifty-five percent delivered rather than the expected rate of 36 percent, which was derived from a pretrial cohort (Romero, 2013). The criticism is that 17-OHPC may have been shown to be effective only because the placebo group was distorted by this high 55-percent preterm delivery rate. This compared with the 36-percent rate, which was actually observed when women were treated with 17-OHPC in the trial. To further elucidate this disparity, a confirmation trial by the Network is underway.
Also in contrast to the 17-OHPC study by Meis and coworkers (2003), O’Brien and associates (2007) randomly assigned 659 women with a prior preterm birth to treatment with daily vaginal progesterone gel (90 mg) or placebo. They found no differences in preterm birth rates.
Subsequent Studies
Perhaps no other topic in contemporary obstetrics has generated as much interest and debate since the 23rd edition of Williams Obstetrics as has the use of progestins to prevent preterm birth. At the center of the controversy is whether or not progestins prevent preterm birth in women with a singleton pregnancy but without prior preterm birth—especially nulliparous women. If progestins are effective in women at low risk for preterm birth, this would justify sonographic screening of all pregnant women to detect short cervices (Silver, 2011).
Three randomized trials are at the center of the controversy, and these are summarized in Table 42-7. Fonseca and colleagues (2007) randomly assigned 250 women with sonographically short cervices—15 mm or less—identified during routine prenatal care. Women were given nightly 200-mg micronized progesterone vaginal capsules or placebo from 24 to 34 weeks’ gestation. As shown in Table 42-7, spontaneous delivery before 34 weeks was significantly reduced by progesterone therapy. Importantly, this trial included not only nulliparous women but also those with twins or prior preterm birth.
TABLE 42-7. Randomized Trials of Progestin Compounds Given Prophylactically to Prevent Preterm Labor
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree