Fig. 31.1
Classification of sequelae of infantile septic arthritis of the hip. Type I: No residual deformity (Type IA) or mild coxa magna (Type IB). Type II: Coxa breva with a deformed head (Type IIA) or progressive coxa vara or valga due to asymmetrical, premature physeal closure (Type IIB). Type III: Slipping at the femoral neck, resulting in coxa vara or valga with severe anteversion or retroversion (Type IIIA) or pseudarthrosis of the femoral neck (Type IIIB). Type IV: Destruction of the femoral head and neck, with a small remnant of the neck (Type IVA) or complete loss of the femoral head and neck and no articulation of the hip (Type IVB)
One common drawback of all the aforementioned radiological classifications is that they were mainly devised based on the changes noted on the plain radiographs. Currently, with the help of modern, advanced imaging technologies, e.g., MRI and 3D-CT, deformed osteocartilaginous geometry of the proximal femur can be better visualized in three dimensions, and the dynamics of articular motion between the deformed FH and acetabulum can be better understood. A new, comprehensive three-dimensional radiological classification is anticipated considering the rapid advancement in the imaging technology.
Late Operative Treatment Modalities for Residual Deformities of Septic Arthritis of the Hip
Treatment modalities for the long-term sequelae of infantile septic arthritis of the hip are outlined in Table 31.1. The recommended primary and secondary treatment methods are as varied as the types of deformities. Unfortunately, no definite primary treatment for a severely damaged hip joint makes the affected joint capable of withstanding the forces imposed on it by otherwise healthy children with their long-term physical demands [1]. Thus, any surgical treatment for severe sequelae must be regarded as a measure that temporarily improves the clinical function and delays the more definitive procedures that are reserved for adult patients [1, 2]. The pearls and pitfalls in the management of late sequelae of infantile septic arthritis of the hip are summarized in Table 31.2.
Table 31.1
Late operative treatment modalities for severe sequelae of infantile septic arthritis of the hip
Purpose | Indications | Procedures |
|---|---|---|
To reduce/contain the hip joint | Subluxation or dislocation | Open reduction; soft-tissue release (adductor-iliopsoas tenotomy) |
To optimize joint congruity | Incongruity | Proximal femoral realignment osteotomy (varus or valgus osteotomy with a sagittal or rotational component); redirectional acetabular osteotomy (Salter, Pemberton, Dega osteotomy, triple innominate osteotomy, Ganz periacetabular osteotomy) |
To improve femoral head coverage | Uncovered femoral head | Redirectional acetabular osteotomy; salvage acetabuloplasty (e.g., Chiari, shelf operation); Ganz femoral head reduction osteotomy |
To reduce cam or pincer lesion | Femoroacetabular impingement | Osteochondroplasty via safe surgical hip dislocation or arthroscopy; excision of the femoral head and neck remnant (Choi Type IVA or mobile nonunion type of IIIB) |
To address intra-articular pathology of the cartilage or labrum | Torn labrum or articular cartilage lesion | Labral debridement or refixation; articular cartilage repair using microfracture technique or osteochondral grafting or chondrocyte transplantation |
To correct acetabular dysplasia | Dysplastic acetabulum | Redirectional acetabular osteotomy (e.g., Salter, Pemberton, Dega, triple innominate osteotomy, Ganz periacetabular osteotomy) |
To correct abnormal version of the proximal femur and acetabulum | Anteverted or retroverted femur and acetabulum | Proximal femoral rotational/derotational osteotomy; redirectional acetabular osteotomy (e.g., triple innominate osteotomy, Ganz periacetabular osteotomy) |
To improve abductor muscle function; to correct coxa brevis | Greater trochanteric overriding; short femoral neck | Greater trochanteric advancement; true or relative femoral neck lengthening |
To repair pseudarthrosis of the femoral neck | Femoral neck nonunion | Bone grafting, often combined with proximal femoral valgus osteotomy |
To reconstruct femoro-pelvic articulation | Destruction of the femoral head and neck | Greater trochanteric arthroplasty; pelvic support osteotomy; Ilizarov hip reconstruction (Choi Type IVB or failed type IVA); L’Episcopo, Albee, or Harmon operation, Ilizarov femoral neck lengthening, femoral neck reconstruction using vascularized bone grafting (Choi Type IVA) |
