Poisonous Bites and Stings
Dee Hodge, III and Carl R. Baum
Although a large proportion of the morbidity and mortality from bites and stings occurs in the pediatric age group, there are surprisingly few studies dealing with their diagnosis and treatment in children. As with other injuries, the immediate care of a child suspected of having suffered from an animal bite or sting should start with a rapid evaluation of vital signs, followed by a more detailed assessment of the local signs, including the size and appearance of fang or sting marks, pain, swelling, and color of surrounding skin. Any further investigation of the source of the injury should not result in overlooking the administration of tetanus prophylaxis when appropriate, or in delaying symptomatic treatment of pain and itching. Frequently, a period of observation is necessary to define the seriousness of the injury, particularly when it is not clear whether the causing animal is venomous.
AQUATIC STINGS
A large number of venomous marine animals cause mild, debilitating, or even fatal envenomation. These are seen most frequently in tropical or temperate waters of North America and the Indo-Pacific region. Because of the marked increase in recreational water sports, especially diving, exposure to marine-animal envenomation has become more frequent.
PHYLUM COELENTERATA (CNIDARIA)
Members of this group are divided into three large classes: the Hydrozoa (hydras, Portuguese man-of-war), Scyphozoa (true jellyfish), and Anthozoa (soft corals, stone corals, and anemones). All of these animals are present in temperate, subtropical, and tropical environments. All members of the phylum have specialized organelles called nematocysts (ie, cnidae) that are used for entrapping and poisoning prey. When the tentacles touch a victim, the nematocysts discharge toxin on or through barbed threads. The severity of envenomation is related to the toxicity of the specie’s venom, number of nematocysts discharged, general condition of the victim, and whether prior sensitization exists. Mild to severe local and/or systemic reactions may ensue. Stings from sessile species are, in general, not as severe as stings from free-floating forms. Paralysis and central nervous system (CNS) dysfunction appear to be caused by specific toxic peptides contained in the venom. Burning pain and urticaria are secondary to the presence of serotonin, histamine, and hista-mine-releasing agents.
The hydrozoans include the feathered hydroid (Pennaria tiarelia) and the Portuguese man-of-war (Physalia physalis). The mild sting of the feathered hydroid occurs with handling and may be treated with local care. The Portuguese man-of-war is commonly considered a jellyfish, but in reality, it is a hydrozoan colony. The tentacles hang from the float and may reach a length of more than 75 feet. Each tentacle contains about 750,000 nematocysts. Because of the length and transparency of the tentacles in the water, swimmers are often stung without seeing the animal. Nematocysts may discharge even when the animal is dead and on the beach. The toxin injected is one of the most powerful marine toxins. Local effects are immediate and include intense pain and irritation. The affected area usually has the appearance of deeply erythematous, vesicular, whip-like striations crisscrossing over one another and delineating the pattern of the tentacles on the skin. The lesions may become necrotic, ulcerate before healing, and leave long-lasting, pigmented striae. Systemic reactions include headache, myalgias, fever, abdominal rigidity, arthralgias, nausea, vomiting, pallor, respiratory distress, hemolysis, renal failure, and coma. Death may occur if the area stung is extensive in relation to the size of the victim.1
Of the scyphozoans (true jellyfish), the common purple jellyfish (Pelagia noctiluca) and the sea nettle (Chrysaora guinguecinda) are only mildly toxic. Local skin irritation is the major clinical manifestation. In contrast, the lion’s mane jellyfish (Cyanea capillata), a species found along both North American coasts, is highly toxic. Contact with its tentacles produces severe burning. Prolonged exposure causes muscle cramps and respiratory failure.
Treatment of hydrozoan and scyphozoan stings is based on the same common principles: stopping further envenomation, relief of pain, and treating the systemic effects if present. The most important step is to remove any adherent tentacles. As long as the tentacle adheres to the skin, the nematocysts continue to discharge. The undischarged nematocysts of many species can be inactivated by topical application of vinegar (3% acetic acid), slurry of baking soda, or meat tenderizer (papain) for 30 minutes. Vinegar has been shown to be ineffective and may activate the nematocysts of the Portuguese man-of-war. The area should then be washed with normal saline. Freshwater should not be used because it causes nematocysts to discharge. Any adherent tentacles should be removed with instruments or gloved hands and the wound area should be immobilized. Removal of nematocysts may be difficult. Some experts recommend applying aerosol shaving cream and then shaving off the nematocysts with a safety razor. General supportive measures for local and systemic reactions include oral antihistamines, oral corticosteroids, and oral narcotics for pain. Anaphylaxis may require administration of epinephrine as well as cardiac and respiratory support. Muscle spasms have been treated with calcium gluconate or benzodiazepines given intravenously. There is no antivenin available for Physalia or the other scyphozoans. A specific antivenin is available for stings by the highly venomous and sometimes fatal box jellyfish, Chironex fleckeri, of Australia. It is effective and, if used promptly, can be life-saving. Local dermatitis should be treated with a topical corticosteroid cream.
The anemones and corals (class Anthozoa) found within United States tidal zones are mildly toxic at worst. Sea anemone stings usually occur in shallow water. They produce an almost instantaneous burning sensation, which is followed by intense itching. An area of central pallor frequently appears, surrounded by erythema and petechial hemorrhage. The envenomed area can become edematous and, in severe envenomation, may become ecchymotic and hemorrhagic. The lesion may ulcerate and heal after eschar formation. Milder envenomations usually resolve uneventfully within several days. In the United States, fire corals (Millepora spp) are among the most common cause of mild coelenterate stings. Contact with these sessile creatures results in immediate, intense burning or stinging. Severe pruritus and urticaria that may last for several days follow the pain. Wheals reach maximum size 30 to 60 minutes after contact. Untreated, the wheals flatten over 14 to 24 hours and resolve over 3 to 7 days. The wheals may leave an area of hyperpigmentation, which gradually fades after several months. Hours after contact, a delayed reaction can appear, presenting as papules or hemorrhagic vesicles. At times, an erythema nodosum–like reaction can recur repeatedly over several months.
