Polycythemia
INTRODUCTION
The normal hematocrit of a healthy term infant ranges from 45% to 61%. This relatively high red cell mass is an adaptive response to the hypoxic intrauterine environment. Neonatal polycythemia, an abnormal elevation of red cell mass, is most often defined in textbooks as a venous hematocrit of 65% or more. It occurs in 1.5%–4% of healthy live births.1 Passive erythrocyte transfusion and increased fetal red cell production are 2 major causes for neonatal polycythemia.
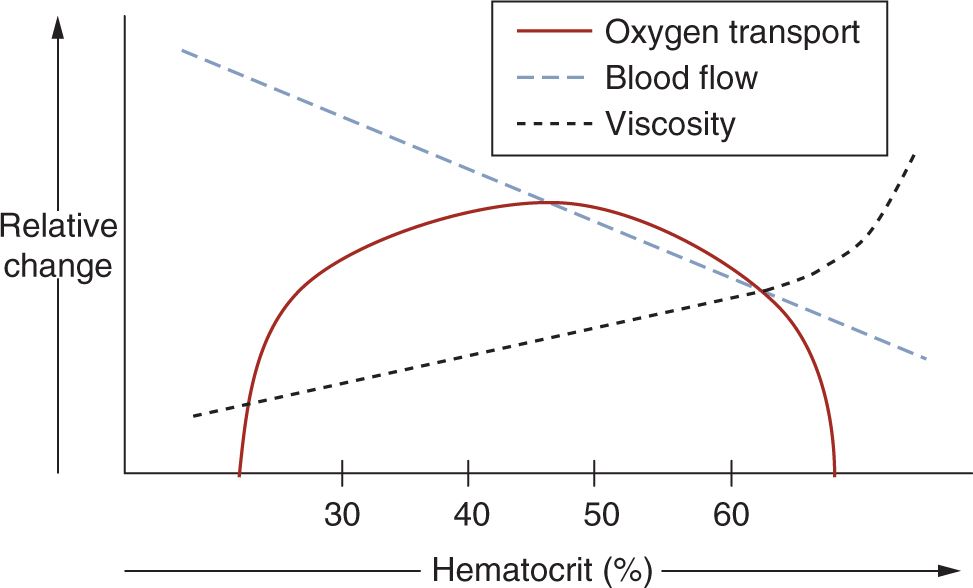
Many patients are asymptomatic. When present, signs and symptoms are presumed to be secondary to associated hyperviscosity. Although not all polycythemic blood is hyperviscous, there is an exponential increase in blood viscosity when the hematocrit is 65% or higher, with a correlative decrease in oxygen transport (Figure 93-1). Poor oxygenation and microthrombi formation are believed to result in organ dysfunction in polycythemia. The central nervous, cardiopulmonary, endocrine, and gastrointestinal systems are commonly affected. Treatment of symptomatic polycythemia is partial exchange transfusion (XT). However, criteria for and benefit from this treatment are controversial.
FIGURE 93-1 Effect of hematocrit on blood flow, viscosity, and oxygen transport. (Adapted with permission from Glader.2)
DIAGNOSIS AND INDICATION
Clinical Findings: History and Physical
Causes of polycythemia in neonates can be divided into 2 major categories: passive red blood cell (RBC) transfusion and increased erythropoiesis secondary to intrauterine hypoxia. During delivery, passive placental RBC transfusion can occur from delayed cord clamping or if the infant is held below the level of the introitus. Perinatal asphyxia and maternal oxytocin administration have also been known to increase placental RBC transfer to the fetus.3 In monochorionic twin pregnancies, twin-twin transfusion results in polycythemia in the recipient, who most commonly is the larger infant.