To equalize the lower limb length | Limb length shortening | Lengthening by distraction osteogenesis; contralateral epiphysiodesis or shortening of the femur; Ilizarov hip reconstruction |
To manage painful unstable hip as a last resort | Unstable hip with advanced osteoarthritis not amenable to the above-mentioned reconstructive procedures | Hip arthrodesis; total hip replacement arthroplasty; Ilizarov hip reconstruction after excision of the femoral head and neck remnant |
Table 31.2
Pearls and pitfalls in the management of late sequelae of infantile septic arthritis of the hip
Assessment | The surgeon should be familiar with radiological classifications of femoral residual deformities. Use of advanced imaging technologies (MRI, ultrasonography, arthrography, and 2-D/3D-CT) to visualize unossified cartilaginous structure of the epiphysis, also to determine osteocartilaginous geometry of the proximal femur, and the dynamics of articular motion between the deformed head and acetabulum. |
Full-length standing radiograph (teleradiograph) visualizing the entire lower limbs is helpful not only to identify associated sequelae at other sites, if any, but also to determine axial malalignment, joint malorientation, and limb length discrepancy. | |
Treatment | Femoroacetabular impingement-related symptoms are often encountered in older children and young adults with severe residual deformities. |
The decision to perform either reconstructive or salvage procedures must be made on an individual basis, after reviewing the clinical findings and imaging studies. Definitive and adjunctive surgical treatment methods can be used alone or in combination (see Table 31.1). | |
Author’s stepwise algorithmic surgical approach to femoroacetabular impingement would be helpful in decision making of treatment for Choi Type II and III hips (see Fig. 31.2). | |
Greater trochanteric arthroplasty for reconstruction of femoro-pelvic articulation is a technically demanding procedure with unpredictable outcomes. If performed at younger age, the transferred greater trochanter can assume a globular shape, but with no or incomplete formation of head-neck offset. | |
Ilizarov hip reconstruction is a highly effective treatment modality for the management of Choi Type IVB and IVA hips in which the previous reconstructive surgery has failed, or there is late presentation with a severe abductor lurch and a considerable limb length shortening, particularly in the adolescents and young adults in whom arthrodesis or hip arthroplasty is not suitable. |
Fig. 31.2
A schema showing the stepwise algorithmic approach to femoroacetabular impingement associated with Choi Type II and III sequelae, which are similar to Perthes(-like) deformities (see text). RFNL relative femoral neck lengthening, TFNL true femoral neck lengthening, PAO periacetabular osteotomy, PA posteroanterior, AP anteroposterior. Note: A triple innominate osteotomy is performed, instead of PAO, in (pre)adolescents with open triradiate cartilage [18]
Choi Type II and III Hips Causing Femoroacetabular Impingement and Secondary Hip Dysplasia
Type II and III hips are fundamentally the result of an abnormally shaped, sized, or oriented FH and neck, altered head-neck offset, and acetabular dysplasia. A wide variety of residual deformities of the FH have been observed in Type II and III hips, ranging from deformities similar to those in Perthes disease with coxa vara/valga, coxa plana, coxa breva, coxa magna, coxa irregularis, relative greater trochanteric overriding, sagging rope sign [15], and acetabular dysplasia to the more deformed proximal femur visualized as beard, collared, staghorn, or rugby ball-shaped FH [16, 17].
Children with Type II or III deformities may remain asymptomatic in their younger age, but, in (pre)adolescence, these children often present with clinical problems such as pain, limp, joint instability or contracture, restriction of motion, LLD, spinal disorders, and even emotional disturbances. According to the author’s experience, in older children with Type II and III hips, a painful limp is usually associated with femoroacetabular impingement (FAI) with or without damaged acetabular cartilage and/or labrum.