The stinging ability of stony corals is not well defined but is considered to be of minor significance. Coral cuts, however, can result in serious injury because they combine laceration of tissue, nematocyst venom, persistence of foreign debris in the wound, and secondary bacterial infection. The presentation typically includes a stinging sensation followed by wheal formation and itching. If the wound is untreated, then an ulcer with an erythematous base may form within a few days. Cellulitis, lymphangitis, fever, and malaise are common. Treatment consists of cleaning the wound and irrigation with copious amounts of saline. Foreign particles must be removed, and débridement may be necessary. Seawater provides an excellent inoculum for wound infections. Organisms causing infections include Vibrio species, Erysipelothrix rhusiopathiae, and Mycobacterium marinum. Wounds should be left open. Broad-spectrum antibiotic therapy, particularly tetracycline, has been advocated for children older than 8 years. For children younger than 8 years, cephalexin or trimethoprim-sulfamethoxazole should be used.
Seabather’s eruption is a pruritic, usually benign, dermatitis that is caused by planula larvae of the phylum Coelenterata (Cnidaria). Typically, these larvae possess more than 200 nematocysts. Off the northeast coast of the United States and the coast of Florida, the planula larva of the sea anemone Edwardsiella lineata and the planula larva of the jellyfish Linuche unguiculata, respectively, have been identified as the probable cause. Onset is typically 4 to 24 hours after exposure. The eruption consists of erythematous maculopapules, or wheals with pruritus. Some people have reported a prickling sensation or develop urticarial lesions immediately, while others may be asymptomatic for 3 to 4 days. The duration of symptoms varies from several days to weeks. Children may have high fevers, provoking extensive medical studies for meningitis, sepsis, or fever of unknown origin. Treatment is symptomatic using antihistamines or corticosteroids.2
PHYLUM ECHINODERMATA
Phylum Echinodermata includes starfish, sea urchins, and sea cucumbers. Of the three classes, the Echinoidea, sea urchins, constitute the greatest threat to children. Only 1% to 2% of the known species are poisonous. Of the poisonous species, either hollow venom-filled spines or jawlike organelles called pedicellariae inject venom. The most severe envenomations occur from those species in which the venom is injected by the pedicellariae. The long-spined urchins (eg, Diadema) are usually responsible. Most of the spines are solid and do not possess venom (as do some of the tropical urchins), but the spines, composed of calcium carbonate, are dangerous when stepped on or handled. The spines easily pierce the skin and become lodged deep in the flesh. The spines can penetrate wet suits and sneakers, and may break off in the wound. Penetration is accompanied by intense pain followed by redness, swelling, and aching. Complications include tattooing of the skin, secondary infection, and granuloma formation.
Treatment consists of immersion of the punctured extremity in hot water (40–45°C). All spines should be removed as completely as possible. If spines break off in the wound, débridement should be performed with local anesthetic. Analgesics may be needed for pain. Systemic antistaphylococcal antibiotics should be used if infection develops.3
PHYLUM CHORDATA
Stingrays
Stingrays are the single most important group of venomous fishes, accounting for an estimated 750 envenomations per year in North America. Stingrays are bottom feeders and have a habit of burying themselves in sand or mud. Envenomations usually occur when an unsuspecting swimmer steps on the back of the animal, causing it to hurl its barbed tail upward into the victim as a reflex defense response. Most injuries are confined to the lower extremities, although wounds to the chest and abdomen have been reported. The venom is delivered by a serrated, retropointed, dentinal caudal spine located on the dorsum of the tail. The spine is encased in an integumentary sheath that contains specialized secretory cells. When the barb strikes the victim, it penetrates the skin, rupturing the integumentary sheath over the spine causing the venom to pass along the ventrolateral grooves of the barb into the wound. The venom is a heat-labile toxin that has been shown to contain at least 15 fractions, including serotonin, 5-nucleotidase, and phosphodiesterase. The toxin produces severe local pain, depresses medullary respiratory centers, and interferes with the cardiac conduction system.
Wounds vary in length and are a combination of puncture and laceration. The sting is followed immediately by pain, which spreads from the site of injury and usually reaches its greatest intensity within 90 minutes. Pain and edema are most often localized to the area of injury. The wound often has a jagged edge that bleeds profusely, and the wound edges may be discolored. Discoloration may extend several centimeters from the wound within hours after injury and may subsequently become necrotic if untreated. Syncope, weakness, nausea, and anxiety are common complaints. Generalized symptoms include vomiting, diarrhea, sweating, and muscle fasciculations of the affected extremity. Generalized cramps, paresthesias, hypotension, arrhythmias, and death may occur. However, deaths are rare and usually result from penetrating wounds to the chest or abdomen.4
Treatment at the scene includes wound irrigation with cold saltwater. Irrigation can help remove much of the venom. Bleeding should be controlled with direct pressure. Supplemental fluids and blood products may be necessary. At the site of definitive care, an attempt should be made to remove any remnants of the integumentary sheath, if it can be seen in the wound. The extremity should be placed in hot water (40–45°C) for 30 to 90 minutes. This inactivates the venom and relieves pain. After soaking, the wound should be re-explored. Further débridement can be accomplished and the wound can be loosely closed. Additional pain relief may be achieved with narcotic analgesia. Tetanus prophylaxis should be given as needed.
