FIGURE 11-1 A: Clinical photograph of pouce flottant. B: Radiograph of same patient without proximal metacarpal, no CMC joint. This was treated with a pollicization.
CLINICAL QUESTIONS
- What systemic conditions are associated with a hypoplastic thumb?
- How are hypoplastic thumbs classified?
- Which thumbs are best treated with amputation and index finger pollicization?
- How does pollicization compare to microvascular reconstruction in a Blauth type IIIB thumb?
Prehension distinguishes human hand function. Sophisticated pinch develops as children progress from rake grasp to rudimentary pinch to tip-to-tip pinch over the course of the first 1 to 2 years of life. Strong thumb intrinsic and extrinsic muscles, along with joint stability and mobility, are vital for normal pinch function.
A hand with a congenital thumb aplasia or a pouce flottant (floating thumb) (Figure 11-1) will be permanently devoid of tip-to-tip pinch function without operative intervention. A pollicization of the index finger is still the procedure of choice for these hands. However, the expected outcomes for a floating thumb with mild radial dysplasia and a near-normal index finger (Figure 11-2) are much better than a floating thumb with marked radial dysplasia and limited index finger function (Figure 11-3).
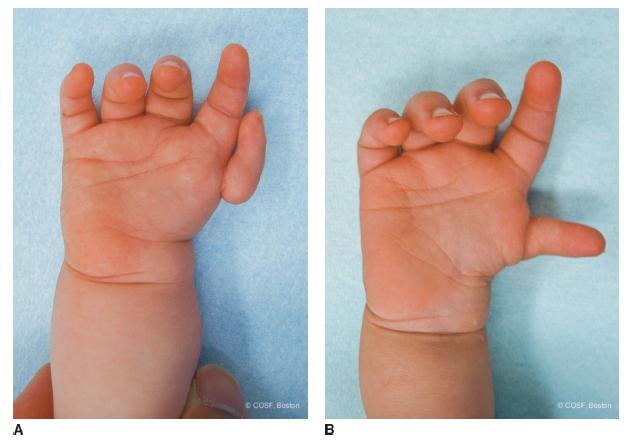
FIGURE 11-2 A: More defined type IIIB. B: This pouce flottant represents even more complex decision making for the parents of this child with another type IIIB. These thumbs make it very difficult for parents to accept amputation and pollicization rather than reconstruction.

FIGURE 11-3 Severe radial longitudinal deficiency (type IV) with pouce flottant. Pollicization results will have a more limited outcome due to stiffness (note no skin creases at IP joints) and muscle limitations of index finger.
A hypoplastic thumb without a proximal metacarpal and carpometacarpal (CMC) joint (Blauth type IIIB) similarly will never develop prehension with that thumb without surgery. There are societal and surgical differences of opinion about whether the best treatment for function and appearance is (1) amputation of the hypoplastic thumb and index finger pollicization or (2) microvascular metatarsal-phalangeal joint transfer for CMC joint reconstruction with tendon transfers.1–7
Etiology and Epidemiology
The specifics are discussed in more detail in the thumb hypoplasia and radial longitudinal deficiency chapters (see Chapters 10 and 13). Suffice it to say, any thumb deficiency can be associated with malformations or deficiencies of other organ systems. In particular, vertebral, anal, cardiac, tracheoesophageal, renal, lower limb (VACTERRL), and hematopoietic abnormalities are common. Specific syndromes include Holt-Oram (autosomal dominant cardiac septal defects and radial deficiency), TAR (autosomal recessive thrombocytopenia absent radius), and Fanconi anemia (FA) (autosomal recessive bone marrow failure).
Clinical Evaluation
It is imperative that a thorough evaluation of the cardiac, renal, musculoskeletal, hematopoietic, and gastrointestinal organ systems occurs before care for the hand begins. Clearance of each system by physical exam and additional testing is done in conjunction with primary care pediatrics and multiple medical and surgical subspecialists. Of note, early diagnosis of a FA is one of the rare situations in which a hand surgeon can truly save a life (see Sidebar).
In terms of hand and arm evaluation, simply, the quality of the index finger determines the quality of the pollicization. The presence of index finger metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) skin creases with easy, full passive motion of those joints is reassuring that the index finger is well developed (Figure 11-2). Thin, shiny skin without creases is a grave concern about future function (Figure 11-3). Similarly, the more radial deficiency, the less likely there is adequate musculature and joint mobility to provide desired pinch postoperatively. It is clear that outcomes from simple thumb aplasia without radial deficiency are far superior to pollicization in the presence of marked radial club hand. Therefore, a thorough clinical and radiographic assessment is critical in realistic planning and discussions with parents and families. They will not be able to discriminate their child’s situation from others they have read about or discussed with other families. You can, and you must, in your exam of the child, engage parents in discussions and surgical decision making.