Figure 31.2 depicts a stepwise algorithmic approach to FAI in Perthes-like deformities at the author’s institute. First, the extent of asphericity is assessed; if it is mild and the FH is well contained within the acetabulum, osteochondroplasty of the head and neck junction alone is indicated. Next, the presence or absence of a labral tear is determined. If a labral tear is present, labral debridement or refixation is necessary. Similarly, the presence of coexisting acetabular dysplasia is assessed. If the hip becomes congruent in abduction, relative femoral neck lengthening combined with periacetabular osteotomy (PAO) or triple innominate osteotomy (TIO) is indicated. In the author’s institute, Bernese PAO is preferred for correction of acetabular dysplasia in adolescents and young adults with closed triradiate cartilage (around 12 years in girls and 14 years in boys) [18], whereas a TIO, in (pre)adolescents with open triradiate cartilage [19]. If the hip becomes congruent in adduction, proximal femoral valgus osteotomy and PAO or TIO are indicated. The next step is to check whether coxa breva and coxa vara associated with relatively greater trochanteric overriding are severe enough to cause FAI, and if so, a relative or true femoral neck lengthening combined with distal advancement of the greater trochanter (GT) is indicated [20–23]. When the FH asphericity is too severe and the FH is “irreducible,” the following procedures should be considered. If the hip becomes cong-ruent in extension and adduction, femoral valgus-flexion osteotomy plus/minus PAO or TIO should be considered. If the hip becomes congruent in any rotational position, rotational osteotomy with or without PAO or TIO may be indicated. If the FH with a central depression is too severely deformed such that the FH cannot be contained within the acetabulum in any position, Chiari osteotomy or FH reduction osteotomy [20, 21, 24] plus/minus PAO or TIO can be considered. In addition, combination of osteochondroplasty, labral debridement/refixation, and distal advancement of the greater trochanter should be performed, if necessary.
Late Treatment Options for Choi Type IV Deformity
The available reconstructive procedures for the treatment of Type IV hips are limited, and, in general, have not yielded satisfactory long-term results [1, 2, 7, 11, 25–29]. When only a remnant of the FH and neck is present, it is difficult to maintain a stable reduction; and if instability and dislocation persist, the surgeon can either leave the deformity uncorrected or can attempt reconstruction of femoro-pelvic articulation [25]. In young children in whom the FH and neck have been destroyed, as in Type IVA sequelae, a new femoral neck can be fashioned to articulate with the acetabulum by utilizing the L’Episcopo [30], Harmon [31], or Albee [32] reconstruction methods. When a reasonably sized unossified cartilaginous cap persists as a femoral neck remnant, open reduction can be attempted. The repositioning of the femoral remnant into the acetabular socket can be facilitated using a modification of the Harmon technique [31]. An incomplete, spring osteotomy is made at the base of the femoral remnant adjoining the greater trochanter and the resulting opening wedged gap is filled with a block of cartilage graft taken from the iliac apophysis. This procedure produces a femoral neck-lengthening effect [28]. In older children, gradual lengthening of the remnant femoral neck using the Ilizarov technique may be indicated. Nonetheless, the author believes that open reduction in children more than 6 years of age is not likely to be beneficial because of the high risk of developing stiffness and pain. Therefore, the author recommends that in children older than 6 years of age, Type IVA hips should be treated in the same manner as hips with Type IVB sequelae [2].
Postponing the treatment of Type IVB hips will result in proximal iliac dislocation with a marked abductor lurch, telescoping, limp, and LLD [8, 26]. Although these patients may remain asymptomatic for a number of years [3, 7, 12] they are at a risk of developing degenerative changes in the lumbosacral spine and hips [25]. Therefore, various treatment modalities for reconstructing a femoro-pelvic articulation in Type IVB hips have been reported: hip reconstruction with vascularized iliac crest grafting [33], arthrodesis, greater trochanteric arthroplasty (GTA) [25, 26, 34–39] with adjunctive or secondary procedures, pelvic support osteotomy (PSO) [40–44], and Ilizarov hip reconstruction (IHR) [44–58]. Of these treatment modalities, the two most commonly performed procedures are GTA and IHR.