Scorpaenidae
The family Scorpaenidae includes the zebrafish, the scorpionfish, the stonefish, and the sculpin. Scorpaenidae are generally found in shallow water, around reefs, kelp beds, or coral. All members of the family are nonmigratory and slow swimming, and are often buried in sand. The venom apparatus consists of a number of dorsal, anal, and pelvic spines covered by integumentary sheaths containing venom glands that lie within anterolateral grooves. The venoms are unstable, heat-labile compounds. Envenomation usually occurs when the fish are handled during fishing excursions.
Signs and symptoms vary among the species in degree only. Severe pain at the site of the wound is the primary clinical sign. The wound and surrounding area becomes ischemic and then cyanotic. Paresthesias and paralysis of the extremity may occur. Other signs and symptoms include nausea, vomiting, hypotension, tachypnea, and myocardial ischemia.
Treatment involves irrigating the wound with sterile saline. The injured extremity is then immersed in hot water (40–45°C) for 30 to 60 minutes or until the pain is completely relieved. In addition, narcotic analgesics may be required. The patient should be monitored carefully for cardiotoxic effects and respiratory depression. The only antivenin available is for the stonefish of Australia.
Catfish
The catfish is a popular food and sport fish found throughout the United States. The venom apparatus consists of a number of spines located in the dorsal and pectoral fins. The integumentary sheaths covering the spines contain venom glands. The venoms are unstable, heat-labile compounds. Envenomation usually occurs when the fish are handled during fishing excursions. The injuries often combine puncture and laceration, foreign body reaction, and the local and systemic effects of venom.
The spines inflict a puncture wound or laceration. The spines may become imbedded in the flesh of the victim, causing soft tissue swelling and possibly a cellulitis and foreign body reaction. The venom produces a local inflammatory response characterized by intense pain, edema, local hemorrhage, and tissue necrosis. The wound should be irrigated with sterile saline and then immersed in hot water (40–45°C) for 30 to 60 minutes or until pain is relieved. Narcotic analgesia may be required. The wound should be explored to locate and remove any retained spines. Systemic antibiotics to cover gram-negative organisms are recommended. Wounds may be closed using a delayed primary closure.
TERRESTRIAL BITES AND STINGS
PHYLUM ARTHROPODA
The arthropods make up the largest phylum in the animal kingdom. All arthropods have an ex-oskeleton with jointed appendages. The phylum is divided into two subphyla: the Chelicerata, which includes spiders, scorpions, ticks, mites; and the Mandibulata, which includes insects.
 SPIDERS
SPIDERS
More than 100,000 species of spiders (class Arachnida) are known to exist. All are carnivorous and have fangs and venom that they use to immobilize and kill their prey. The risk of serious bites is small, because in most species, the fangs are too short and fragile to penetrate human skin, and the venom is mild. Contrary to common belief, most spiders are harmless and shy.
Laxosceles (Brown Recluse Spider)
Two species of Loxosceles have caused envenomation in the Western Hemisphere. Loxosceles reclusa is found primarily in the southern and midwestern states. L. laeta is found in South and Central America. These small spiders (1–1.5 cm long) are characterized by a brown violin-shaped mark on the dorsum of the cephalothorax. They establish nests indoors, especially in closets and basements, and bite when disturbed. The venom contains a cytotoxic factor related to hyaluronidase.
Initially, the bite appears innocuous, but the site can become painful within hours. Because the bite is often unnoticed at first, there is sometimes a delay in seeking medical attention. The spectrum of reaction ranges from minor local reaction to severe necrosis. Mild to moderate pain, generally 2 to 8 hours after the bite, characterizes the local reaction, which varies with the amount of venom injected. At the site of the bite, erythema develops with a central blister or pustule. A bulla may develop, and concentric areas of ischemia and erythema may appear. During the ensuing 24 to 48 hours, the lesion becomes cyanotic and ulcerates. The necrotic ulcer slowly expands and can reach 10 to 20 cm in diameter during the subsequent weeks to months. Scar formation is rare if there is no clinical evidence of necrosis within 72 hours of the bite. Systemic reaction is usually noted 24 to 48 hours after the bite, and includes fever, chills, malaise, weakness, nausea, vomiting, joint pain, morbilliform eruption with petechiae, intravascular hemolysis, hematuria, and renal failure.6,7
Unless the spider is available for identification, definitive diagnosis cannot be made. Envenomation outside of endemic areas is rare.8 Currently there is no specific serologic, biochemical, or histologic test to diagnose envenomation approved for use in humans. Serious complications are rare, and the vast majority of victims will heal with supportive care. If large areas of necrosis have become demarcated, surgical excision and skin grafting may be required, but grafting is usually not needed. Administration of steroids or heparin does not seem to alter the extent of necrosis. The use of dapsone should be limited to adults with proven brown recluse bites because of the possibility of methemoglobinemia. Antivenin is not commercially available. If systemic manifestations occur, vigorous supportive care is needed, as well as laboratory monitoring for evidence of hemolysis and renal failure.7
Latrodectus (Black Widow Spider)
Latrodectus mactans is the leading cause of death from spider bites in the United States. The female is shiny black with a brilliant red hourglass mark on the abdomen. The average width of the abdomen is 6 mm, and the overall length (with legs extended) is 40 mm. The male may have a similar mark, but is not a threat because it is only one-quarter the size of the female, and its fangs cannot penetrate human skin. The webs are usually found in out-of-the-way places such as vacant rodent burrows, hollow stumps, or dark corners of barns, privies, and garages. The female is not aggressive unless guarding her egg sac or provoked. The venom is a complex protein that includes a neurotoxin that stimulates myoneural junctions, nerves, and nerve endings.
