Introduction
Cardiovascular disease (CVD) is the leading cause of death among women in the United States. An increasing body of evidence indicates that pregnancy-related morbidities, including preeclampsia, placental infarction, and abruption, are associated with the development of subsequent CVD and can be referred to as maternal placental syndromes (PS). Furthermore, the adverse pregnancy outcomes of preterm delivery, and infants born small for gestational age (SGA), resulting from intrauterine growth restriction, may be referred to as fetal PS and also appear to confer CVD risk.
Both retrospective and prospective epidemiological studies have reported associations between hypertensive disorders of pregnancy, preterm birth (PTB), and maternal PS and an increased risk of future CVD. While most of these studies focus on long-term CVD risk, up to 15 years after giving birth, limited data exist regarding the short-term risk of CVD. CVD occurring within the first 5 years of the index delivery will likely occur in the mother’s reproductive lifespan and therefore lead to further morbidity in subsequent pregnancies. No prior research investigates the impact of PS and subsequent CVD on health care utilization or costs. We hypothesized that the short-term risk of CVD (within 5 years of first pregnancy) would be increased among women with maternal PS. Additionally we examined health care utilization and direct medical costs in the years immediately following pregnancy with and without placental complications.
Materials and Methods
Design, data source, and study population
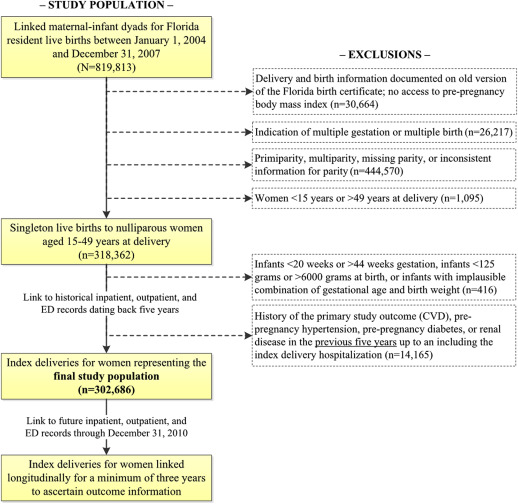
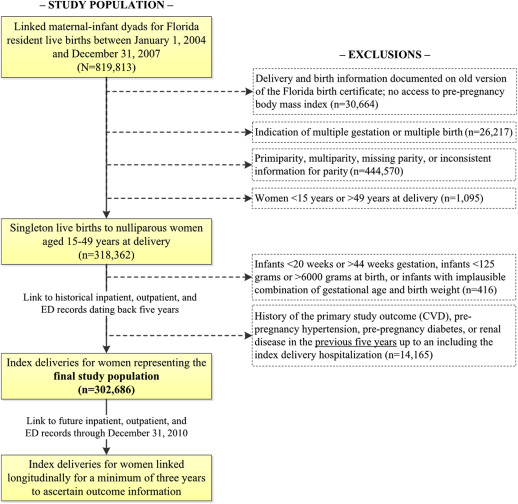
We conducted a population-based retrospective cohort study using a statewide maternal and infant longitudinally linked database. For Florida-resident births from 1998 through 2009, birth certificates were linked both to infant birth and maternal delivery hospitalization discharge records using a hierarchical deterministic linking strategy. After establishing events that occur at birth, we then linked in death certificates and all subsequent infant and maternal inpatient, outpatient, and emergency department discharge records available through the end of follow-up (Dec. 31, 2010). For mothers, we also linked to all hospital discharge data preceding the index pregnancy, as far back as Jan. 1, 1998. Details of the data linkage process, which achieved >92% linkage rate, and an evaluation of the validity and reliability of database have been published previously. The study population consisted initially of 318,362 nulliparous pregnant women and girls aged 15-49 years who gave birth to a live born singleton infant from Jan. 1, 2004, through Dec. 31, 2007 ( Figure 1 ). This time frame was chosen to review medical history in the 5-year period before pregnancy, incorporate potential confounders present only on the new version of the Florida birth certificate, and allow for a minimum of 3 years of follow-up after the index delivery. Women diagnosed with prepregnancy CVD, hypertension, diabetes, or renal disease in the 5-year period before the index delivery hospitalization (n = 14,165) and those giving birth to infants with implausible gestational age-birthweight combinations based on national fetal growth curves (n = 416) were excluded. The final study population consisted of 302,686 women and girls.