Greater Trochanteric Arthroplasty Versus Pelvic Support Osteotomy (Ilizarov Hip Reconstruction)
GTA was originally described by Colonna [34] and was popularized by Westin [35] and others [25, 26, 36, 37]. The underlying concept of GTA is based on the following two aspects: firstly, the GT is viable and therefore retains its growth potential; and secondly, when the hyaline cartilage covering the GT is placed inside the acetabulum, the GT assumes a globular shape, similar to that of an FH [1, 2, 18, 26, 28, 29, 34–39, 44]. The detached abductor muscles must be transferred distally in order to provide hip stability and some degree of abductor function. However, the subsequent progressive subluxation observed in most of the patients necessitates additional procedures, such as femoral varus osteotomy, pelvic osteotomy including Chiari osteotomy, or shelf acetabuloplasty, to improve FH coverage. There are many drawbacks and limitations of GTA for reconstruction of femoro-pelvic articulation due to the uniqueness of the technique. Previous reports have described the potential risk of avascularity of the proximal segment after femoral varus osteotomy, difficulty in osteosynthesis at the varus osteotomy site, gradual straightening of the proximal femur due to remodeling at the osteotomy site, abductor weakness, stiffness, degenerative arthritis, and difficulty during conversion to total hip arthroplasty in adulthood [1, 2, 25, 26, 28, 36, 37, 51]. According to the author’s observation, the transferred GT can assume a globular shape with time, but with no or incomplete formation of head-neck offset. For this reason, even those children with satisfactory results at the midterm follow-up often present with FAI-related symptoms (Fig. 31.3).
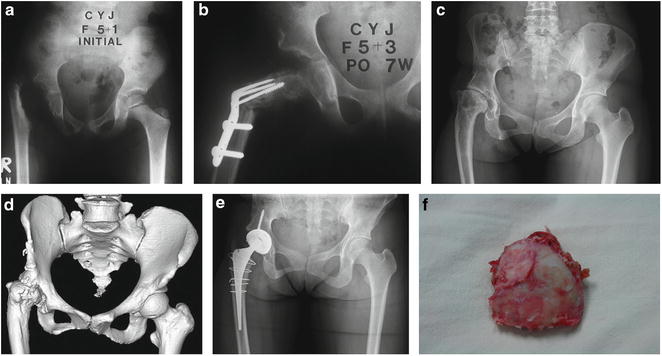
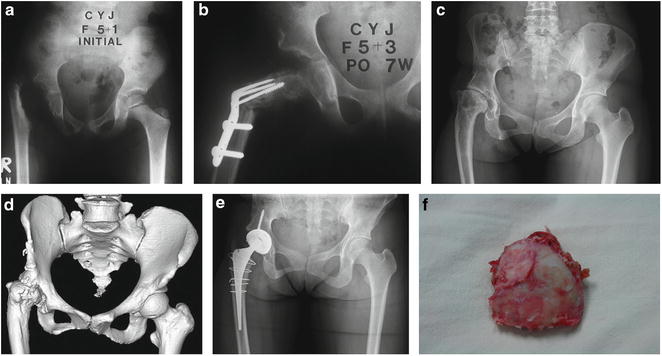
Fig. 31.3
Greater trochanteric arthroplasty in a girl. (a) A radiograph in a 5-year- and 1-month-old girl showing Choi Type IVB sequelae in the right hip. (b) A radiograph showing trochanteric arthroplasty with adjunctive femoral varus osteotomy. (c, d) Radiographs taken at 32 years of age showing advanced degenerative arthritis of the right hip joint, despite a well-remodeled greater trochanter which had assumed a globular shape similar to that of a femoral head. 3D-CT image also shows laterally displaced, remodeled greater trochanter with multiple osteochondral prominences on its margin, suggestive of femoroacetabular impingement. (e) A radiograph showing total hip replacement arthroplasty which was performed to treat a painful limp. (f) A gross photograph of the remodeled greater trochanter; the articular cartilaginous surface had been markedly degenerated, showing some fibrous adhesions
The two most important factors that determine the success or failure of a procedure after GTA are preoperative abductor weakness and stiffness [2]. Although some authors have reported satisfactory results [25, 26, 34, 35, 37–39], most of the experienced surgeons feel that GTA is a technically demanding procedure with highly unpredictable outcomes. The author has noted that the result of GTA may also be correlated with the patient’s age at operation. In a retrospective study performed by the author [28], satisfactory results were obtained only in those children who underwent GTA at less than 6 years of age. This observation may support the opinion that a patient should be old enough to follow the physical therapy instructions, and young enough to allow remodeling of the transferred GT [2].