The bite of the female black widow spider resembles a pinprick, sometimes with slight swelling. Immediately after the attack, the victim experiences local sharp, throbbing pain that increases in intensity for several hours, by which time vascular spread has occurred. One to 8 hours after the bite, cramping pain is felt in the abdomen, flanks, thighs, and chest. Nausea and vomiting are often reported in children. Respiratory distress is not unusual. Chills, urinary retention, and priapism have been reported. There is an overall 4% to 5% mortality rate, with death resulting from cardiovascular collapse.
Symptoms generally are more severe in children and the elderly. A child who presents with severe pain and muscle rigidity after a spider bite should be considered a potential Latrodectus bite victim.9 In children who weigh less than 40 kg, treatment with Latrodectus antivenin (Merck), if available, should be administered as soon as a bite is confirmed. After skin testing for sensitivity to horse serum, the usual dose is 2.5 mL (1 vial) in 50 mL of saline administered by slow intravenous injection. For children who weigh more than 40 kg, administration of antivenin is not as urgent, but indications for its use include patients under age 16 years, respiratory difficulty, or marked hypertension. Antivenin is usually effective within 30 minutes and may be repeated once (maximum dose: 2 vials) within 2 hours if necessary. Serum sickness is a possible side effect but is uncommon. Muscle relaxants such as diazepam have been advocated, but they are variably effective and the effects are short lived. Analgesia may be achieved with morphine. A monoclonal antibody fragment has been used in mice to neutralize alpha-latrotoxin, a neurotoxic component of the black widow spider venom.9,10
Tarantulas and Other Spiders
Tarantulas, although fearsome in size and appearance, do not bite unless provoked. The venom is mild, and envenomation is not a problem. The wolf spider (Lycosa spp) and the jumping spider (Phidippus spp) also have been implicated in bites. Like the tarantula, they have a mild venom that causes only local reactions. Bites from all three of these spiders should be treated with local wound care.
 SCORPIONS
SCORPIONS
There are many scorpion species that accidentally sting humans. Only a limited number are dangerous to man. In Mexico, for example, where scorpions have been responsible for 82% of 24,627 deaths from poisonous animals over a 10-year period, more than 80% of these fatalities have occurred in children under age 5 years, and 94% in children under age 10 years. In the southwestern United States, the bark scorpion, or Centruroides sculpturatus (C. exilicauda) is the only native, lethal inhabitant. The animal has two pinching claws and a tail or pseudoabdomen that ends in a telson. The telson houses a pair of poison glands and a stinger. Scorpions are nocturnal; during the day they may crawl into sleeping bags and unoccupied clothing.
The scorpion’s venom contains a local cytotoxin and a neurotoxin that also have hemolytic properties. The general neurotoxicity is excitatory, affecting the autonomic and skeletal neuromuscular system. Following a sting there is an immediate sharp pain. Common symptoms include restlessness, hyperactivity, roving eye movements, and respiratory distress. Other associated signs may include convulsions, drooling, wheezing, hyperthermia, cyanosis, and respiratory failure. Pulmonary and gastrointestinal hemorrhage may occur. Death occurs because of respiratory paralysis, pulmonary edema, or intractable hypotension and shock. A history of a sting may not be elicited, making the diagnosis difficult. There is no laboratory test for confirmation of envenomation.
Treatment should be initiated as soon as possible. General supportive care is critical. Cryo-therapy of the site of sting has been advocated to reduce swelling and local induration. Continuous intravenous benzodiazepines may be necessary up to 24 hours to mitigate symptoms in severe envenomation.11 In Central Arizona, a locally manufactured scorpion antivenin was available for severe envenomation for many years, but production ceased in 2001, depleting stockpiles of antivenin in 2004, and leading to greater numbers of admissions to pediatric intensive care units.12,13
 TICKS
TICKS
Both tick bites and tick-borne diseases have become more frequent, especially along the East Coast of the United States. Ticks are blood-sucking ectoparasites in all of their stages, and they can be recognized easily by the organization of their mouthparts and body. They are subdivided into two major groups: (1) the argasids, or soft ticks; and (2) the ixodids, or hard ticks.
Ticks are widespread in nature and may transmit numerous infectious diseases including spirochetes, viruses, rickettsiae, bacteria, and protozoa. In addition, they cause mechanical injury at the bite wound. Occasionally, they may release toxic substances of their own, as in the case of the tick-induced paralysis. Ticks attach to their host by their highly specialized mouth-parts, and they may engorge themselves with blood for days or weeks before dropping off. During this period, they may become so enlarged that they resemble a pedunculated wart or fibroma. The North American deer tick, Ixodes scapularis, is minute and may go unnoticed. After a tick bite and detachment, a granuloma may form at the bite wound. This generally resolves during the subsequent few months.
Tick paralysis most often is reported in children, in whom almost all fatalities occur. Approximately 20 species of ticks, in the genera Dermacentro, Amblyomma, Rhipicephalus, Ixodes, Ornithodoros, Haemaphysalis, and Argas, have been implicated. In North America, tick paralysis in humans is usually associated with species of Dermacentor and Amblyomma. Symptoms may begin with motor weakness and progress as an ascending, flaccid, motor paralysis, which often is mistaken for Guillain-Barre syndrome or poliomyelitis. Sensory involvement is uncommon. Symptoms of paralysis may become evident 4 to 7 days after the bloodsucking starts, although symptoms occurring after only 1 day have been reported. The ascending paralysis may progress in a matter of hours to involve the cranial nerves. Patients may die of respiratory failure or aspiration pneumonia. Laboratory data, including cerebrospinal fluid are usually normal, but lymphocytic pleocytosis has been reported. It is believed that the gravid female tick secretes in her saliva a neurotoxin that blocks the release of acetylcholine at neuromuscular junctions. If not too far advanced, removing the tick is associated with prompt, and often dramatic, reversal of the symptoms.14 Patients are usually afebrile. A tick may be found after careful examination. It is important to search the scalp, axilla, and pubic regions to locate the ticks.