PS and adverse infant outcomes
Using International Classification of Diseases, Ninth Revision, Clinical Modification ( ICD-9-CM ) diagnosis codes from discharge records, supplemented with birth certificate indicators to improve sensitivity, we determined whether each mother had a PS–preeclampsia (642.4, 642.5), eclampsia (642.6 or birth certificate indicator), gestational hypertension (642.3 or birth certificate indicator), placental infarction (656.7), or placental abruption (641.2)–diagnosed during her index delivery hospitalization. Three exposures were used in analyses: (1) a 2-level “any PS” variable; (2) a 5-level variable to capture the nature and number of PS conditions; and (3) a 4-level variable that combined PS with PTB (20-37 weeks’ gestation) and SGA (birthweight <10th percentile for gestational age).
Cardiovascular health outcomes
The primary outcome was incident CVD, operationalized as presence of ≥1 ICD-9-CM diagnosis codes indicative of coronary heart disease, cerebrovascular disease, peripheral artery disease, or congestive heart failure, or an ICD-9-CM procedure code for cardiac or peripheral arterial revascularization. To prevent capturing the immediate effect of the index delivery on risk of CVD, assessment of CVD included encounters taking place ≥90 days after discharge from the index delivery hospitalization. Follow-up continued through Dec. 31, 2010. A detailed list of the ICD-9-CM codes used to define CVD is presented in the Appendix .
Health care utilization indices
We explored the associations between PS and 3 indicators of health care utilization: (1) number of encounters, (2) length of stay (LOS) across encounters, and (3) cost of providing direct medical care. The number of encounters was calculated as the number of unique inpatient, outpatient, and emergency department discharge records with date of admission ≥90 days after discharge from the index delivery hospitalization. To calculate LOS in days for any type of encounter, we subtracted the dates of admission and discharge. Same day visits were assigned an LOS of 1 day since these hospitalizations constitute a distinct stay and are billed as 1 day for room/board. For each woman or girl, the number of days across all admissions was summed. Hospital discharge records in our linked database contain detailed department-level charges for each encounter. Charges reflect what a hospital bills for services and are a poor estimate of actual cost. The degree of markup from cost to billed charges varies considerably across hospitals, departments within the same hospital, and over time. We developed an algorithm to convert charges to cost using time-, hospital-, and department-specific cost-to-charge ratios from hospital cost reports, and further adjusted estimates for inflation to 2010 dollars using the medical care component of the Consumer Price Index. Due to the lack of reliable cost-to-charge ratio to fit our data, outpatient visits were not included in determining the cost of medical care during follow-up.
To remove the impact of subsequent pregnancies on health care utilization metrics, we excluded nonindex delivery hospitalizations. We stratified total LOS and direct medical costs into those occurring during the index delivery hospitalization and during the post-90-day follow-up period.
Sociodemographic, behavioral, and clinical covariates
Using both birth certificate and ICD-9-CM codes, we examined sociodemographic characteristics (age at the index delivery, race/ethnicity, nativity, education, and per-capita income), health behaviors (tobacco, alcohol, and drug use), clinical comorbidities (a 5-year history of hyperlipidemia, migraine, and lupus), prepregnancy body mass index (BMI), and gestational diabetes that could plausibly confound the associations between PS and the study outcomes. Specific ICD-9-CM codes and birth certificate indicator variables used are provided in the Appendix .