“Pelvic support osteotomy (PSO)” has a long history in orthopedic surgery. The technique was developed in 1910s and quite popular until the advent of total hip arthroplasty [40–44]. The basic concepts and goals of PSO are to enhance femoro-pelvic stability by means of a proximal femoral valgus osteotomy and to improve hip biomechanics by displacing the center of gravity medially, resulting in an improvement in the mechanical efficiency of the abductor muscles [44]. However, the clinical application of traditional PSO is limited due to its indigenous shortcomings. It is difficult to achieve the optimal extent of angulation. If the angular correction is too large, excessive genu valgum, fixed pelvic obliquity, and impingement pain on adduction of the lower limb to neutral position may occur. On the other hand, if the angular correction is too small, the result would lead to an insufficient improvement in hip biomechanics, and most importantly, the issue of persisting LLD cannot be addressed. To overcome the shortcomings of traditional PSO, Ilizarov developed and popularized a modified PSO technique, the so-called IHR, in which a second distal femoral osteotomy is performed in addition to proximal femoral valgus osteotomy for pelvic support to realign the knee joint and to correct the LLD [44–58]. Furthermore, Ilizarov emphasized the importance of extension of the proximal femoral osteotomy to correct the fixed flexion deformity of the hip and to permit locking of the hip joint [44–47, 49–58].
Evidence has accumulated that IHR is highly effective in eliminating or substantially reducing the Trendelenburg gait and in equalizing the lower limb length while improving the stability and range of motion of the hip joint at the same time [44, 47–58]. Hence, the author currently prefers IHR for the management of Type IVB and IVA hips in which the previous reconstructive surgery has failed, or there is late presentation with a severe abductor lurch and a considerable LLD, particularly in the adolescents and young adults in whom arthrodesis or hip arthroplasty is not suitable [44].
The reported complications of IHR in the literature include knee stiffness, pin tract infection, delayed consolidation, refracture, obturator nerve entrapment, straightening of proximal valgus angulation, and persistent Trendelenburg gait. There exists a possibility of ischiofemoral impingement if the apex of the proximal femoral valgus angulation site directly abuts the ischium. The literature demonstrates that an average of 30 % (range, 0–62.5 %) of patients have a persistent positive Trendelenburg sign after IHR, although it is reduced in severity in most of the patients [44].
IHR is not ideal for young children, because in accordance with Wolff’s law, gradual straightening of the proximal femur tends to occur at the site of valgus angulation, which may result in loss of pelvic support. Bone remodeling and subsequent gradual loss of valgus angulation remain important considerations in proximal femoral osteotomy [44, 46, 51, 52, 55, 56, 58] (Fig. 31.4). Therefore, when performing IHR at an age before adolescence, as much as 25°–40° of overcorrection should be empirically added to the valgus correction angle based on the single-leg stance drop angle relative to the horizontal line of the pelvis due to the possibility of straightening of the proximal femur after IHR [44, 46, 51]. The author believes that IHR is still indicated even if patients are older than 6 years of age, despite the high probability of repeat PSO, because a second femoral lengthening is usually needed at or near skeletal maturity in patients with hip instability associated with marked LLD due to multiple lower limb growth disturbances secondary to neonatal sepsis. Another alternative is to perform femoral lengthening without a PSO, and insert half pins into the pelvis to prevent proximal migration of the femur at a younger age, and subsequently perform IHR when the patients are near skeletal maturity [44, 55].