Increased erythropoiesis can occur in response to intrauterine hypoxia, and result in neonatal polycythemia. This is seen in pregnancies with placental insufficiency, which can result from multiple etiologies (Table 93-1). Increased erythropoiesis is also seen in pregnancies with increased fetal oxygen consumption, including congenital thyrotoxicosis and maternal diabetes.3
Table 93-1 Factors and Conditions Associated With Neonatal Polycythemia
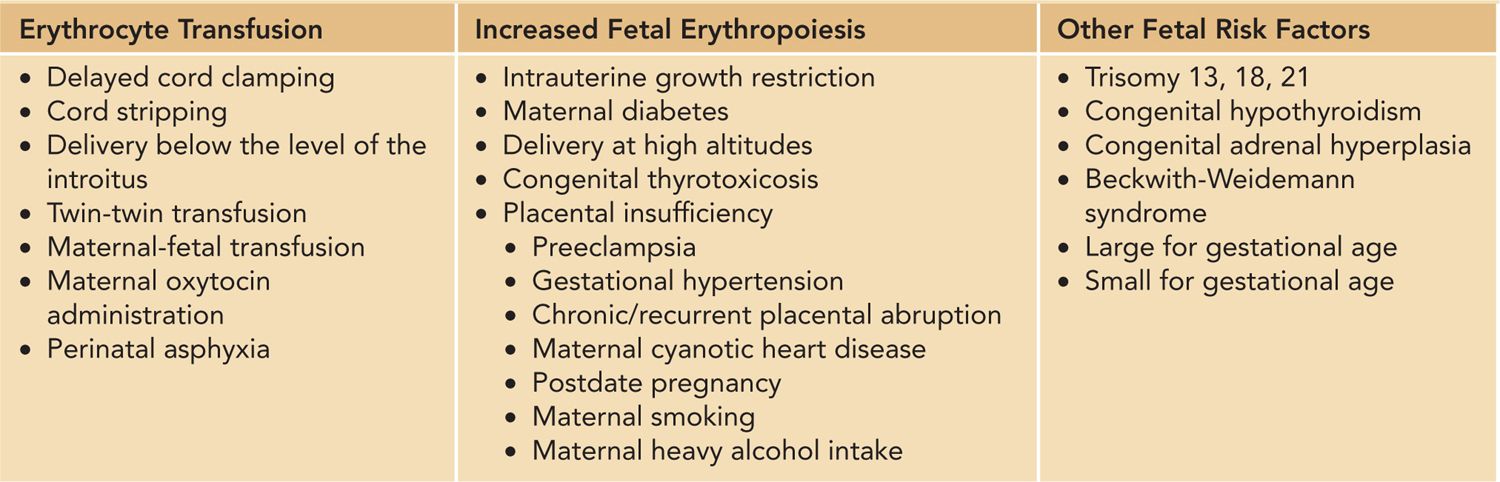
Polycythemia has been observed in neonates with trisomy 13, 18, and 21, as well as in those with Beckwith-Weidemann syndrome. The cause of polycythemia in patients with these genetic disorders is not known. Infants who are large or small for gestational age are also at risk. A comprehensive list of factors is outlined in Table 93-1.