Ticks normally should be removed manually by gentle traction using blunt forceps or tweezers. The tick should be grasped as close to the skin surface as possible and pulled upward with a steady, even pressure. A twisting or jerking motion may cause the mouthparts to break off. The entire tick, including the mouthparts, must be removed. If the mouthparts are left behind, they usually cause a severe granulomatous lesion that may not heal for months. Squeezing or crushing the body of the tick may facilitate inoculation of infective agents into the host. Ticks can be controlled with synthetic permethrin or pyrethroid sprays. Dogs should wear tick collars that are changed every 30 to 60 days. Clothing can be impregnated with tick repellents such as dimethylphthalate, diethyltolu-amide, or indalone. Dogs should be inspected every day to prevent infesting the home.
 CENTIPEDES
CENTIPEDES
Centipedes (class Myrapoda) are wormlike arthropods possessing many repetitive body segments, each of which has one pair of segmented legs. Immediately below the mouth are modified legs of the first body segment (ie, the max-illipeds), which are powerful poison claws used to attack and kill prey. Although centipedes are greatly feared for their appearance, they rarely bite. However, bites can be extremely painful. The toxin causes only local reaction. The pain usually diminishes rapidly and may require nothing more than a cold compress and local wound care. Injection of local anesthetic at the wound site is used for extreme pain. More generalized reactions, such as nausea, vomiting, and dizziness, are rare. General supportive care is warranted in these cases. A single death in a 7-year-old child has been reported.
 INSECTS
INSECTS
The stings of bees, hornets, yellow jackets, wasps, and fire ants introduces a venom that in nonsensitized individuals causes immediate pain, induration, and redness lasting several hours or longer. Serious allergic reactions including death may occur, especially in those who are previously sensitized. Hymenoptera are responsible for 50% of human deaths from venomous bites and stings. Although higher levels are reported in adults than in children, only approximately 8% develop an allergic reaction following a repeat sting. It is not clear whether subsequent experiences are associated with progressively more severe reactions. Stings may cause a profound systemic reaction with nausea, vomiting, hypotension, loss of consciousness, and death. However, in most cases, individuals who have had local reactions continue that pattern with each sting. Systemic reactions occur more frequently in individuals who have had multiple stings.
Bees and Wasps
The venoms of the bee, hornet, yellow jacket, and wasp contain protein antigens that can elicit an immunoglobulin (IgE antibody) response in those persons who are stung. In addition, venoms contain various biogenic amines, phospholipase, phosphatase, and hyaluronidase. The barbed stinger of the bee remains in the victim’s skin. The wasp, in contrast, may sting many times. Reactions may be grouped by severity. Local reaction to a sting results in pain, erythema and swelling. Large reactions consist of more extensive erythema and edema. Systemic allergic reactions may be grouped using the following system15:
Group I: generalized urticaria or erythema, itching, malaise, or anxiety
Group II: angioedema or two or more of the following: chest or throat tightness, nausea, vomiting, diarrhea, abdominal pain, dizziness
Group III: dyspnea, wheezing, or stridor, or two or more of the following: dysphagia, dysarthria, hoarseness, weakness, confusion, or feeling of impending disaster
Group IV: hypotension, collapse, loss of consciousness, cyanosis, incontinence
The barbed honeybee stinger with venom sac is avulsed and often remains in the victim’s skin. It must be removed if possible; delays in removal are likely to increase the dose of venom received. Treatment is based on the severity of the allergic reaction. Local reactions require only cold compresses at the site of sting. More severe local reactions are treated with diphenhydramine or loratadine orally for several days and oral steroids are often added. Group I through group III reactions are treated with subcutaneous injection of epinephrine 1:1000 (0.01 mL/kg, 0.3 mL max). It may be necessary to repeat epinephrine twice at 10-minute intervals to arrest the symptoms, followed by oral antihistamines. H2-blockers such as ranitidine or famotidine may provide additional benefit for group I and II patients. Group II and group III patients should be admitted for observation for 24 hours.16 Group IV reactions may require intubation if upper-airway obstruction is present. Hypotension should be treated with a fluid bolus of saline or lactated Ringer solution. Intravenous epinephrine may be indicated if hypotension fails to respond to subcutaneous epinephrine and fluid bolus.17 In addition, intravenous steroids are indicated.
Children who have had a group II, III, or IV reaction merit follow up by an allergist, if possible and should be considered for hyposensitization. Because immunotherapy may reduce the risk of anaphylaxis to approximately 3%, many advocate that venom-sensitized patients undergo immunotherapy. Allergic individuals who have not had immunotherapy should be advised to carry an anaphylaxis emergency treatment kit. Parents should receive information regarding the avoidance of situations and behaviors that would attract stinging insects.
Ants
Ant stings frequently occur in the southern United States and are caused by various species of fire ants of the genus Solenopsis. Multiple stings and mass attacks can cause severe reaction. Harvester ants (ie, Pogonomyronex) attack humans readily and cause painful stings. The venom differs from the venom of other Hymenoptera in that it is an alkaloid with a direct toxic effect on mast cells. There is no cross-reactivity with other members of the order. Severe and fatal reactions have been reported in farm animals; fortunately, these are rare in humans. The fire ant bites with well-developed jaws and then uses its head as a pivot to inflict multiple stings. Immediately after a sting, an erythematous wheal appears, which vesiculates after a few hours. A pustule forms within 24 hours; in several days to a week this ruptures, encrusts, and finally forms a small fibrous nodule or scar. Pain can persist for 3 to 10 days. Systemic reactions can occur, especially if there are multiple stings. Treatment is symptomatic. Local care, such as ice applied to the reactive area, and frequent cleansing of the lesions to prevent secondary infection is all that is usually required. Systemic therapy does not appear to prevent pustule formation. Antihistamines are useful for pruritus. Systemic reactions are rare and should be treated similarly to other Hymenoptera reactions.