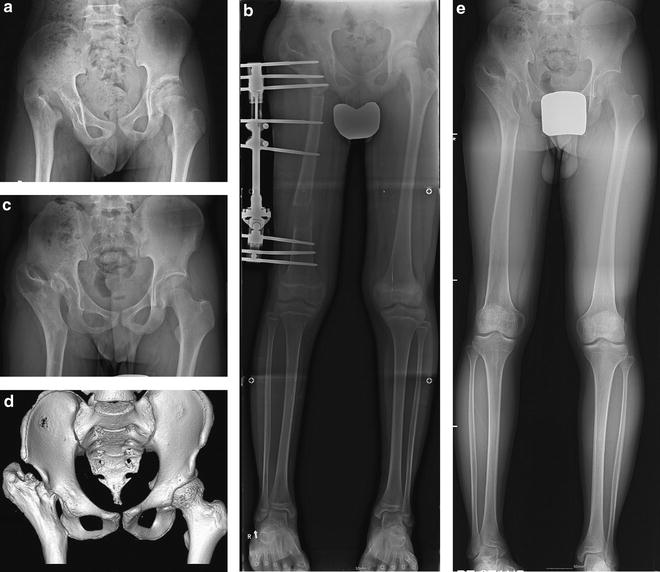
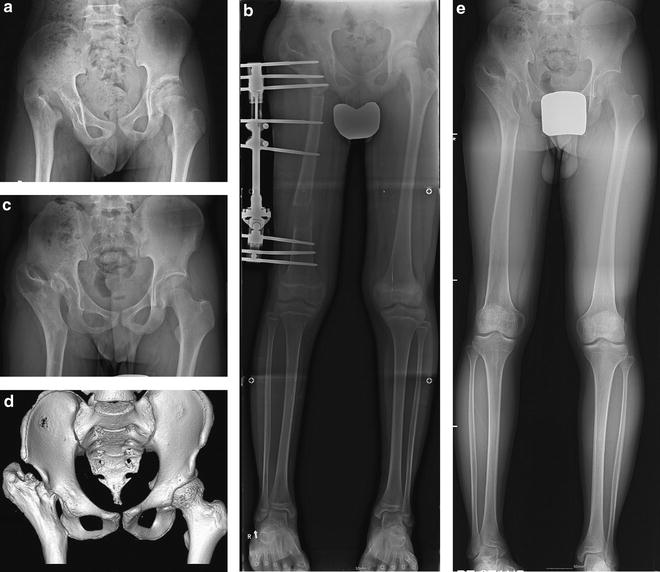
Fig. 31.4
(a) A radiograph in a 12-year- and 4-month-old boy with Choi Type IVB sequelae in the right hip. He had a previous history of Ilizarov hip reconstruction with 40° of proximal valgus osteotomy for pelvic support and 4 cm of distal diaphyseal lengthening for leg length equalization performed at an age of 8 years and 1 month. It is noteworthy to observe a completely remodeled, straightened proximal femur showing no evidence of pelvic support. (b) A teleradiograph showing a repeated Ilizarov hip reconstruction osteotomy. (c, d) A plain radiograph and 3D-CT taken at 17 years of age showing displacement of the lesser trochanter into the acetabulum and proximal femur with valgus angulation near the ischium, which apparently enhances the femoro-pelvic stability and improves abductor mechanics by displacing the center of gravity medially. (e) A teleradiograph taken at 17 years of age showing equalization of the lower limb length after surgery. He had a negative Trendelenburg sign
Late Sequelae After Septic Arthritis and Osteomyelitis Around the Knee and Ankle Joints
The rate of overall unsatisfactory results in terms of residual deformities after infantile or childhood septic arthritis of the knee and ankle joints is less as compared to that after septic arthritis of the hip [5, 6], because the infection in these joints can be diagnosed sooner than that in the hip [9]. Long-term assessment is essential because radiographic improvement in the involved epiphyseal region can occur several months to years after the infection. In younger children in whom the secondary ossification center has not yet developed, vascular damage can lead to a marked delay in the formation of the ossific center, but the cartilage model continues to grow. Therefore, even when bone deficiency is seen on plain radiography, it is necessary to perform advanced imaging studies such as ultrasonography, arthrography, or MR imaging [9] in order to better visualize the cartilaginous epiphysis (chondroepiphysis) and assess the potential growth of the adjacent physis. When the appropriate treatment is delayed, growth disturbance with a resultant angular deformity, joint incongruity, impingement, and accompanying ligamentous laxity and joint instability may develop gradually. Postinfectious juxta-articular deformity of the knee usually develops as a result of metaphyseal osteomyelitis or primary septic arthritis of the knee, involving the distal femoral physis or the proximal tibial physis, or both. The distal femur is more prone to growth-related sequelae than the proximal tibia. Angular deformities due to partial distal femoral physeal destruction are far more common than complete symmetric growth cessation [9]. The most serious growth sequelae occur following neonatal sepsis and to a lesser extent within the first 2 years of life [6, 9] (Fig. 31.5). In particular, meningococcemia caused by Neisseria meningitides or meningococcus, which is found only in human respiratory secretions, is a devastating illness that primarily affects young children. The disseminated intravascular coagulation and focal infections of the acute phase are primarily responsible for the vascular injuries to the growing chondro-osseous tissues and contiguous soft tissues. Ischemic changes also selectively involve the physeal circulation, which adversely affect longitudinal and transverse growth of bone. Therefore, children who survive meningococcal septicemia are prone to develop complex deformities of the lower limb due to multiple areas of growth disturbance [59–61].