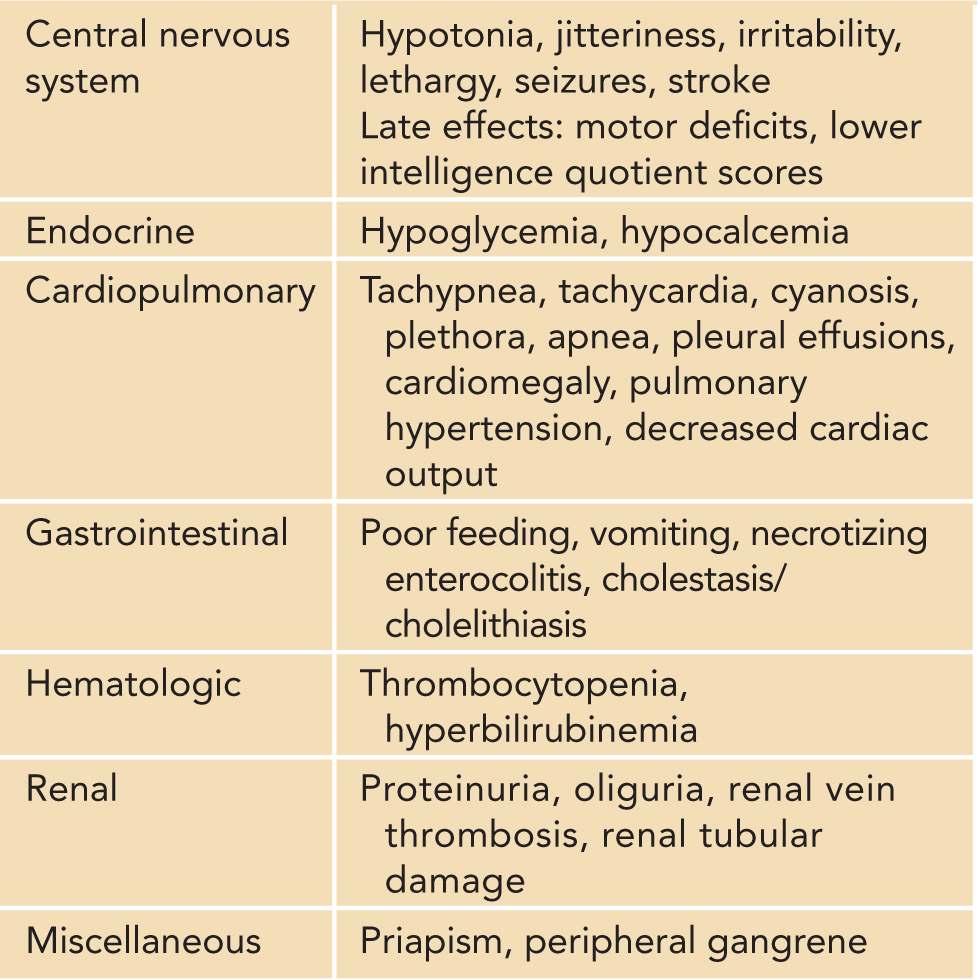
The American Academy of Pediatrics (AAP) does not recommend routine screening for polycythemia.4 However, screening should be done in neonates who are at risk or have clinical signs suspicious for polycythemia. Common early signs include plethora, jitteriness, and poor feeding. Tachypnea, abdominal distention, irritability, and lethargy are also common. Hypoglycemia and hypocalcemia are frequently observed endocrine abnormalities, with up to 40% of patients having hypoglycemia. Associated hematologic complications include hyperbilirubinemia and thrombocytopenia. Neonates with polycythemia may also have significantly decreased gastrointestinal blood flow, which places them at risk for necrotizing enterocolitis (NEC). Renal vein thrombosis, proteinuria, and priapism are other rarer symptoms. A more comprehensive list of clinical features is outlined in Table 93-2. It is important to note that these signs and symptoms are not specific for polycythemia, and when present, other causes for these abnormalities should also be investigated.
Table 93-2 Clinical Features Associated With Polycythemia and Hyperviscosity
Baseline and Confirmatory Tests
To accurately diagnose polycythemia, there are 3 major areas that require attention: site of blood draw, timing of draw, and mode of analysis. Capillary blood flow can have significant variability and result in up to 15% higher hemoglobin and hematocrit values compared to venous samples.1 Therefore, a capillary hematocrit of 65% or greater needs to be confirmed with a venous sample.
The timing of blood draws needs to be noted as hematocrit values peak 2 hours postpartum, at which time values up to 71% may be considered normal.5 This initial increase in hematocrit is related to movement of fluid from the intravascular to the extravascular space. After this point, values begin to decrease in response to higher extrauterine ambient oxygen concentrations. Therefore, screening is best done after 6 to 8 hours of life if performed in an asymptomatic infant.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree