Fig. 70.1
a Micturating cystourethrogram showing dilated bladder with no vesicoureteric reflux. Note the dilated posterior urethra indicative of posterior urethral valve. b micturating cystourethrogram showing a dilated posterior urethra indicative of posterior urethral valve
Fig. 70.2
a and b Micturating cystourethrogram showing dilated posterior urethra indicative of posterior urethral valve. Note the marked right sided and left sided vesicoureteric reflux
Visualization of the valve leaflets
A thickened trabeculated urinary bladder
A dilated or elongated posterior urethra
A hypertrophied bladder neck
The presence of diverticula, vesicoureteral reflux, and reflux into the ejaculatory ducts
Very thickened hypertrophied urinary bladder wall which may lead to secondary ureterovesical junction obstruction
Renal scintigraphy
Tc-dimercaptosuccinic acid (DMSA) and mercaptoacetyltriglycine (MAG-3) renal scintigraphy provide information about relative renal function and areas of scarring or dysplasia.
MAG-3 renal scan with furosemide (Lasix) also provides information about renal drainage and possible obstruction.
Urodynamic evaluation:
Provides information about bladder storage and emptying.
The term “valve bladder” is used to describe patients with PUV and a fibrotic noncompliant bladder.
These patients are at risk of developing hydroureteronephrosis, progressive renal deterioration, recurrent infections, and urinary incontinence.
Patients with PUV require periodic urodynamic evaluation throughout childhood because bladder compliance may further deteriorate over time.
Cystoscopy: serves both diagnostic and therapeutic functions.
Diagnostic cystoscopy:
◦ Confirm the diagnosis
Therapeutic cystoscopy:
◦ Transurethral incision of the PUV.
◦ Multiple techniques have been described for ablating the valves.
◦ Currently, valves are disrupted under direct vision by cystoscopy using an endoscopic loop, Bugbee electro cauterization, or laser fulguration.
◦ In extremely small infants (< 2000 g), a 2F Fogarty catheter may be passed either under fluoroscopic or under direct vision for valve disruption.
◦ In some patients, the urethra may be too small and a temporary vesicostomy is performed.
Secondary effects of PUV:
Vesicoureteral reflux (Fig. 70.3)
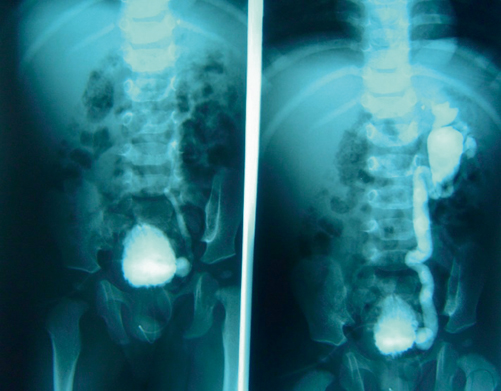
Fig. 70.3
Micturating cystourethrogram showing vesicoureteric reflux (left), which is severe in the second picture (right)
Vesicoureteral reflux is commonly associated with PUV and is present in as many as one third of patients .
When associated with PUV, reflux is generally secondary to elevated intravesical pressures.
The treatment of vesicoureteral reflux in patients with PUV involves treatment of intravesical pressures using :
1.
Anticholinergics
2.
Timed voiding
3.
Double voiding
4.
Intermittent catheterization
5.
Bladder augmentation
UTIs
Recurrent UTIs are common in patients with PUV. These are secondary to :
1.
Elevated intravesical pressures
2.
Increased post void residual urine volumes, leading to stasis of urine.
3.
Dilated upper urinary tracts, with or without vesicoureteral reflux.
UTI management is directed at:
1.
Lowering bladder pressures (anticholinergic medication)
2.
Lowering post void residual urine volume (via clean intermittent catheterization)
3.
Administering prophylactic antibiotics
Urinary incontinence
The same factors that lead to vesicoureteral reflux and UTI also lead to urinary incontinence .
Correct management of bladder function depends on adequate bladder evaluation with urodynamic studies.
These include:
1.
Lowering bladder pressure.
2.
Improving bladder compliance.
3.
Minimizing post void residual urine volume.
4.
In some, bladder augmentation may be needed .
Pathophysiology
An interesting group of patients are those with vesicoureteral reflux and renal dysplasia (VURD) syndrome .
Get Clinical Tree app for offline access
In these patients, one kidney is hydronephrotic, nonfunctioning, and has high-grade vesicoureteral reflux .
The high-grade reflux is thought to act as a pop-off valve (Fig. 70.4), leading to reduced overall bladder pressures and preservation of contralateral renal function.
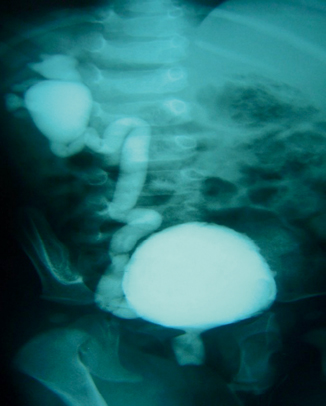
Fig. 70.4
Micturating cystourethrogram showing posterior urethral valve and marked reflux on the right side. There is marked hydronephrosis which act as a pop-off valve
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