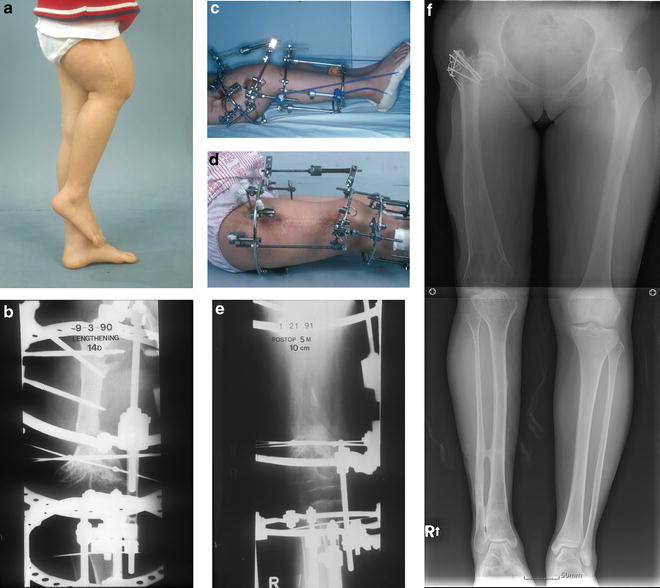
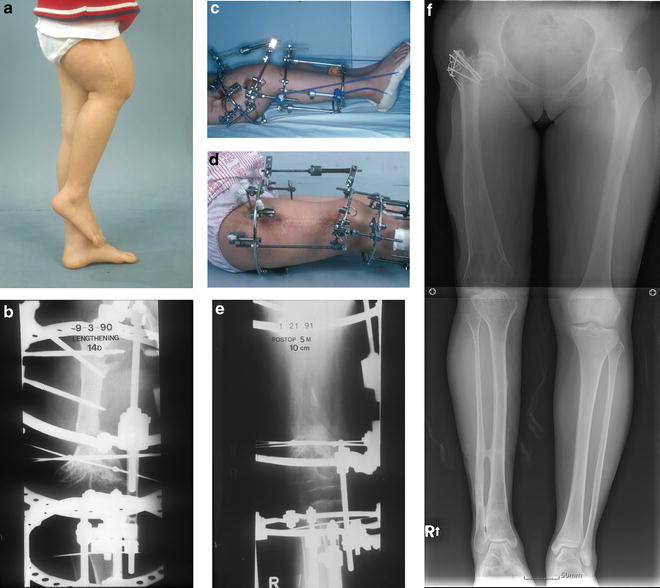
Fig. 31.5




(a) A 10-year- and 7-month-old girl presenting with 17.5 cm of shortening of the right femur and a concomitant 30° of flexion contracture of the knee joint after fulminant osteomyelitis of the right femur extending to the hip and knee joints. Further flexion in the knee joint was only marginally limited. (b, c) A radiograph and photograph showing the femoral and tibial Ilizarov frames constructed with one proximal full ring and a distal two-third ring for concomitant femoral lengthening and deformity correction at the distal femoral corticotomy site. Tibial frame was applied for the purpose of transarticular fixation during lengthening to prevent potential subluxation of the unstable knee joint apparently caused by deformation of the femoral condyle secondary to central physeal arrest in the distal femur. (d, e) A concomitant 10-cm lengthening and deformity correction could be achieved by differential distraction of the anterior and posterior motor rods. Subsequent procedures included right tibial and fibular lengthening followed by left distal femoral epiphysiodesis, concomitant right femoral and tibial lengthening, and right greater trochanteric advancement. (f) At the last follow-up at the age of 26 years, her right lower limb function and gait were excellent with equalization of the lower limb length and no knee flexion contracture despite the difference in the knee level
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