Statistical analysis
Descriptive statistics were used to describe the distribution of nulliparous women with and without a PS by sociodemographic, clinical, behavioral, and infant characteristics. The χ 2 test (categorical data) and independent-samples t tests or Wilcoxon-Mann-Whitney tests (continuous data) were used to assess the statistical significance of bivariate associations. Kaplan-Meier curves were used to describe the risk of incident CVD for women with and without PS, and Cox proportional hazards regression was used to calculate hazard ratios (HR) and 95% confidence intervals (CI) that represent the association between PS and time to CVD. Women and girls were censored if they did not experience a CVD-related event by Dec. 31, 2010. Ties, in which ≥2 women or girls experience a CVD at the same recorded time, were handled using the Efron approximation. The proportional hazards assumption was assessed using plots of Schoenfeld residuals versus time; linearity was examined using plots of Martingale residuals and each covariate. To compare mean health care utilization indices across exposure and outcome groups, we used generalized linear modeling to calculate adjusted measures of association (eg, cost ratios) and 95% CIs. Due to the positively skewed nature of LOS and cost data, we considered various nonnormal distributions with the best-fitting model selected based on Akaike information criterion. For each exposure-outcome association, 3 multivariable models were constructed to demonstrate the relative confounding effects of 3 types of factors: (1) adjusting for sociodemographic characteristics; (2) additional adjustment for 5-year history of hyperlipidemia, migraine, and lupus; and (3) additional adjustment for prepregnancy BMI, gestational diabetes, and tobacco, drug, and alcohol use during the index pregnancy.
We conducted sensitivity analyses to evaluate the robustness of our results to alternative eligibility criteria and model inputs. Although index pregnancies in the current study were only nulliparous women and girls, subsequent pregnancies may have occurred during the follow-up period. These pregnancies could increase the risk of CVD independent of PS during the index pregnancy. Therefore, we re-ran all analyses after restricting to women and girls with no subsequent deliveries. Our cost analyses did not include outpatient visits, therefore we analyzed charges among all encounters, and compared calculated charge ratios to cost ratios. All analyses were conducted using software (SAS 9.4; SAS Institute Inc, Cary, NC) using a 5% type I error rate and 2-sided hypothesis tests. The linked database was deidentified prior to use and the study was approved by the institutional review boards of the Florida Department of Health, University of South Florida, and Baylor College of Medicine.
Materials and Methods
Design, data source, and study population
We conducted a population-based retrospective cohort study using a statewide maternal and infant longitudinally linked database. For Florida-resident births from 1998 through 2009, birth certificates were linked both to infant birth and maternal delivery hospitalization discharge records using a hierarchical deterministic linking strategy. After establishing events that occur at birth, we then linked in death certificates and all subsequent infant and maternal inpatient, outpatient, and emergency department discharge records available through the end of follow-up (Dec. 31, 2010). For mothers, we also linked to all hospital discharge data preceding the index pregnancy, as far back as Jan. 1, 1998. Details of the data linkage process, which achieved >92% linkage rate, and an evaluation of the validity and reliability of database have been published previously. The study population consisted initially of 318,362 nulliparous pregnant women and girls aged 15-49 years who gave birth to a live born singleton infant from Jan. 1, 2004, through Dec. 31, 2007 ( Figure 1 ). This time frame was chosen to review medical history in the 5-year period before pregnancy, incorporate potential confounders present only on the new version of the Florida birth certificate, and allow for a minimum of 3 years of follow-up after the index delivery. Women diagnosed with prepregnancy CVD, hypertension, diabetes, or renal disease in the 5-year period before the index delivery hospitalization (n = 14,165) and those giving birth to infants with implausible gestational age-birthweight combinations based on national fetal growth curves (n = 416) were excluded. The final study population consisted of 302,686 women and girls.
PS and adverse infant outcomes
Using International Classification of Diseases, Ninth Revision, Clinical Modification ( ICD-9-CM ) diagnosis codes from discharge records, supplemented with birth certificate indicators to improve sensitivity, we determined whether each mother had a PS–preeclampsia (642.4, 642.5), eclampsia (642.6 or birth certificate indicator), gestational hypertension (642.3 or birth certificate indicator), placental infarction (656.7), or placental abruption (641.2)–diagnosed during her index delivery hospitalization. Three exposures were used in analyses: (1) a 2-level “any PS” variable; (2) a 5-level variable to capture the nature and number of PS conditions; and (3) a 4-level variable that combined PS with PTB (20-37 weeks’ gestation) and SGA (birthweight <10th percentile for gestational age).
Cardiovascular health outcomes
The primary outcome was incident CVD, operationalized as presence of ≥1 ICD-9-CM diagnosis codes indicative of coronary heart disease, cerebrovascular disease, peripheral artery disease, or congestive heart failure, or an ICD-9-CM procedure code for cardiac or peripheral arterial revascularization. To prevent capturing the immediate effect of the index delivery on risk of CVD, assessment of CVD included encounters taking place ≥90 days after discharge from the index delivery hospitalization. Follow-up continued through Dec. 31, 2010. A detailed list of the ICD-9-CM codes used to define CVD is presented in the Appendix .