Fanconi Testing and Bone Marrow Transplantation
FA is a rare, autosomal recessive genetic disorder (rarely X-linked recessive) with an incidence of about 1:350,000 live births. The incidence is much higher in the Ashkenazi Jewish population. The genetic deficiency is in core proteins (FANCA) responsible for DNA repair. Eight of these FANCA proteins assemble in the nucleus when DNA failure occurs. Failure of these proteins to effectively repair DNA accounts for the high risk of cancer, especially acute myelogenous leukemia, and/or progressive bone marrow failure in untreated patients with FA. These children can have associated congenital differences with hearing loss, short stature, and renal abnormalities, among others. At present, any infant, especially those without typical phenotypic features of FA, with radial longitudinal deficiency should have a chromosomal fragility challenge test (with mitomycin C or diepoxybutane [cross-linking agents]). Early identification of FA allows for HLA-type testing of family members looking for an identical match for hematopoietic stem cell transplantation. If no matches exist, genetic counseling can assist the family in deciding about a savior sibling with preimplantation genetic diagnosis. Early survival rate after identical HLA matching bone marrow transplantation can be as high as 90% and significantly exceeds transplantation from unrelated donors. Bone marrow stem cell transplantation has the best results in the first decade of life and before any bone marrow failure begins. Macrocytosis and nonmegaloblastic anemia occur at an average age of 7 years. Thus, early identification of FA and genetic counseling are critical to survival rates with bone marrow transplantation. The pediatric hand surgeon needs to be very knowledgeable about FA and well connected with skilled genetic counseling and care to help save or prolong a life.
Surgical Indications
About the only thing that comes to us without effort is old age
—Gloria Pitzer
The indications for pollicization include (1) absent thumb, (2) floating thumb, (3) hypoplastic thumb without a CMC joint, and (4) a well-developed, mobile index finger to become a high-quality thumb. Parental, social, religious, and personal considerations are major factors. Central nervous system integration is important, but, so far, no one has determined an IQ level required for pollicization.
A teacher is one who makes himself progressively unnecessary.
—Thomas Carruthers
Pollicization is an operation for the experienced and dedicated pediatric hand and upper limb surgeon. There are many different techniques of pollicization outlined in the peer review and textbook literature.8–12 Mostly they differ on skin flap design and rotation. However, the underlying anatomic principles are the same. In order for an index finger to become a functional and cosmetic thumb, you need (1) more skin for a first web space that is deeper and more mobile than the second web space; (2) less bone for a biphalangeal thumb rather than a triphalangeal index finger; (3) more thenar abduction and opposition power; (4) a new CMC joint in the proper orientation for tip prehension to the middle finger, the new index so to speak; and (5) survival of the pollex, all skin flaps, and adequate mobility and strength for functional use. You can use the flap design of your choice. You cannot violate the principles and be successful (see Figure 11-6).
Specific unique anatomic features of a well-developed, mobile index finger that allow it to work as a pollex are (1) two extensor muscles and tendons, extensor indicis proprius (EIP) and extensor digitorum communis (EDC) that can be used to provide both extrinsic extensor and abductor function, (2) a strong first dorsal interosseous that can provide adequate thenar intrinsic muscle function, (3) a distal metacarpal epiphysis that can be converted into a thumb carpal bone, and (4) abundant dorsal skin that can be rotated into the first web space when the index metacarpal is excised.
Pollicization, like most operations, is a series of technical steps. Like many congenital hand operations, the flap design and incision outline with a marking pen is one of the most critical steps. As mentioned, there are many published and unpublished flap designs. We follow a series of modifications from the Buck-Gramcko pollicization technique that Lister modified and then Waters modified further (Figure 11-4).
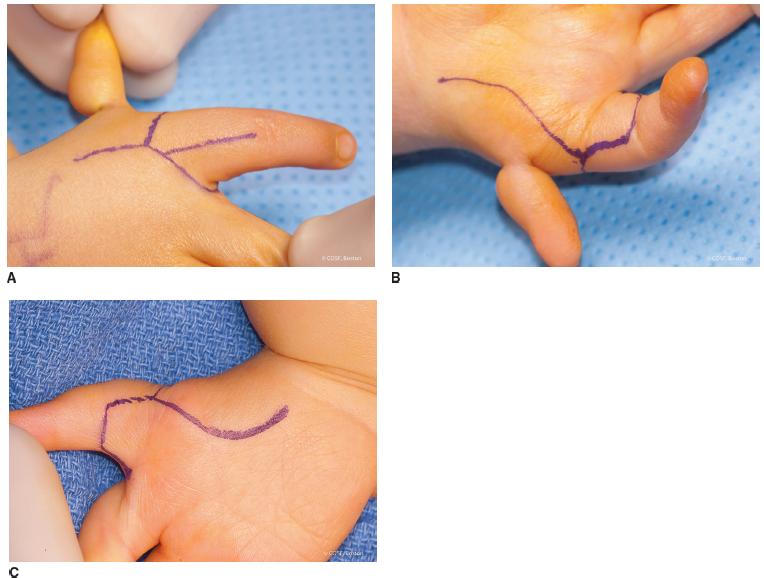
FIGURE 11-4 A: Dorsal skin incision. B, C: Volar and radial skin incisions with floating thumb. C: Dorsal and radial skin incision without floating thumb.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