PHYLUM CHORDATA
 VENOMOUS SNAKEBITES
VENOMOUS SNAKEBITES
Although only 15% of the 120 snake species found in the United States are venomous, poisonous snakes bite an estimated 8000 persons annually. Predictably, the pediatric population, especially males ages 5 to 19 years, accounts for a disproportionately large number of these victims, and males are more likely than females to sustain bites that require antivenin. The highest incidence occurs in the Southeast and Southwest between April and October. If treated properly and early, these injuries have a remarkably low mortality and morbidity. Only 10 to 15 deaths are reported per year, but the morbidity in limb dysfunction and other complications, though unknown, is undoubtedly higher.
Snake venoms are an evolutionary adaptation for obtaining food. As such, venoms are complex mixtures of potent enzymes, primarily proteinases and low-molecular-weight peptides that possess toxic properties. Certain components are intended to immobilize prey, whereas other components are digestive enzymes that penetrate throughout the prey’s tissues. Crotalid venom is often a combination of necrotizing, hemotoxic, neurotoxic, nephrotoxic, and/or cardiotoxic substances. Elapid venom contains neurotoxic and cardiotoxic components. Mojave rattlesnake venom contains primarily neurotoxic compounds that are related to phospholipase A and bind the nicotinic acetylcholine receptors, thus preventing the depolarizing action of acetylcholine. Proteolytic enzymes aided by hyaluronidase cause much of the local tissue destruction. Many of the venoms induce increased endothelial permeability and venous pooling, thus decreasing intravascular volume. Transient hemoconcentration may be present as a result of plasma extravasation. Respiratory failure may occur because of pulmonary edema. Hemotoxic effects include hemolysis and fibrinolysis. Thrombocytopenia is frequently present. Elapid snake venoms may cause considerable necrosis in addition to exhibiting neurotoxicity.
The venom enzymes typically found in crotalid and viperid venoms are esterases with procoagulant and bradykinin-releasing activities. They cause intravascular clotting either by a thrombinlike action (pit vipers) or by activation of factor X (eg, Russell viper). The thrombinlike activity of many North American pit viper venoms differ, however, from that of thrombin in that other clotting factors are not usually activated and the resulting microclots are friable, unstable, and readily lysed by the activation of the plasminogen–plasmin system. This results in defibrination and a clinical picture resembling disseminated intravascular coagulation in which the defibrinating agent is presumed to be thrombin. Snake venom procoagulants, however, do not usually cause platelet aggregation, nor do they activate and destroy factors V and VIII. Inhibition by heparin is incomplete or does not occur. The defibrination produced is readily corrected by antivenin.
Pit Vipers
The poisonous snakes indigenous to the United States are members of the Crotalidae (pit viper) or Elapidae families. The Crotalidae contain three genera: Crotalus, or large rattlesnakes, with about 30 species including the Eastern and Western diamondback, timber, prairie, and pacific rattlesnakes; Sistrurus, or ground rattlers, which include the massasauga and the pygmy rattlesnake; and Agkistrodon, or moccasins, which include the cottonmouth and copperhead. The pit vipers have several characteristic features that distinguish them from nonvenomous snakes: (1) the pit from which their name originates contains heat-sensitive organs that assist in the localization of prey and are located on each side of the head between the eye and nostril; (2) their pupils are elliptical and vertically oriented in contrast to the round pupil of harmless snakes; (3) they have two, 5- to 20-mm-long curved fangs or hollow maxillary teeth that are folded posteriorly against the palate and advance forward when the pit viper strikes; in larger snakes, they may be spaced as widely as 3 cm; (4) a relatively more triangular head than that of most nonvenomous snakes; and (5) a single-row scute, or scales, on the ventral portion, caudad to the anal plate, as opposed to the double-row seen in nonpoisonous snakes. Physicians who might treat snakebite victims should become familiar with the particular species in their areas.
The effects of a pit viper bite depend on the characteristics of both victim and snake. The victim’s size and state of health influence how the toxins are tolerated; the characteristics of the wound inflicted by the bite and its location affect venom absorption. Fang penetration of a vessel or subfascial compartment ensures a more rapid absorption and serious systemic effects. Likewise, a bite on the head, neck, or trunk (3% of snakebites) hastens systemic absorption. Approximately one third of snakebites involve the upper extremity and cause higher long-term functional morbidity than do lower-extremity wounds.
The snake’s size, the amount of venom injected, and the potency of the particular species’ venom also influence the bite’s outcome. Thus, long, healthy fangs or full stores of venom add to its toxicity.
Local pain after a crotalid envenomation is typically intense. A sensation of burning occurs almost immediately (within 5 to 10 minutes). The pain increases as edema develops and is dependent on the size of the venom inoculate. Victims of a significant rattlesnake bite often complain within minutes of perioral numbness and paresthesias extending to the scalp and periphery. These paresthesias may be accompanied by a metallic taste in the mouth. Nausea, vomiting, weakness, chills, sweating, and syncope are also frequent. A copperhead or pygmy rattlesnake envenomation usually produces less-localized symptoms, and systemic consequences are often minimal, unless the victim is a small child, there are multiple bites, or a larger-than-average snake is involved.18 The effects of the water moccasin’s envenomation are more variable. Severe pain and swelling are absent after Mojave rattler bites, although, as in other crotalid bites, the patient may complain of pares-thesia in the affected extremity. Within several hours, neuromuscular symptoms, such as diplopia, swallowing difficulty, lethargy, nausea, and progressive weakness develop.