Health care utilization indices
We explored the associations between PS and 3 indicators of health care utilization: (1) number of encounters, (2) length of stay (LOS) across encounters, and (3) cost of providing direct medical care. The number of encounters was calculated as the number of unique inpatient, outpatient, and emergency department discharge records with date of admission ≥90 days after discharge from the index delivery hospitalization. To calculate LOS in days for any type of encounter, we subtracted the dates of admission and discharge. Same day visits were assigned an LOS of 1 day since these hospitalizations constitute a distinct stay and are billed as 1 day for room/board. For each woman or girl, the number of days across all admissions was summed. Hospital discharge records in our linked database contain detailed department-level charges for each encounter. Charges reflect what a hospital bills for services and are a poor estimate of actual cost. The degree of markup from cost to billed charges varies considerably across hospitals, departments within the same hospital, and over time. We developed an algorithm to convert charges to cost using time-, hospital-, and department-specific cost-to-charge ratios from hospital cost reports, and further adjusted estimates for inflation to 2010 dollars using the medical care component of the Consumer Price Index. Due to the lack of reliable cost-to-charge ratio to fit our data, outpatient visits were not included in determining the cost of medical care during follow-up.
To remove the impact of subsequent pregnancies on health care utilization metrics, we excluded nonindex delivery hospitalizations. We stratified total LOS and direct medical costs into those occurring during the index delivery hospitalization and during the post-90-day follow-up period.
Sociodemographic, behavioral, and clinical covariates
Using both birth certificate and ICD-9-CM codes, we examined sociodemographic characteristics (age at the index delivery, race/ethnicity, nativity, education, and per-capita income), health behaviors (tobacco, alcohol, and drug use), clinical comorbidities (a 5-year history of hyperlipidemia, migraine, and lupus), prepregnancy body mass index (BMI), and gestational diabetes that could plausibly confound the associations between PS and the study outcomes. Specific ICD-9-CM codes and birth certificate indicator variables used are provided in the Appendix .
Statistical analysis
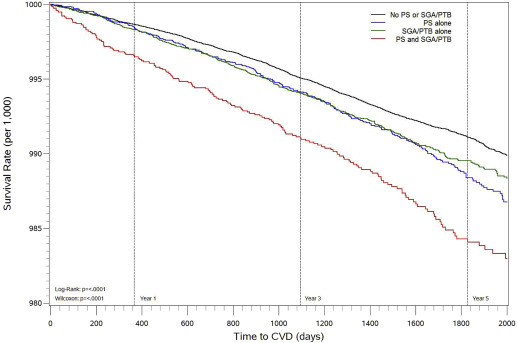
Descriptive statistics were used to describe the distribution of nulliparous women with and without a PS by sociodemographic, clinical, behavioral, and infant characteristics. The χ 2 test (categorical data) and independent-samples t tests or Wilcoxon-Mann-Whitney tests (continuous data) were used to assess the statistical significance of bivariate associations. Kaplan-Meier curves were used to describe the risk of incident CVD for women with and without PS, and Cox proportional hazards regression was used to calculate hazard ratios (HR) and 95% confidence intervals (CI) that represent the association between PS and time to CVD. Women and girls were censored if they did not experience a CVD-related event by Dec. 31, 2010. Ties, in which ≥2 women or girls experience a CVD at the same recorded time, were handled using the Efron approximation. The proportional hazards assumption was assessed using plots of Schoenfeld residuals versus time; linearity was examined using plots of Martingale residuals and each covariate. To compare mean health care utilization indices across exposure and outcome groups, we used generalized linear modeling to calculate adjusted measures of association (eg, cost ratios) and 95% CIs. Due to the positively skewed nature of LOS and cost data, we considered various nonnormal distributions with the best-fitting model selected based on Akaike information criterion. For each exposure-outcome association, 3 multivariable models were constructed to demonstrate the relative confounding effects of 3 types of factors: (1) adjusting for sociodemographic characteristics; (2) additional adjustment for 5-year history of hyperlipidemia, migraine, and lupus; and (3) additional adjustment for prepregnancy BMI, gestational diabetes, and tobacco, drug, and alcohol use during the index pregnancy.
