Fig. 59.1
a Clinical photograph in a patient with abdominal neuroblastoma. Note the mass crossing the midline. b Abdominal CT scan showing a large abdominal neuroblastoma crossing the midline
As a result, most children present with abdominal symptoms, such as fullness or distension. Typically, children with localized disease are asymptomatic, whereas those with disseminated neuroblastoma are generally sick and may have systemic manifestations, including weight loss, anorexia, and failure to thrive, fever, irritability, and bone pain.
The most common finding in those with abdominal neuroblastoma is a nontender, firm, irregular abdominal mass that crosses the midline (Fig. 59.2).

Fig. 59.2
Clinical photographs showing a patient with neuroblastoma and ecchymosis around the eyes (a) and a patient with neuroblastoma with metastasis to the retrobulbar area (b)
Most neuroblastomas produce catecholamines which result in interesting presentations in children with neuroblastoma .
Kerner–Morrison syndrome is caused by vasoactive intestinal peptide (VIP) tumor secretion and is more commonly associated with ganglioneuroblastoma or ganglioneuroma. It causes intractable secretory diarrhea, resulting in hypovolemia, hypokalemia, and prostration. This syndrome typically resolves following the complete removal of the tumor .
William Pepper in 1901 described a localized primary tumor and metastatic disease limited to the skin, liver, and bone marrow in infants. Pepper syndrome has since been associated with stage 4S neuroblastoma, a unique entity that occurs only in infants younger than 1 year. Pepper syndrome generally is associated with spontaneous regression. Some infants with stage 4S neuroblastoma, however, die of massive hepatomegaly, respiratory failure, and overwhelming sepsis.
“Blueberry muffin” babies are infants in whom neuroblastoma has metastasized to subcutaneous sites. When provoked, the nodules become intensely red and subsequently blanch for several minutes thereafter. The response is probably secondary to the release of vasoconstrictive metabolic tumor by-products.
Hutchinson syndrome results in bone pain with consequent limping and pathologic fractures. It results from widespread metastasis of neuroblastoma to the bones.
Neuroblastomas that arise in the paraspinal ganglia may invade through the neural foramina, compress the spinal cord, and subsequently cause paralysis.
Infrequently, neuroblastoma can become metastatic to the retrobulbar region, leading to rapidly progressive, unilateral, painless proptosis, periorbital edema, and ecchymosis of the upper lid (“raccoon eyes”) (Fig. 59.2) .
Investigations and Diagnosis
Abdominal x-ray most commonly reveals a soft-tissue density and finely stippled calcifications (Fig. 59.3) .

Fig. 59.3
Abdominal x-ray showing a large soft-tissue density occupying most of the abdomen
Chest x-ray may show a soft-tissue density with fine calcification in the posterior mediastinum in cases of thoracic neuroblastoma (Fig. 59.4).
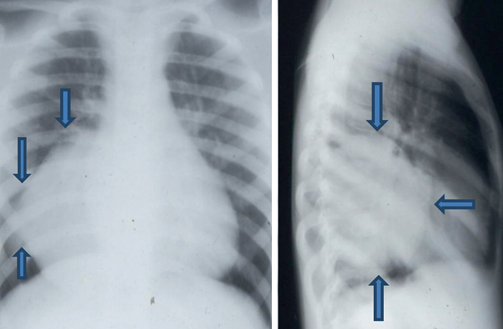
Fig. 59.4
Chest x-ray showing a soft-tissue mass in the posterior mediastinum in a patient with thoracic ganglioneuroma
Abdominal ultrasound is more informative regarding the site, consistency, and size of the mass.
Abdominal and thoracic CT scan or MRI (for paraspinal tumors) provides more information about the mass, regional lymph nodes, invasion, and distant metastasis (Fig. 59.5).
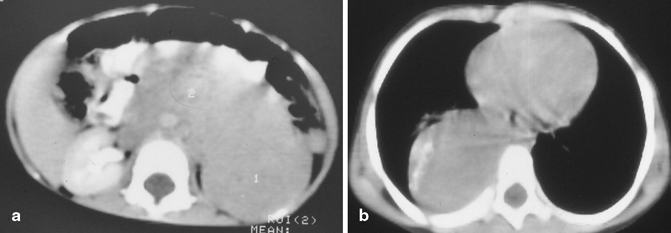
Fig. 59.5
a Abdominal CT scan showing a large abdominal mass arising from the left adrenal gland and crossing the midline. b Thoracic CT scan showing a ganglioneuroma in the posterior mediastinum. Note the presence of calcification in the mass
Bone scan and a skeletal survey detect cortical bone disease.
Another way to detect neuroblastoma is the meta-iodobenzylguanidine (MIBG) scan, which is taken up by 90–95 % of neuroblastomas, often termed “mIBG-avid.” MIBG scan which is a labeled isotope derivative of norepinephrine is quite sensitive and specific in the detection of metastasis to bones and soft tissue. MIBG is recommended for reassessment both during and after treatment of neuroblastoma.
Recently, positron emission tomography (PET) scan has been used for the detection of non-MIBG avid disease and for follow-up of high risk cases .
Ninety percent of neuroblastomas secrete elevated levels of catecholamines and their metabolites which include dopamine, homovanillic acid (HVA), and/or vanillylmandelic acid (VMA). These are found in the urine or blood .
This fact becomes clinically relevant because children with undifferentiated tumors excrete higher levels of HVA than VMA. This occurs because undifferentiated tumors have lost the final enzymatic pathway that converts HVA to VMA. A low VMA-to-HVA ratio is consistent with a poorly differentiated tumor and indicative of a poor prognosis. HVA and VMA levels measured prior to treatment serve as markers and if elevated after the treatment indicates persistent disease or recurrence.
Elevated levels of neuron-specific enolase (NSE), lactic dehydrogenase (LDH > 1000), and ferritin (> 150) are markers useful in the diagnosis of neuroblastoma as well as the prognosis.
Approximately 96 % of patients with metastatic neuroblastomas have an elevated NSE level, which has been associated with a poor prognosis.
Specific requirements to stage neuroblastoma include :
1.
Bilateral bone marrow aspirates and biopsy
2.
Abdominal and chest CT scan
3.
Bone scan
4.
MIBG scan
Recently, an international committee on neuroblastoma staging recommended obtaining two bone marrow aspirates and two biopsies, one from each posterior iliac crest .
According to the International Neuroblastoma Staging System (INSS), the diagnosis of neuroblastoma is based on either:
1.
Characteristic histopathologic findings of neuroblastoma
2.
The presence of neuroblastoma cells in a bone marrow aspirate or biopsy sample
3.
Elevated levels of urinary catecholamine metabolic by-products
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