The wound should be inspected for fang punctures, and if two are present, the distance between them should be noted. In general, less than an 8 mm inter fang distance suggests a small snake; 8 to 12 mm suggests a medium-sized snake; and greater than 12 mm suggests a larger snake. Fang wounds by small snakes such as the pygmy rattler may be extremely subtle. There may be bloody serosanguineous fluid dripping from the fang punctures. Depending on the time to presentation, the fang marks may be hidden within hemorrhagic blebs and edema. Occasionally, only one puncture or two simple scratches are present. In these wounds, there is still the potential for envenomation. However, 10% to 20% of known rattlesnake strikes do not inject venom. Other etiologies for puncture wounds also must be kept in mind, notably rodent bites or thorn wounds. Nonpoisonous snakes sometimes leave an imprint of their two rows of teeth, but the wounds lack fang puncture marks.
Progressive swelling usually develops over the next 8 hours and may continue to some degree for an additional 24 hours, depending on the size of the inoculum. In a severe diamondback rattlesnake bite, an entire extremity may be swollen within 1 hour. The swelling looks impressive and the skin may feel tense and look shiny. Subfascial compartmental pressures are generally not increased, and compartment syndromes requiring fasciotomy are rare. Bluish discoloration of the bitten part is common, and ecchymoses, blebs, and blisters may develop. Local ecchymoses and vesicles usually appear within the first few hours, and, commonly, by 24 hours hemorrhagic blebs are present. Lymph node enlargement or lymphadenitis also may become apparent. Without appropriate therapy, these local manifestations progress to necrosis and may extend throughout the bitten extremity. However, local necrosis may occur even in optimally treated patients.
Other systemic signs are dependent on the species and the amount of venom injected. Tachycardia and decreased capillary perfusion may be seen. In severe cases, hypotension and shock develop. Increased respiratory effort may be the result of metabolic acidosis or from pulmonary edema, and may progress to respiratory failure. Oliguria may be secondary to shock or renal failure. Hemoglobinuria and hematuria are the result of the bleeding diathesis, which can develop. Hemoglobinuria cannot be the result of the bleeding problem alone. Neurologic signs include fasciculation, weakness, paralysis, and convulsions.
Treatment Therapy for poisonous snakebites remains controversial. Because snakebites are uncommon, few physicians have extensive experience, and controlled studies are infeasible. In spite of this, certain tenets of management are not in question. As in all medical emergencies, the airway, breathing, and circulation of the patient must be assessed and guaranteed before attending to the snakebite. The first priority of prehospital care of the snakebite victim is rapid transport to a medical facility.
It is important to reassure the patient and avoid agitation. The affected extremity should be stripped of any jewelry or clothing and immobilized in a position of function below the level of the heart. Tight tourniquets are not recommended. However, a constriction band that obstructs lymph and venous flow can be valuable when a transport longer than 30 to 60 minutes is anticipated. The band should be at least 2 cm wide, made of nonstretchable material, and placed 5 to 10 cm proximal to the wound. Only the lymphatics and superficial veins need to be occluded, and good distal arterial pulses should be preserved (band loose enough to admit a finger). Observation for adequate perfusion is necessary because of progressive edema; the constriction band should be shifted to remain proximal to the swelling. The band must be applied initially within 1 hour of a pit viper bite. (Note that constriction bands are not recommended in coral snake envenomation.)
Incision and suction cannot be recommended. A study of a suction device (Sawyer Extractor pump) in a simulated snakebite in human volunteers demonstrated that the pump removed bloody fluid but almost no mock venom, and is unlikely to reduce the total body burden in the field.19 In the rare situation in which skilled personnel and supplies are at the scene and a long transport is expected, it is reasonable to allow one or two attempts at intravenous access. Many also suggest capturing or killing the snake for later verification; however, an inexperienced person should be extremely cautious and not risk a second bite. If the snake arrives in the emergency department or office, treat it with respect. Snakes that appear to be dead have been known to bite, and decapitated snake heads can bite reflexively for up to 1 hour.
In the past, the use of ice to cool the bitten area was advocated. However, cryotherapy should never be used in snakebite because frostbite is easily produced in a limb with circulation already impaired by the action of the venom. Cooling does not slow the action of the venom. Recently, the use of electric shock therapy has received a great deal of publicity in the lay press. The use of high-voltage, low-current shocks in experimental studies has failed to demonstrate any beneficial effects and should not be used.20
Following arrival in the emergency department the key steps to management of snakebite include: (1) establish a baseline of physical findings and physiologic parameters; (2) grade the level of envenomation (see Table 122-1); (3) administer antivenin if indicated; and (4) provide other supportive and therapeutic measures.
A brief history should be obtained and an initial physical examination including vital signs, an inspection of the bite site for fang and/or tooth marks, and evaluation of current neurologic status should be done. Next, the circumference of the injured extremity at the leading point of edema and 10 cm (4 inches) proximal to this level should be measured every 30 minutes for 6 hours and then at least once every 4 hours for a total of 24 hours. If the history and physical examination on arrival in the emergency department are consistent with a venomous snakebite, immediate laboratory evaluation (detailed below) and intravenous access are indicated. Aggressive supportive medical care must be available if signs of major system dysfunction are present. Any prehospital care (eg, extremity immobilization) should be rechecked. If an occluding tourniquet is present, it should be removed after placing a more proximal constriction band, staying well prepared to respond to a systemic release of venom.