We conducted sensitivity analyses to evaluate the robustness of our results to alternative eligibility criteria and model inputs. Although index pregnancies in the current study were only nulliparous women and girls, subsequent pregnancies may have occurred during the follow-up period. These pregnancies could increase the risk of CVD independent of PS during the index pregnancy. Therefore, we re-ran all analyses after restricting to women and girls with no subsequent deliveries. Our cost analyses did not include outpatient visits, therefore we analyzed charges among all encounters, and compared calculated charge ratios to cost ratios. All analyses were conducted using software (SAS 9.4; SAS Institute Inc, Cary, NC) using a 5% type I error rate and 2-sided hypothesis tests. The linked database was deidentified prior to use and the study was approved by the institutional review boards of the Florida Department of Health, University of South Florida, and Baylor College of Medicine.
Results
We identified 36,713 (13.8%) mothers with a PS during their index delivery hospitalization. Mothers with PS were more likely to be black non-Hispanic, have a high school education or less, have lower income, have a higher prepregnancy BMI, have gestational diabetes, and use illicit drugs during pregnancy ( Table 1 ). Infants of mothers with PS were more likely to be born preterm and be SGA.
| Characteristic a | Placental syndrome, N = 36,713 | No placental syndrome, N = 265,973 | P b |
|---|---|---|---|
| Follow-up time (days), median (Q1–Q3) c | 1770 (1428–2121) | 1775 (1433–2129) | .03 |
| Sociodemographics | |||
| Age, y, mean ± SD | 24.9 ± 6.1 | 25.1 ± 6.0 | <.01 |
| Race/ethnicity | <.01 | ||
| Non-Hispanic white | 19,139 (52.1) | 131,193 (49.3) | |
| Non-Hispanic black | 8325 (22.7) | 47,207 (17.7) | |
| Hispanic | 7840 (21.4) | 72,476 (27.2) | |
| Non-Hispanic other | 1247 (3.4) | 13,938 (5.2) | |
| Nativity, foreign-born | 7773 (21.2) | 78,250 (29.4) | <.01 |
| Education | <.01 | ||
| <High school | 6714 (18.3) | 46,812 (17.6) | |
| High school | 11,619 (31.6) | 79,405 (29.9) | |
| >High school | 18,172 (49.5) | 138,134 (51.9) | |
| Per-capita income, US$ d , median (Q1–Q3) | 23.6 (18.9–28.5) | 23.8 (19.4–29.5) | <.01 |
| Had another live birth | 13,472 (36.7) | 99,872 (37.5) | <.01 |
| Comorbidities, 5-y history | |||
| Hyperlipidemia | 52 (0.1) | 244 (0.1) | <.01 |
| Migraine | 433 (1.2) | 2059 (0.8) | <.01 |
| Lupus | 63 (0.2) | 230 (0.1) | <.01 |
| Comorbidities, current pregnancy | |||
| BMI, kg/m 2 , mean ± SD | 26.3 ± 6.5 | 24.2 ± 5.3 | <.01 |
| Prepregnancy BMI | <.01 | ||
| Underweight | 1529 (4.2) | 17,677 (6.6) | |
| Normal | 15,884 (43.3) | 148,153 (55.7) | |
| Overweight | 8720 (23.8) | 51,611 (19.4) | |
| Obese I | 4603 (12.5) | 20,392 (7.7) | |
| Obese II | 2208 (6.0) | 7784 (2.9) | |
| Obese III | 1428 (3.9) | 4206 (1.6) | |
| Gestational diabetes | 2733 (7.4) | 11,384 (4.3) | <.01 |
| Behavioral factors | |||
| Tobacco use during pregnancy | 2754 (7.5) | 20,470 (7.7) | .19 |
| Alcohol use during pregnancy | 142 (0.4) | 978 (0.4) | .57 |
| Drug use during pregnancy | 425 (1.2) | 2444 (0.9) | <.01 |
| Infant characteristics | |||
| Male sex | 18,919 (51.5) | 136,179 (51.2) | .23 |
| Small for gestational age | 6215 (16.9) | 26,603 (10.0) | <.01 |
| Preterm birth | 7517 (20.5) | 18,821 (7.1) | <.01 |
a Binary characteristics are presented as frequency and percentage that reflect presence of condition
b Generated from χ 2 test of statistical independence for categorical variables, and from independent samples t test or Wilcoxon-Mann-Whitney test for continuous variables
PS and risk of subsequent CVD
Women or girls with any PS were at a 39% higher risk of subsequently developing CVD than women or girls without PS (95% CI, 1.25–1.54) ( Table 2 ). The risk was reduced to 19% after adjusting for sociodemographic, clinical, and behavioral factors, and infant sex (95% CI, 1.07–1.32). Women or girls with >1 PS condition had the highest CVD risk (HR, 1.43; 95% CI, 1.20–1.70), followed by those with eclampsia/preeclampsia alone (HR, 1.42; 95% CI, 1.14–1.76). Although women or girls with gestational hypertension alone experienced an 18% increased crude risk of CVD, the risk was not significant after adjustment for confounders. When PS was combined with PTB and/or SGA, the adjusted risk of CVD increased 45% (95% CI, 1.24–1.71) ( Figure 2 ). Women and girls with PS without PTB or SGA did not demonstrate increased CVD risk, relative to women and girls without PS, PTB, or SGA.
| Exposure category | CVD cases | CVD rate b | Unadjusted model HR (95% CI) | Adjusted model 1 c HR (95% CI) | Adjusted model 2 d HR (95% CI) | Adjusted model 3 e HR (95% CI) |
|---|---|---|---|---|---|---|
| Any PS | ||||||
| No | 2269 | 8.5 | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Yes | 432 | 11.8 | 1.39 (1.25–1.54) f | 1.27 (1.14–1.40) f | 1.26 (1.13–1.39) f | 1.19 (1.07–1.32) f |
| Nature/no. of PS conditions | ||||||
| No PS | 2269 | 8.5 | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Eclampsia/preeclampsia alone | 87 | 13.7 | 1.60 (1.29–1.98) f | 1.48 (1.20–1.84) f | 1.47 (1.18–1.82) f | 1.42 (1.14–1.76) f |
| Gestational hypertension alone | 178 | 10.0 | 1.18 (1.01–1.37) f | 1.07 (0.91–1.24) | 1.06 (0.91–1.24) | 0.99 (0.85–1.16) |
| Placental abruption/infarction alone | 32 | 10.5 | 1.22 (0.86–1.73) | 1.12 (0.78–1.60) | 1.12 (0.78–1.60) | 1.09 (0.76–1.57) |
| More than one placental syndrome condition | 135 | 14.3 | 1.69 (1.42–2.01) f | 1.54 (1.29–1.83) f | 1.53 (1.28–1.82) f | 1.43 (1.20–1.70) f |
| PS and adverse infant outcomes | ||||||
| No PS, no PTB, no SGA | 1854 | 8.3 | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| PS alone | 268 | 10.7 | 1.29 (1.14–1.47) f | 1.16 (1.02–1.32) f | 1.16 (1.02–1.32) f | 1.08 (0.95–1.23) |
| PTB/SGA alone | 415 | 9.6 | 1.16 (1.04–1.29) f | 1.10 (0.99–1.22) | 1.10 (0.98–1.22) | 1.07 (0.96–1.20) |
| PS and PTB/SGA | 164 | 14.1 | 1.70 (1.45–2.00) f | 1.56 (1.33–1.83) f | 1.54 (1.31–1.81) f | 1.45 (1.24–1.71) f |
a Composite indicator including diagnosis of ischemic heart disease, cerebrovascular disease, peripheral artery disease, congestive heart failure, and certain operations on cardiovascular system
b Rate expressed as no. of incident CVD cases per 1000 women
c Crude model + adjusted for maternal age, race/ethnicity, nativity, education, and income
d Adjusted model 1 + adjusted for 5-y history of hyperlipidemia, migraine, and lupus
e Adjusted model 2 + adjusted for prepregnancy body mass index, gestational diabetes, tobacco use, drug use, and infant sex