Table 122-1. Crotalidae (Pit Viper) Envenomation Grading System (AAPCC)
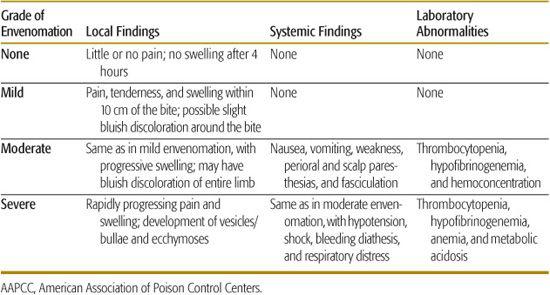
Therapy is based on the clinician’s overall grading of venom toxicity. Local and systemic manifestations, as well as laboratory findings, weigh heavily in this judgment. A complete blood count, coagulation studies, platelet count, urinalysis, and blood crossmatching should be obtained on all patients with suspected venomous snakebite. In moderate or severe poisoning, serum electrolytes, blood urea nitrogen, creatinine, fibrinogen, and arterial blood gases are indicated because of the findings described below. The laboratory studies may need to be repeated every 6 hours to ensure that no significant changes occur. The clinical pattern may change dramatically as the venom’s effects unfold. Frequent reassessment is crucial.
The Scientific Review subcommittee of the American Association of Poison Control Centers has suggested a grading system. The grading system applies only to pit viper bites (Table 122-1).
Antivenin is highly effective in the management of crotalid snakebite. The currently available antivenin is CroFab (Crotalidae Polyvalent Immune Fab Ovine: Protherics, Inc.), which contains purified Fab fragments specific to pit viper species. An equine IgG antivenin (Antivenin Crotalidae Polyvalent, Wyeth Laboratories), used in the past for rattlesnake, water moccasin, and copperhead envenomations, is highly antigenic. The purified Fab product is safe in children as well as adults, and is as efficacious as the older IgG antivenin, but is associated with fewer allergic reactions, although the shorter half-life of the Fab antivenin may allow recurrence of venom effects. CroFab is indicated for progressive venom injury, including worsening local injury, coagulopathy, or systemic effects. Early use within 6 hours of snakebite is recommended to prevent or correct abnormalities that result from envenomation.21-24
Wound care includes irrigation, cleansing, a loose dressing, and tetanus prophylaxis if the patient is judged to lack immunity. The affected extremity should be maintained just below the level of the heart and in a position of comfort. Cotton padding between swollen digits is useful. As in any animal-inflicted wound, secondary infection is a risk. Broad-spectrum prophylactic antibiotics may be indicated. Analgesics for pain should be given. Surgical excision of the wound, routine fasciotomy, and application of ice are not indicated. Fasciotomy should be reserved for the very rare case of a true compartment syndrome. Proteolytic enzymes or inappropriate therapy, not compartmental pressure, usually cause necrosis. Superficial débridement may be required at 3 to 6 days. Physical therapy is beneficial during the healing phase.
The major goal of supportive care is correction of the intravascular volume depletion that results from increased venous capacitance, interstitial edema, and hemorrhagic losses. Moderate or severe envenomation requires placement of two intravenous catheters for separate but simultaneous antivenin therapy and volume replacement. Shock usually develops between 6 and 24 hours after the snakebite but may present within the first hour in severe envenomation. Signs of hypovolemia deserve aggressive therapy. Central vascular monitoring and accurate urine output measurements are desirable for optimal therapy. Normal saline or lactated Ringer solution (20 mL/kg), followed by fresh whole blood or other blood components, frequently corrects the hypovolemia. Vasopressors are usually needed only transiently in the most severe cases. A bleeding diathesis is best managed with fresh whole blood, or blood-component therapy, in addition to antivenin. With life-threatening bleeding, platelets and cryoprecipi-tate should be considered. Abnormal clotting tests, including fibrinogen concentration and platelet and blood counts, should be reevaluated every 4 to 6 hours. Respiratory support also is frequently required when shock has developed. Renal failure is another potential problem in this setting.
Coral Snakebite
The family Elapidae, which includes cobras and mambas, is represented by two species of coral snake, the eastern (Micrurus fulvius) and the Arizona (Micruroides euryxanthus). M. fulvius is responsible for the majority of human envenomation and is found in most of the southeastern states. M. euryxanthus is indigenous only to Arizona and New Mexico. The relatively passive coral snake is responsible for only 10 to 15 snakebite cases per year in the United States. Coral snakes are 2 to 3 feet long and do not share the pit viper’s distinctive physical characteristics. Unlike nonpoisonous snakes, the coral snake does have two small maxillary fangs. A small amount of highly toxic venom is produced. The snout of the coral snake is always black and is followed by brightly colored transverse bands of yellow, red, and black.
Symptoms seen after coral snakebite differ from those seen after the bite of pit vipers. The signs and symptoms reflect the neurotoxic nature of the venom. The bite may have 1 or 2 punctures, at most 7 to 8 mm apart, as well as other small teeth marks, as opposed to the one or two fang marks of pit viper bites. There is usually only mild pain and little, if any, swelling. Local necrosis does not occur. Systemic symptoms are delayed and occur over several hours. Initial symptoms include generalized malaise and nausea, vomiting, and paresthesias in the bitten part. Fasciculations and weakness develop insidiously. The patient may complain of diplopia and may have difficulty talking or swallowing. Physical examination reveals bulbar dysfunction and generalized weakness. Paralysis of skeletal muscles follows, beginning with the limb girdles and progressing distally. Respiratory failure may ensue. Paralysis persists for 3 to 4 days followed by recovery, although minor effects may linger for several weeks.
An elapid (Micrurus fulvius) antivenin (Wyeth) went out of production in 2006. Other elapid antivenins are under investigation. There is no antivenin available for the Arizona coral snake (Micruroides euryxanthus). Additional supportive care measures as outlined in the management of pit viper bites should be followed.25
Exotic Snakes
The clinician confronted with an exotic snakebite or a clinician inexperienced in snakebites should consult a local medical herpetologist or a regional poison control center of the American Association of Poison Control Centers (1-800-222-1222). Report all illegally possessed reptiles to the police or to the appropriate fish and game agency.
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


